Critical clinical appraisal of the role of computed tomography-guided minimally invasive aspiration cytology in evaluation of retroperitoneal masses
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2014; 35(01): 60-65
DOI: DOI: 10.4103/0971-5851.133723
Abstract
Context: Fine-needle aspiration (FNA) is increasing in popularity as a means of diagnosing mass lesions in retroperitoneal area. With use of radiologic guidance for needle placement, this technique is an effective way to obtain diagnostic material. Aims: The aims of the study were (1) to establish the validity and reliability of fine needle aspiration cytology in preoperative diagnosis of retroperitoneal tumor, and (2) to compare the significance of cytological diagnosis with histopathological report. Settings and Design: A prospective, cross-sectional hospital-based study. Materials and Methods: A prospective, cross-sectional study was designed on 45 cases of clinically and radiologically diagnosed retroperitoneal tumor in a tertiary care hospital. Computerized tomography (CT)-guided percutaneous FNA was performed and cytology smears were stained with May-Grünwald-Giemsa stain and conventional Papanicolaou (Pap) stain. Smears were broadly categorized into unsatisfactory, benign, suspicious of malignancy and malignant lesion. The cytological diagnosis was compared with subsequent histopathology report. Statistical Analysis: Positive and negative predictive values, diagnostic accuracy, chi-square test and others. Results: The total number of cases studied was 45, which include both epithelial tumors and mesenchymal tumors. Age group varied from 15 to 70 years. The overall sensitivity in our study to diagnose benign and malignant tumors by FNA cytology is 86% and the specificity is 96% with positive and negative predictive value of 86% and 96%, respectively. Diagnostic accuracy was 93.55% with high statistical significance (P < 0 class="b" xss=removed>Conclusions: FNA cytology is a simple, fast, reliable and less expensive method for diagnosis of various retroperitoneal neoplasms.
Keywords
Computed tomography - fine needle aspiration cytology - histopathology - May-Grόnwald-Giemsa stain - retroperitoneal massPublication History
Article published online:
19 July 2021
© 2014. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Context:
Fine-needle aspiration (FNA) is increasing in popularity as a means of diagnosing mass lesions in retroperitoneal area. With use of radiologic guidance for needle placement, this technique is an effective way to obtain diagnostic material.
Aims:
The aims of the study were (1) to establish the validity and reliability of fine needle aspiration cytology in preoperative diagnosis of retroperitoneal tumor, and (2) to compare the significance of cytological diagnosis with histopathological report.
Settings and Design:
A prospective, cross-sectional hospital-based study.
Materials and Methods:
A prospective, cross-sectional study was designed on 45 cases of clinically and radiologically diagnosed retroperitoneal tumor in a tertiary care hospital. Computerized tomography (CT)-guided percutaneous FNA was performed and cytology smears were stained with May-Grünwald-Giemsa stain and conventional Papanicolaou (Pap) stain. Smears were broadly categorized into unsatisfactory, benign, suspicious of malignancy and malignant lesion. The cytological diagnosis was compared with subsequent histopathology report.
Statistical Analysis:
Positive and negative predictive values, diagnostic accuracy, chi-square test and others.
Results:
The total number of cases studied was 45, which include both epithelial tumors and mesenchymal tumors. Age group varied from 15 to 70 years. The overall sensitivity in our study to diagnose benign and malignant tumors by FNA cytology is 86% and the specificity is 96% with positive and negative predictive value of 86% and 96%, respectively. Diagnostic accuracy was 93.55% with high statistical significance (P < 0>
Conclusions:
FNA cytology is a simple, fast, reliable and less expensive method for diagnosis of various retroperitoneal neoplasms.
INTRODUCTION
The retroperitoneal space is a part of the posterior abdomen and is demarcated anteriorly by the posterior parietal peritoneum and posteriorly by paravertebral skeletal muscles and fasciae. It is the site of diverse group of pathological processes arising from either retroperitoneal organs or from lymphoid and connective tissues.
