A clinical survey of laryngectomy patients to detect presence of the false perception of an intact larynx or the
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2013; 34(01): 3-7
DOI: DOI: 10.4103/0971-5851.113394
Abstract
Hypothesis: The Phantom larynx phenomenon (the false perception on an intact larynx in a laryngectomee) exists and is an important issue in the post-laryngectomy rehabilitation of such patients. Objectives: The phantom limb phenomenon has been described after amputation of a limb or other parts of the body. Amputation or removal of any part is usually associated with a global feeling that the missing part is still present. We undertook this study to identify whether a phantom larynx phenomenon actually exists in laryngectomees. We also aimed to elicit its association with the duration following surgery. Patients and Methods: We did a clinical survey of 66 post-laryngectomy patients (30-80 years of age). Twenty-two of these patients were assessed within 6 months following surgery, whereas 44 patients were assessed at least 6 months later. A questionnaire containing 11 questions was served to these laryngectomees pertaining to false perception of persistent laryngeal functions and adaptation to the post-laryngectomy status. Results: All patients showed an evidence of a phantom larynx phenomenon. In the majority of these patients, it persisted even after 6 months following surgery. There was no significant difference in the two groups (less than or more than 6 months) except for one question pertaining to occlusion of stoma for speech (77% vs. 29%). False perception of nasal breathing (59% and 43%) and olfactory sensation (63% in both groups) were the most common. Conclusion: Phantom larynx phenomenon following laryngectomy exists and may cause anxiety and poor rehabilitation among patients. Education and rehabilitation with regards to such a phenomenon is therefore needed in all patients.
Keywords
Laryngectomy - phantom larynx phenomenon - phantom limb - post-laryngectomy rehabilitation - questionnairePublication History
Article published online:
20 July 2021
© 2013. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Hypothesis:
The Phantom larynx phenomenon (the false perception on an intact larynx in a laryngectomee) exists and is an important issue in the post-laryngectomy rehabilitation of such patients.
Objectives:
The phantom limb phenomenon has been described after amputation of a limb or other parts of the body. Amputation or removal of any part is usually associated with a global feeling that the missing part is still present. We undertook this study to identify whether a phantom larynx phenomenon actually exists in laryngectomees. We also aimed to elicit its association with the duration following surgery.
Patients and Methods:
We did a clinical survey of 66 post-laryngectomy patients (30-80 years of age). Twenty-two of these patients were assessed within 6 months following surgery, whereas 44 patients were assessed at least 6 months later. A questionnaire containing 11 questions was served to these laryngectomees pertaining to false perception of persistent laryngeal functions and adaptation to the post-laryngectomy status.
Results:
All patients showed an evidence of a phantom larynx phenomenon. In the majority of these patients, it persisted even after 6 months following surgery. There was no significant difference in the two groups (less than or more than 6 months) except for one question pertaining to occlusion of stoma for speech (77% vs. 29%). False perception of nasal breathing (59% and 43%) and olfactory sensation (63% in both groups) were the most common.
Conclusion:
Phantom larynx phenomenon following laryngectomy exists and may cause anxiety and poor rehabilitation among patients. Education and rehabilitation with regards to such a phenomenon is therefore needed in all patients.
INTRODUCTION
Surgical treatment of advanced laryngeal and hypopharyngeal cancers often requires a total laryngectomy (TL), resulting in a permanent tracheostomy and potential difficulties with a patient's speech, communication, and swallowing. The “Phantom limb” phenomenon has been described after amputation of a limb or other parts of the body. Amputation or removal of any part is usually associated with a global feeling that the missing part is still present. Phantom sensations of other internal organs (bladder, rectum, stomach, and genitalia) have also been reported in literature.[1] The interruption of the afferent input to the brain from the “external organs” leads to “phantom organs,” whereas that from “internal organs” leads to the experience of “phantom sensations.” A recently published study looked at cutaneous sensations of intact larynx following TL.[2] The study concluded that a phantom larynx phenomenon does appear to occur after TL and as many as 69% patients, either had a subjective sensation of phantom or a positive response to cutaneous stimulation. We wanted to find out whether such a phenomenon actually exists clinically.
The presence of a phantom larynx phenomenon can potentially be an important cause of delayed rehabilitation of these patients. We feel that it may also cause anxiety and depression among these patients. Current literature has evidence to suggest that TL leads to significant anxiety and depression and hence poor quality-of-life among survivors.[3] We believe that the “phantom larynx” phenomenon is an important cause of such psychological problems, and addressing this problem would be beneficial to all laryngectomees. We therefore conducted a clinical survey of post-laryngectomy patients using a questionnaire, asking questions pertaining to false perceptions of an intact larynx.
