Comparative study of effectiveness of Pap smear versus visual inspection with acetic acid and visual inspection with Lugol's iodine for mass screening of premalignant and malignant lesion of cervix
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2012; 33(03): 161-165
DOI: DOI: 10.4103/0971-5851.103143
Abstract
Background and Objective: Cancer of the cervix is a leading cause of morbidity and mortality among women worldwide. Therefore, to curb the disease, there is a need to develop a screening test that has good sensitivity and specificity. The present study is aimed to compare the effectiveness of the Pap smear, visual inspection with acetic acid (VIA) and visual inspection with Lugol′s iodine (VILI) for mass screening of premalignant and malignant lesions of the cervix; to evaluate the usefulness of VIA and VILI as an adjunct to improve sensitivity of cervical cytology; and to evaluate the role of VILI as a parallel screening method with VIA to enhance its test performance. Design and Setting: This was a prospective, analytical study in which 210 patients of the reproductive age group attending the gynecology OPD were enrolled. Patients and Methods: Patients were first subjected to Pap smear followed by VIA, VILI, colposcopy and biopsy for confirmation of lesion, if needed. Data was obtained and statistically analyzed. Results: Of the 210 patients, 34 (16.27%) had positive Pap test, 29 (13.87%) had positive VIA and 24 (11.43%) had positive VILI and 31 (14.75%) showed features of cervical intraepithelial neoplasia (CIN) on colposcopy. Of the total of 48 patients in whom either of the screening tests was positive and had undergone cervical biopsy, one had CIN-3, three had CIN-2, 12 had CIN-1, three had carcinoma in situ CIS and 29 reported normal. In our study, 40 patients were picked up as positive by combination of these tests, of which 19 (47.50%) had CIN on biopsy. Conclusion: Our study showed that VIA and VILI had sensitivity comparable to Pap smear and can thus be a suitable potential alternative/adjunctive screening test not only in a resource-poor setting but in well-equipped centers also. And, use of a combination of tests (Pap+VIA+VILI) had 100% sensitivity but at cost of low specificity and more false-positive results.
Keywords
Cervical cancer - Pap smear - visual inspection with acetic acid - visual inspection with Lugol′s iodinePublication History
Article published online:
02 August 2021
© 2012. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Background and Objective:
Cancer of the cervix is a leading cause of morbidity and mortality among women worldwide. Therefore, to curb the disease, there is a need to develop a screening test that has good sensitivity and specificity. The present study is aimed to compare the effectiveness of the Pap smear, visual inspection with acetic acid (VIA) and visual inspection with Lugol's iodine (VILI) for mass screening of premalignant and malignant lesions of the cervix; to evaluate the usefulness of VIA and VILI as an adjunct to improve sensitivity of cervical cytology; and to evaluate the role of VILI as a parallel screening method with VIA to enhance its test performance.
Design and Setting:
This was a prospective, analytical study in which 210 patients of the reproductive age group attending the gynecology OPD were enrolled.
Patients and Methods:
Patients were first subjected to Pap smear followed by VIA, VILI, colposcopy and biopsy for confirmation of lesion, if needed. Data was obtained and statistically analyzed.
Results:
Of the 210 patients, 34 (16.27%) had positive Pap test, 29 (13.87%) had positive VIA and 24 (11.43%) had positive VILI and 31 (14.75%) showed features of cervical intraepithelial neoplasia (CIN) on colposcopy. Of the total of 48 patients in whom either of the screening tests was positive and had undergone cervical biopsy, one had CIN-3, three had CIN-2, 12 had CIN-1, three had carcinoma in situ CIS and 29 reported normal. In our study, 40 patients were picked up as positive by combination of these tests, of which 19 (47.50%) had CIN on biopsy.
Conclusion:
Our study showed that VIA and VILI had sensitivity comparable to Pap smear and can thus be a suitable potential alternative/adjunctive screening test not only in a resource-poor setting but in well-equipped centers also. And, use of a combination of tests (Pap+VIA+VILI) had 100% sensitivity but at cost of low specificity and more false-positive results.