Rapid preoperative diagnosis is important for surgeons to avoid operative intervention in certain benign conditions and for early institution of chemotherapy in malignant tumors. Fine-needle aspiration cytology (FNAC) is a cost-effective method, which provides rapid preoperative diagnosis with high accuracy. It helps to differentiate benign from malignant lesions and also primary malignancy from metastatic. Regarding diagnostic accuracy, FNAC is concordance with open biopsy in both non-neoplastic and neoplastic lesions.[1] Most of the retroperitoneal masses are non — palpable and even if they are palpable, correct and accurate assessment of size, shape and the extent of the lesion is difficult. Therefore, various imaging modalities like computed tomography (CT) and ultrasonography (USG) are used as a guide for fine-needle aspiration (FNA). Dissociated viable cells obtained by FNA can be used for ancillary techniques.[2]
The procedure's low complication rate is an additional advantage which allows FNAC to be performed as an out-patient procedure. It is also a suitable procedure when patients are debilitated or have multiple lesions.
MATERIALS AND METHODS
This prospective, single-centered study was conducted on 45 patients in the Department of Pathology in a tertiary care hospital in collaboration with Department of Radiology from June 2011 to May 2013. Inclusion criteria were
- Patients presented with clinically symptomatic retroperitoneal mass,
- Incidentally diagnosed retroperitoneal mass on imaging,
- Patients who gave consent and fully co-operative during the study process.
Patients having bleeding disorders were excluded from the study.
After taking valid consent from the patient, a detailed history was taken and clinical examination was done. The approach used for intervention varied according to the size and location of the lesion. Anterior, lateral and posterior approaches were selected and patients were positioned accordingly. An 88-mm long, 22-23 G lumber puncture needle was used along with 10 cc disposable syringe for aspiration of representative samples. With the help of Siemens CT Emotion Series scanner, scan was done in axial plane by taking 10 mm thin contiguous parallel slices. CT image helps in localizing the dermal entry point which was marked by the needle used for local anesthesia. 1% lidocaine was used for local anesthesia. CT-guided aspiration was done from the solid area and from the margin of the tumor (avoiding any area of necrosis). Grease-free plain glass slides were used for smear preparation. Two slides were air dried and stained with May-Grunewald-Giemsa (M™.G) stain. Two slides were fixed in 95% ethyl alcohol and stained with Papanicolaou stain. We assessed the adequacy and quantity of cells in each stained smear. Inadequate smear was characterized by paucicellularity and poorly preserved cellular morphology. If those patients with inadequate smears remained asymptomatic without any complication, a repeat aspiration was performed.
Stained smears were examined depending on the following cytological parameters — background, arrangement, cytological pattern, cellular subtype, nuclei and chromatin pattern. Smears were broadly categorized into unsatisfactory, benign, suspicious of malignancy and malignant lesion. Histopathological reports either from surgical specimen or from tru-cut biopsy were available in 31 cases. Considering histopathology as gold standard, sensitivity and specificity of FNAC were obtained.
RESULTS
Forty-five cases of retroperitoneal masses were included aged between 15 and 70 years. Twenty-two patients (49%) were males and 23 were (51%) females.
Out of 45 cases, 28 cases (62.2%) were malignant, 13 cases (28.9%) were benign and 1 case (2.2%) was of suspicious lesions. There were about 6.7% unsatisfactory smears [Table 1]. According to radiological and cytological findings, malignant and benign cases were classified into six categories: renal lesions, adrenal lesions, germ cell tumors, lymphoid lesions, soft tissue mass and miscellaneous [Tables [Tables22 and and33].