Concept of “phantom larynx”
The “Phantom limb” phenomenon occurs after amputation of limb or any other part of the body. The theory behind the development of a phantom organ is that if a part of the somatosensory cortex has no input, then the cortical map reorganizes itself in such a manner that the unaffected part of the cortex represents a different part of the body surface. This concept is known as “cortical reorganization.” The data on motor homunculus of the human brain are based on neurosurgical studies of electrical stimulation of the awake human brain carried out by Penfield, et al. in the 1930s and 1940s.[4] In Penfield and Rasmussen's work on the control of speech, they described a sequential dorsoventral organization for the lips, jaw, tongue, and pharynx, respectively, on the human motor cerebral cortex.[5] However, they were unable to reliably localize the motor area for vocalization and noted that its representation overlaps that of lips, jaw, and tongue movement. There is evidence today from neuroimaging data that a specific “larynx and phonation” area exists in human motor cortex.[6] One recent study looked at the cutaneous sensations of an intact larynx following TL.[2] In this study, the subjective sensation of “phantom larynx” was charted and a phantom phenomenon was elicited by cutaneous stimulation of neck and face. They concluded that a “phantom larynx” phenomenon exists and as many as 69% of patients had evidence of either a subjective sensation of phantom larynx or a positive response to cutaneous stimulation. But there has been no clinical evidence or study looking at patient experiences and impact of such a phantom phenomenon on post-laryngectomy rehabilitation.
Hypothesis
Phantom larynx phenomenon (false perception on an intact functioning larynx) exists and is an important problem in post-laryngectomy rehabilitation.
PATIENTS AND METHODS
Our aim was to investigate the clinical existence of “phantom larynx” phenomenon or false perception of an intact larynx following laryngectomy surgery and to know its incidence in early post-operative period as well as in long-term follow-up. The study population included 66 post-laryngectomy patients aged between 30 and 80 years. There were 59 males and seven female patients. All patients had undergone either a total or near TL for laryngeal or hypopharyngeal cancer. Sixty-four patients had undergone a TL, whereas two patients had undergone a near TL. Sixty-two patients had tracheoesophageal speech using speech prosthesis, two patients had tracheoesophageal speech using the mucosal shunt created by near TL, and two patients had esophageal speech. All patients had received pre- and post-operative thorough speech and swallowing counseling and therapy. Only two patients had received olfactory rehabilitation post-operatively. A questionnaire containing 11 questions was served to these patients. All questions were pertaining to the false perception of persistent laryngeal functions and adaptation to the post-laryngectomy status [Table 1].
Table 1
Phantom larynx questionnaire with explanation of relevant phantom association
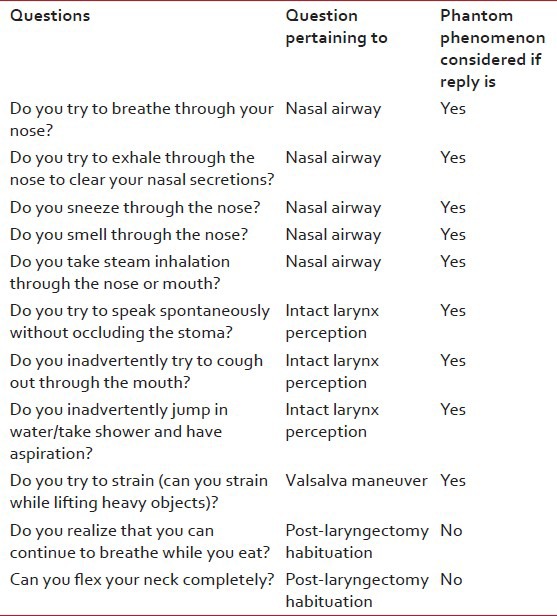
Phantom larynx questionnaire
The questionnaire was framed considering the fact that laryngectomy has a significant impact on speech, communication, and swallowing. It also leads to dramatic changes in other daily activities such as swallowing, olfaction, cough, sneezing, etc., Certain activities like swimming become impossible, while others such as bathing under a shower, generating positive pressure to lift heavy objects become extremely difficult. The questionnaire therefore included questions related to nasal airway and breathing, laryngeal functions, and lastly questions related to adaptation following TL. The questionnaire has not been validated. We intend to validate the questionnaire in our next study with larger sample size.
The first five questions were related to nasal airway and nasal breathing. The next four questions were related to false perceptions of intact laryngeal functions. The last two questions dealt with post-laryngectomy adaptation and hence for these two questions – a negative reply was considered to be suggestive of presence of a phantom larynx phenomenon.