INTRODUCTION
According to the World Health Organization, cervical cancer is the second most common type of cancer among females, and was responsible for over 250,000 deaths in 2005. Approximately 80% of these deaths occurred in developing countries. Without urgent intervention, deaths due to cervical cancer are projected to rise by almost 25% over the next 10 years.
Cancer cervix has been considered preventable because it has a long preinvasive state and availability of screening programs and treatment of preinvasive lesions is effective. It has been well established that well-organized screening by cytology has substantially reduced the incidence of morbidity and mortality from cervical cancer in developed countries.[1–3]
Many developing countries do not have ample resources to implement cytology-based prevention programs, which necessitates well-organized laboratories to collects material and specialized personnel apt to render a diagnosis.[4]
Newer approaches such as automated Pap, liquid-based Pap and HPV DNA testing using hybrid capture II (HC II) are time consuming, expensive and not widely available. Prompted by the need for optimal strategies for cervical cancer screening in low-resource settings, the role of visual inspection with acetic acid (VIA) and visual inspection with Lugol's iodine (VILI) has been widely studied in several recent studies, which suggest that VIA and VILI closely match the Pap smear in its performance in detecting cervical cancer precursor.[5] The present study is an endeavor to perform a comparative study of performance of VIA and VILI used as a stand-alone test and combined with Pap smear for mass screening of premalignant and malignant lesions of the cervix.
PATIENTS AND METHODS
The present study was carried out in the Department of Obstetrics and Gynaecology at the Northern Railway Central Hospital, Delhi, for a period of 1 year ( June 2007 to May 2008). A total of 210 patients attending the gynecology OPD were enrolled in the study. Patients to be screened were explained the procedure to be performed, written informed consent was taken and the relevant obstetrical and gynecological history was also taken, with the patient being reassured that the procedure was painless. Firstly, a Pap smear was taken with Ayre's spatula and cytobrush and was evaluated by the Bethesda system. Following the Pap smear, VIA was performed with 3% acetic acid followed by Lugol's iodine test (VILI). Results of VIA and VILI were recorded after waiting for 1 minute as negative, single-positive and double-positive. All the tests were performed by trained residents and faculty who did not know the aims and objective of the study, and was also done separately by different residents/faculty.
All the patients in the study were subjected to colposcopy. The cervix was inspected with the naked eye than with a colposcope. After taking the Pap smear, the cervix was washed with normal saline and visualized, followed by application of 3% acetic acid and visualization by colposcope followed by application of Lugol's iodine and colposcopy. Grading of lesion was done according to the Reid's colposcopic index. Biopsy was done for confirmation of lesion if either of the three screening tests or colposcopy had a positive finding or if the Pap smear reported ASCUS, for confirmation of lesion. Collected data was statistically analyzed to determine specificity and sensitivity, PPV, NPV of Pap smear, VIA, VILI alone and Pap+VIA+VILI and VIA+VILI. The patients who reported normal on all screening tests and colposcopy were called for annual follow-up. Patients who were positive at either of the screening tests or colposcopy underwent biopsy and were treated according to the grade of the lesion (6-monthly follow-up and repeat Pap, loop electrode excision procedure (LEEP), hysterectomy, Wertheime's hysterectomy). Approval from ethical committee of our institute was taken before commencing the study.
RESULTS
Table 1 shows that out of 210 patients enrolled in the study, 34 patients (16.27%) had a positive Pap smear, 23 patients (11.00%) had inflammatory smears and 152 had normal smear. VIA was positive in 29 patients (13.81%) while the remaining 181 patients (86.19%) had normal VIA. VILI was positive in 24 patients (11.43%) and the remaining 186 patients (88.57%) had normal VILI. Of the 210 patients, 31 patients (14.75%) showed features of CIN on colposcopy; the remaining were normal.