Table 1
Distribution of all cases according to cytological diagnostic category
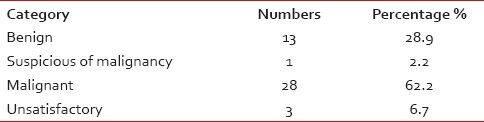
|
Table 2
Distribution of benign retroperitoneal lesions
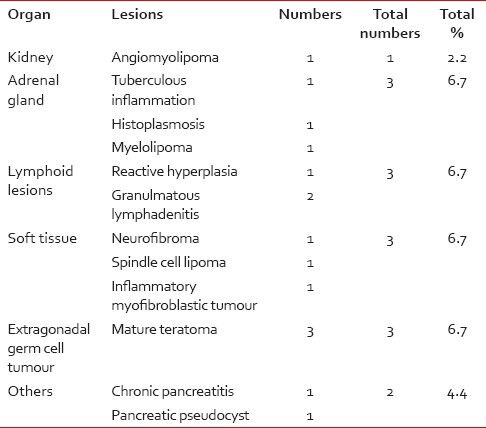
|
Table 3
Distribution of malignant retroperitoneal lesions
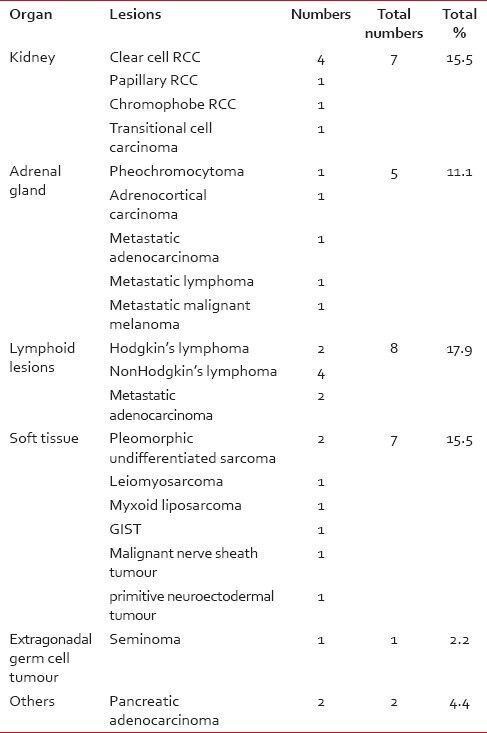
|
Lymphoid lesions
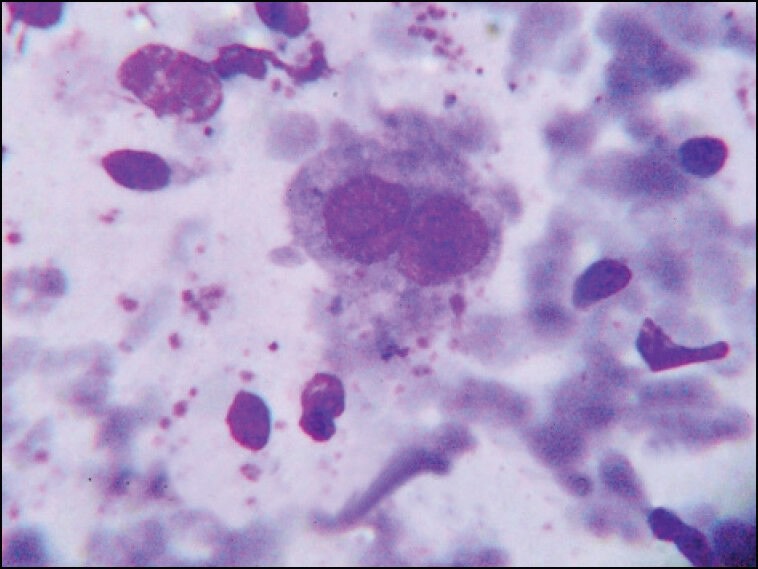
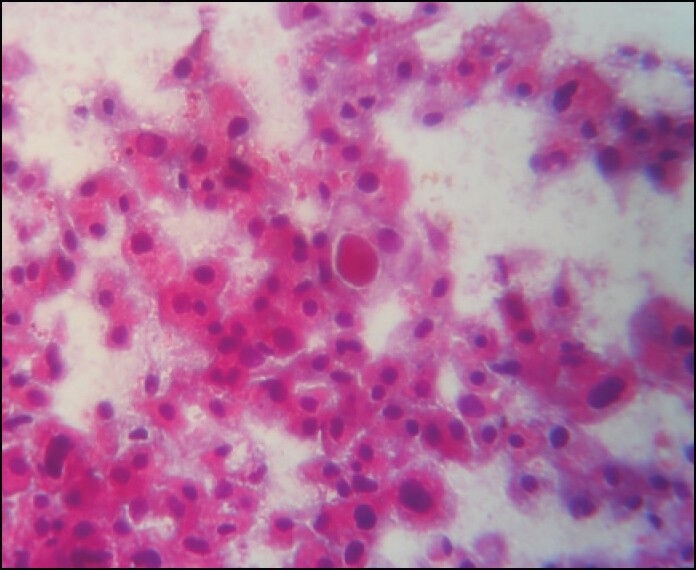
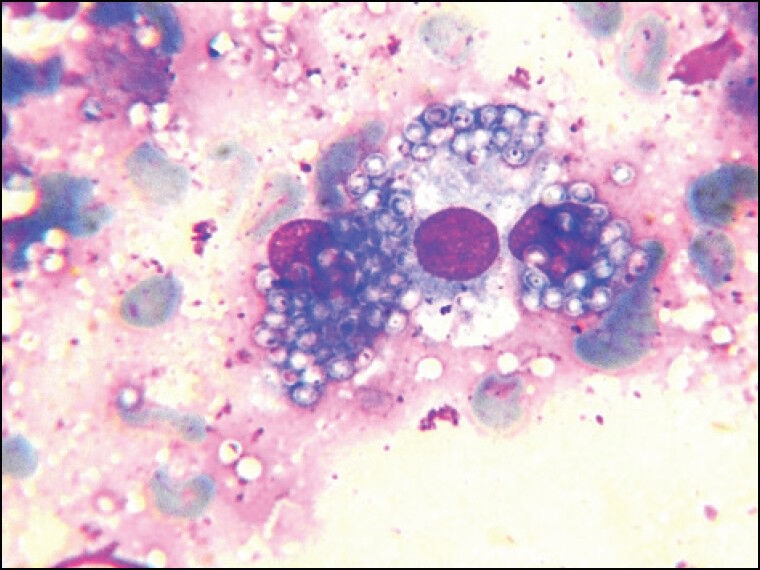
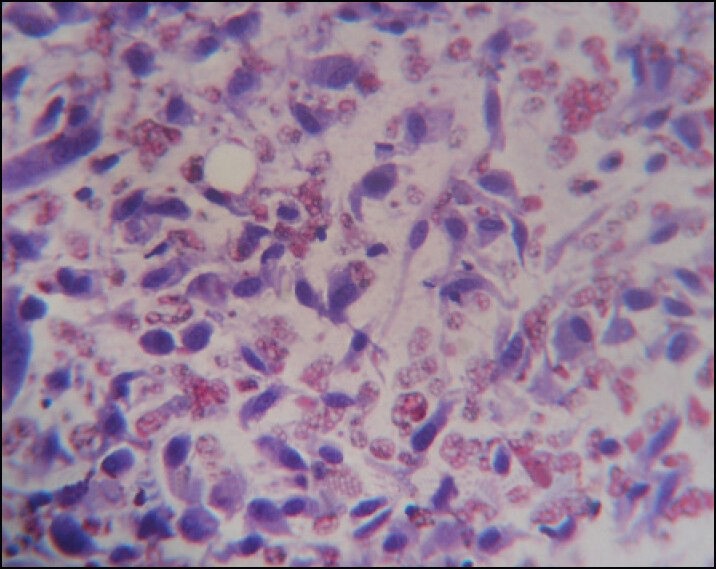
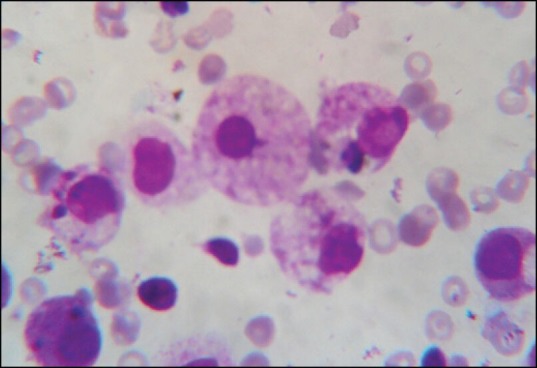
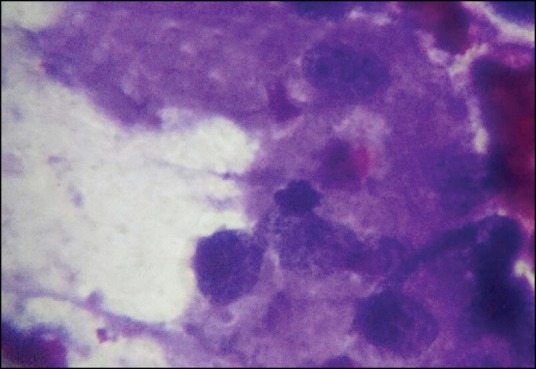