RESULTS
At the conclusion of the survey, we divided 66 patients into two subgroups, depending on whether they were assessed within or after 6 months after the surgery. Duration of 6 months was chosen because phantom phenomena are generally known to persist for about 6 months and slowly tend to decline. Overall, 22 patients were assessed within 6 months following surgery, whereas 44 patients were assessed 6 months after the surgery. Table 1 shows numbers and percentage of patients in early post-operative period ( < 6 months) group responding as “yes” to each of the questions. Table 2 shows numbers and percentage of patients in early post-operative period ( < 6 months) group responding as “yes” to each of the questions. Tables Tables33 and and44 shows numbers and percentages of the groups and their comparison trends as well as “P” value calculated using statistical analysis.
Tables33 and and44 shows numbers and percentages of the groups and their comparison trends as well as “P” value calculated using statistical analysis.Table 2
Patients assessed within 6 months following surgery and responding as “yes” for each question
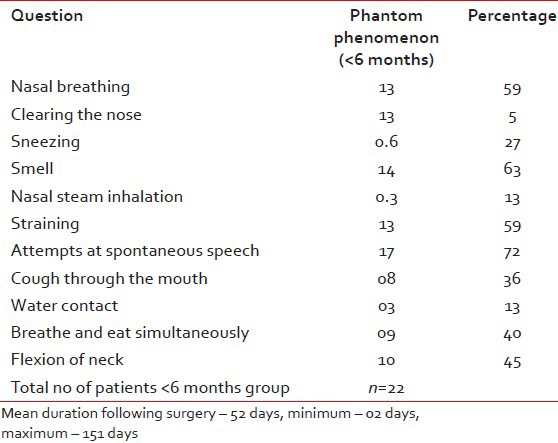
Table 3
Patients assessed at least 6 months following surgery and responding as “yes” to all questions
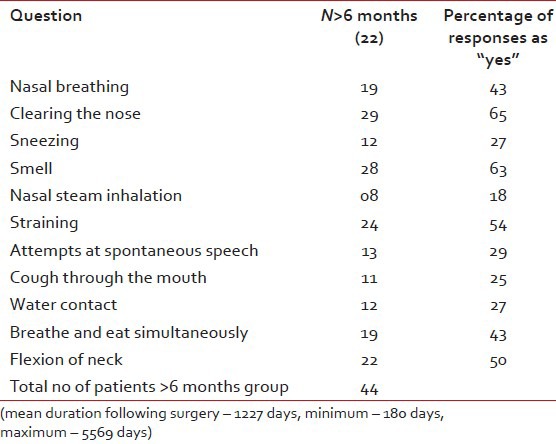
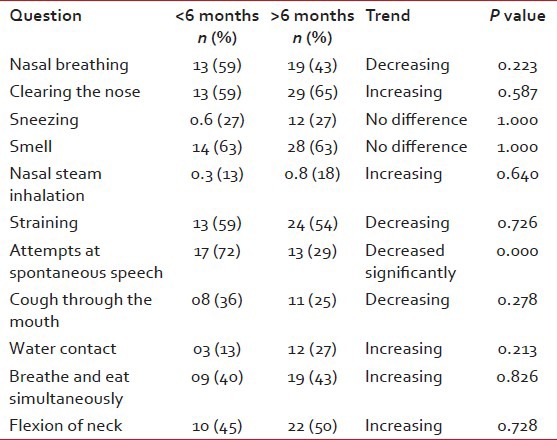
Table 4
Comparison of phantom phenomena among the two groups of post-laryngectomy patients and their trends (increasing or decreasing)
Statistical analysis
Statistical analysis was done using predictive analytics software (PASW), Version 18.
Normality of the data was assessed using Kolmogorov–Smirnov test. “Chi square” was used as the test of significance to compare the two groups.
All patients showed evidence of a phantom larynx phenomenon. In majority of these patients, it persisted even after 6 months following surgery. There was no significant difference in the two groups (less than or more than 6 months) except for one question pertaining to attempts at speech without occlusion of stoma (77% vs. 29%, P value 0.000). False perception of nasal breathing (59% and 43%) and olfactory sensation (63% in both groups) were the most common phantom larynx phenomenon across the two groups. Phantom phenomena of attempts at sneezing through the nose (27.27% in both groups) and nasal steam inhalation (13.63% and 18.18%) were comparatively less in both groups.