Table 1
Result of Pap smear, VIA, VILI and colposcopy examination among the study group
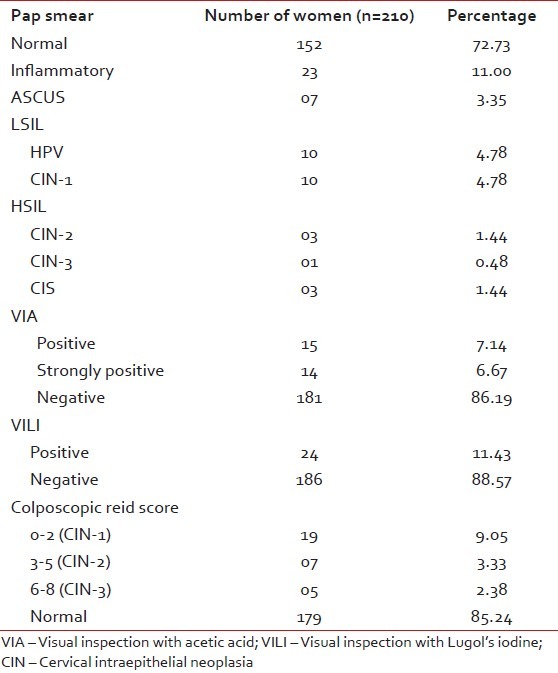
Table 2 shows that of a total of 210 Pap smears performed, 27 were reported positive excluding ASCUS. Of these 27 positive cases, 16 (i.e., 59.26%) had CIN on histopathological examination and three (14.29%) patients who reported negative on Pap smear (but positive on other screening tests) had positive histopathological examination. Of the 29 VIA-positive cases, 16 (i.e., 55.17%) had CIN on histopathological examination and three (15.79%) patients who had negative VIA (but positive on other screening tests) were reported to have positive histopathological examination. Of the 24 VILI-positive cases, 17 (i.e., 70.83%) had CIN on histopathological examination and two cases (10.53%) that were missed on VILI (but positive on other screening tests) had positive histopathological examination.
Table 2
Correlation of Pap smear, VIA and VILI with histopathological examination
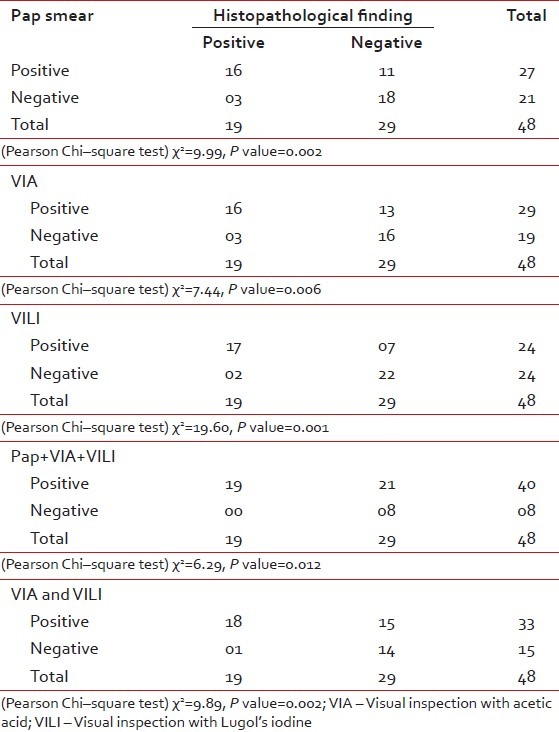
Of the total 210 patients in whom all three screening tests (Pap+VIA+VILI) were performed, 40 patients were picked up as positive by a combination of these tests; of these 40 positive cases, 19 (i.e., 47.50%) had CIN on histopathological examination and no cases were missed by using a combination of these tests. This thus proved the adjunctive role of VIA and VILI to Pap smear in picking up premalignant and malignant lesions of the cervix, increasing the sensitivity of combination tests to 100% but at the cost of decreasing the specificity to 27.60%. Of the total of 210 patients in whom VIA+VILI was performed, 33 (68.75%) had positive results. Of these 33 cases, 18 (i.e., 54.55%) had CIN on histopathological examination, one case (5.26%) was missed on a combination of tests (VIA+VILI), which was picked up to be positive on histopathological examination. This thus proved the role of VILI as a parallel screening test to VIA.