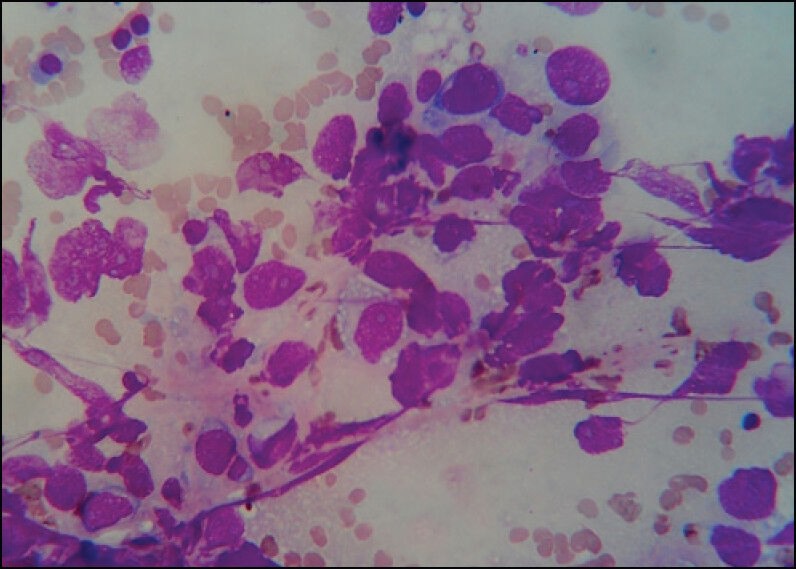
Lymphoid lesions comprised of major number of cases (24.6%). One case was diagnosed as reactive hyperplasia of lymph node. The smear showed a mixed population composed of small and large lymphocytes with cleaved nuclei and tingible body macrophages. Two cases were reported as granulomatous lymphadenitis showing epithelioid histiocytes and Langhan's type of giant cells against a background of extensive necrosis [Figure 1]. Diagnosis of tuberculous lymphadenitis was confirmed in both cases after identification of acid fast bacilli. Four cases were diagnosed as non-Hodgkin lymphoma. Aspirates from all four cases revealed similar cytological features, consisting of monomorphous population of medium-sized lymphoid cells having irregular nuclear profiles and fine nuclear chromatin with abundant lymphoglandular bodies in the background. Two cases of Hodgkin lymphoma showed classic Reed-Sternberg (R-S) cells in a background of eosinophils, lymphocytes and histiocytes [Figure 2]. Mononuclear R-S cells (Hodgkin cells) were also found. Two cases of metastatic lesions were diagnosed.