DISCUSSION
Surgical treatment of advanced laryngeal and hypopharyngeal cancers often requires a TL, resulting in a permanent tracheostomy and potential difficulties with a patient's speech, communication, and swallowing. “Phantom limb” phenomenon is well known following amputation of a limb or other part of the body. Phantom sensations of other internal organs (bladder, rectum, stomach, and genitalia) have also been reported in literature. The interruption of afferent input to the brain from internal organs leads to the experience of phantom sensations. Data from neurosurgical studies of electrical stimulation of the awake human brain and from functional neuroimaging data strongly suggest the presence of a specific “larynx and phonation” area in human motor cortex. There is also evidence to show that cutaneous stimulation of face and neck leads to phantom larynx sensation suggestive of “cortical reorganization” following TL. We conducted a clinical survey of patients using a specifically structured “Phantom Larynx Questionnaire” to detect the presence of phantom larynx phenomenon.
All patients showed evidence of a phantom larynx phenomenon in our study. In majority of these patients, it persisted even after 6 months following surgery.
Phantom phenomena related to nasal airway were more predominant as compared to other phenomena. Only false perception of nasal breathing showed a decreasing trend, whereas attempts to clear the nose using forceful expiration had actually increased, behavior of sneezing through nose and pseudo or false olfactory sensation remained static and the attempts for nasal steam inhalation had actually increased when compared to the long-term follow-up group.
False perception of intact laryngeal functions such as straining to attempt valsalva maneuver, attempts at spontaneous speech without occluding the stoma (none of our patients have used hand-free devices) were found to be less in the long-term follow-up group. The difference for phantom phenomena of attempts at speech without occlusion of stoma was statistically significant between the two groups (P–0.000). Speech being a highly repetitive function, patients possibly get habituated faster for this function. As for the function of airway protection while bathing, there was a slight increasing trend in the long-term follow-up group.
The last two questions were related to post-laryngectomy adaptation of the patient and understanding of anatomical and physiological changes following the procedure. The first one was related to understanding by the patient that the airway and food passages are now separate and hence breathing and eating could be performed simultaneously. The second such phenomenon was related to neck posture. Majority of laryngectomees have partial stomal occlusion on neck flexion with difficulty to breathe. Most patients develop a habit of avoiding neck flexion in all activities including sleep. Development of such a habit was considered to be good adaptation, whereas persistent events of neck flexion with experiences of choking sensation intermittently were presumed as presence of a phantom larynx perception. There was an decreasing trend for both perceptions indicating that patients perhaps develop a better understanding of the anatomical and physiological changes following TL over a period of time.
There has been no definite description of phantom larynx phenomenon in literature. There is already developing knowledge on phantom larynx phenomenon from recent studies based on neuroimaging data and cutaneous sensations.[2,5] Considering the descriptions of phantom phenomenon for other internal organs and results of our study, we believe that phantom larynx phenomenon exists. It is present not only in the immediate post-operative period but also persist in many patients even after 6 months following the surgery. Phantom limb phenomenon is known to cause anxiety among patients. Similarly, phantom larynx phenomenon may cause difficulty in rehabilitation of post-laryngectomy patients. Delayed or difficult rehabilitation to various daily functions affected may cause anxiety and depression among these patients. There is enough literature to suggest that TL surgery is associated with anxiety and depression and thereby poor quality-of-life among survivors. Whether and how much of it is caused by such a phantom phenomenon is not known. It will be interesting to study the relation of phantom phenomenon and its association with rehabilitation of such patients as well as degree of anxiety and depression in patients showing marked phantom phenomena. Lack of patient education could be a major contributing factor apart from the “cortical representation” of larynx. Thorough counseling regarding the normal anatomy and physiology of larynx as well as changes taking place after the surgery is necessary. Patients must be educated about changes in simple functions, viz – breathing, olfaction, cough, sneezing, speech, etc. We believe that education and rehabilitation with regards to such a phenomenon are therefore needed in all patients.
The aim of treatment policy is not just to treat cancer but also simultaneously achieve the best functional results and avoid serious complications. We plan to prospectively study the “phantom larynx” phenomenon and adaptation to it post-operatively. We also want to validate the questionnaire used in this study by performing a prospective study.
CONCLUSION
Phantom larynx phenomenon exists. It occurs not only in early post-operative period but also in long-term follow-up period after laryngectomy. It may cause anxiety and poor rehabilitation among patients. Lack of patient education could be a major contributing factor apart from the cortical representation of larynx. Further prospective studies regarding such a phenomenon are needed. Patient education regarding such a phenomenon may help decrease anxiety and depression following the surgery and improve the quality-of-life of laryngectomees.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.


 PDF
PDF  Views
Views  Share
Share