The sensitivity, specificity, NPV and PPV of different screening tests or their combinations are shown in Table 3. Sensitivity of Pap smear=84.20% (CI 59.50–95.80), specificity of Pap smear=62.10% (CI 42.40–78.70), PPV of Pap smear=59.30% (CI 39.00–77.00), NPV of Pap smear=85.70% (CI 62.60–96.20), % of false positive=37.93% and % of false-negative=15.79%.
Table 3
Tests characteristic of screening tests in detecting CIN or worse lesion
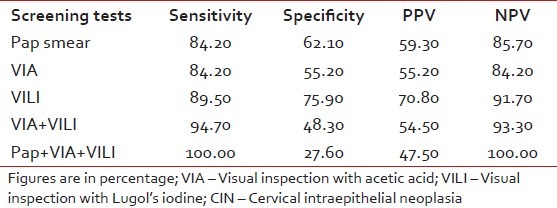
Sensitivity of VIA=84.20% (CI 59.50–95.80),pspecificity of VIA=55.20% (CI 36.00–73.00), PPV of VIA=55.20% (CI 36.00–73.00), NPV of VIA=84.20% (CI 59.50–95.80), % of false-positive=44.83% and % of false-negative =15.79%.
Sensitivity of VILI=89.50% (CI 65.50–98.20), specificity of VILI=75.90% (CI 56.10–89.00), PPV of VILI=70.80% (CI 48.80–86.60), NPV of VILI=91.70% (CI 71.50–98.50), % of false-positive=24.14% and % of false negative=10.55%.
Sensitivity of combination tests=100.00% (CI 79.10–100.00), specificity of combination tests=27.60% (CI 13.40–47.50), PPV of combination tests=47.50% (CI 31.80–63.70), NPV of combination tests=100.00% (CI 59.80–100.00), % of false positive=72.41% and % of false negative=00%.
Sensitivity of combination tests (VIA+VILI)=94.70% (CI 71.90–99.70), specificity of combination tests (VIA +VILI)=48.30% (CI 29.90–67.10), PPV of combination tests (VIA+VILI)=54.50% (CI 36.60–71.50), NPV of combination tests (VIA+VILI)=93.30% (CI 66.60–99.70), % of false positive=78.95% and % of false-negative=5.26%.
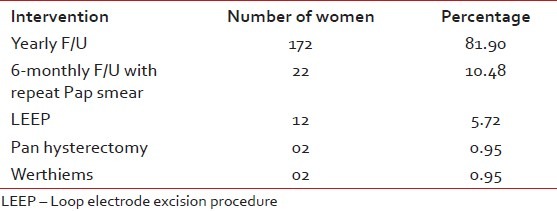
Table 4 shows that of the 210 women screened, 172 were called for annual follow-up and 22 patients who reported ASCUS on Pap smear and CIN-1 on colposcopy and histopathological examination and who were complaint were called after 6 months for follow-up and repeat Pap smear. Twelve patients who reported CIN-1 (who were not complaint and had associated risk factors) and CIN-2 underwent LEEP. Two patients who had CIN-3 and CIS (with superficially invasive cancer with negative margins) underwent Pan hysterectomy. Two patients with CIS had Werthiems hysterectomy performed.
Table 4
Intervention done in patients enrolled in the study on the basis of screening test results and positive histopathlogical findings
DISCUSSION
In a metaanyalsis done by Fahey et al. in 1995[6] involving 62 studies conducted between 1984 and 1992, the mean sensitivity and specificity of cytology was 58% (range 11–99%) and 68% (range 14–97%), respectively. In another recent metaanalysis by Nanda et al. in 2000,[7] the sensitivity of cytology to the detection of CIN 2 or worse lesions ranged from 18% to 98% and the specificity ranged from 17% to 99%. In the IARC multicenter study done in India and Africa by Sankaranarayanan et al. in 2004,[8] which included 11 cross-sectional studies, the sensitivity of VIA ranged from 56.10% to 93.90% and the specificity ranged between 74.20% and 93.80%.
Considering the various studies, our results of Pap smear as a screening test are comparable. In the present study, the sensitivity of Pap smear was 84.20% and the specificity was 62.10%.
In the present study, the sensitivity of VIA was 84.20%, which was similar to that of Pap smear, but had a lesser specificity than the Pap smear (Pap 62.00% vs. VIA 55.20%).
The reason behind the high sensitivity and/or low specificity of VIA in our study could be due to:
- Presence of infection and inflammation that take up acetowhite stain
- Some faint acetowhite areas might have been interpreted as being positive
- Scoring those areas with distinct acetowhite uptake on cervix as positive.
Because of the high number of false-positive cases and low specificity of VIA, the usefulness of this procedure is limited. But, due to the high sensitivity of VIA, it is still used as primary screening in some developing countries for early detection of cervical carcinoma.
In the present study, the results are in comparison with that of the above-mentioned studies, suggesting that VIA may find a place as an alternative low-resource technology and low-cost method of screening and case finding.
In the IARC multicenter study done in India and Africa by Sankaranarayanan et al. in 2004,[8] which included 11 cross-sectional studies, the sensitivity of VILI ranges from 76.00% to 97.00% and the specificity between 73.00% and 91.30%.
In the present study, of the 210 patients, VILI was positive in 24 (i.e., 11.43%) patients. (Sensitivity 89.5% and specificity 75.90%). In our study, the reason for high sensitivity and low percentage of FP results of VILI as compared with that of VIA (VILI vs VIA 89.50% vs 84.2%) are because Lugol's iodine produces characteristic nonuptake yellow areas in suspected cases that are easy to interpret, and observation was based on the well-defined criteria to identify between iodine uptake and nonuptake, mahagony brown area versus yellow areas. An atlas also has been referred from time to time for characteristic identification of lesions in case of doubt.
In the present study, the combined sensitivity of VIA and VILI performed together was 94.70%, which was significantly greater than the sensitivity of individual procedures, thus showing that VILI can be used as a parallel screening test to VIA to enhance its test performance. The Sankarnarayan et al. 2004[8] study showed a similar result and recommended the use of both VIA and VILI in parallel to increase test sensitivity.
In our study, we tried to find out whether the combination of tests (i.e., Pap smear, VIA and VILI) improves the sensitivity of the screening tests. Our results showed that when all three (Pap smear+VIA+VILI) are used in combination, the sensitivity is 100%, but this happens at the cost of increasing the percentage of false-positive and decreasing the specificity. Also, our study showed that when VILI is used in combination with VIA, the sensitivity has improved to 94.70% from around 84.20%.
Our results are consistent with that of the Panten et al. 1995[9] study at the University of Jimbanbe/JHPIEGO cervical cancer project 1999,[10] Denny et al. 2000[11] and Shankaranarayan et al. 2003[12] studies, which showed that combining VIA and VILI with Pap smear markedly improved their performance as screening tests at the cost of large number of women being referred for further treatment in view of false-positive results and decreased specificity of the test.
An attempt has been made in present study to increase awareness of women about cervical cancer and preventive health-seeking behavior, screen all women of the reproductive age group at least once a year and motivate them for annual screening until three negative Pap smears, to provide a screening test with high sensitivity as women have less frequent opportunities for repeated screening and treating women with high-grade dysplasia and cancer.
Women continue to ignore symptoms of irregular bleeding, postmenopausal bleeding and postcoital bleeding. Therefore, in our study, we aimed at educating women about these signs and symptoms and to seek immediate medical care.
Thus, an attempt has been made to target the disease before its onset at the level of primary prevention by providing education and counseling and secondary prevention by effective screening and treatment.
CONCLUSION
Cervical cancer is “preventable but not prevented” remains the reality today, because no perfect screening tests are available that have 100% sensitivity and good specificity. Therefore, in the present study, an attempt has been made to analyze Pap smear, VIA and VILI as standalone tests and when used in combination.
We found that the combination tests had 100% sensitivity but at the cost of low specificity and more false-positive results. Our study showed that VIA and VILI had sensitivity comparable to Pap smear and can therefore be a suitable potential alternative/adjunctive screening test not only in resource-poor settings but also in well-equipped centers. But, these drawbacks are low cost to pay for preventing and diagnosing disease at an early stage for effective control.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared


 PDF
PDF  Views
Views  Share
Share