| Figure 1:Cytology of granuloma ×400
| Figure 2:Cytology of Hodgkins disease ×1000
Soft tissue
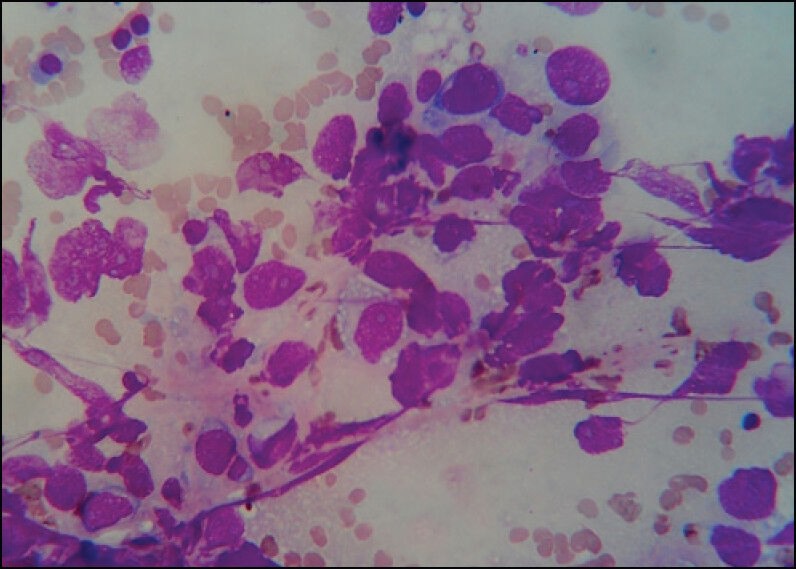
Depending on different cytomorphological appearances, two cases (4.4%) represented pleomorphic type, one case (2.2%) was of round cell tumors, five cases (11.1%) were of spindle cell tumors and the remaining one case was of myxoid category [Figure 3]. All categories except spindle cell tumors were histologically diagnosed as sarcomas. Three cases (6.7%) of spindle cell subtype were malignant [Figure 4]. Aspirate from one case of histologically diagnosed leiomyosarcoma showed only necrotic materials and considered as unsatisfactory smear. One case of inflammatory myofibroblastic tumor was wrongly diagnosed as spindle cell sarcoma.
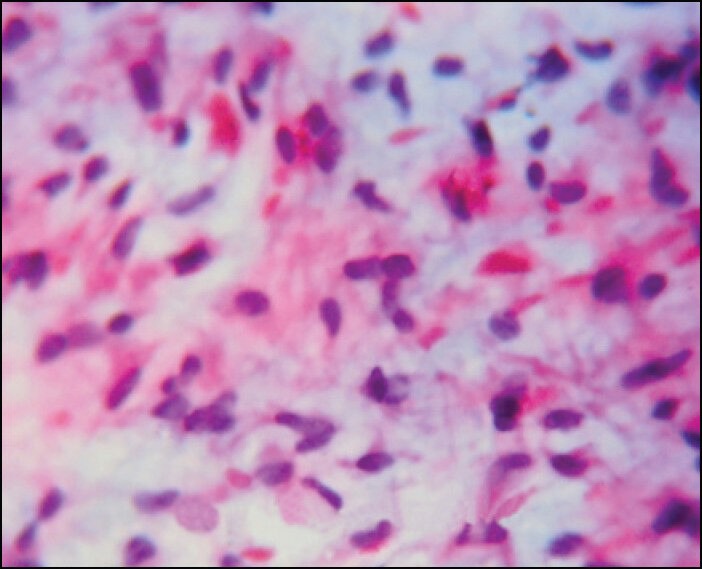
| Figure 3:Cytology of myxoid tumor ×400
| Figure 4:Cytology of malignant spindle cell tumor ×400
Renal lesions
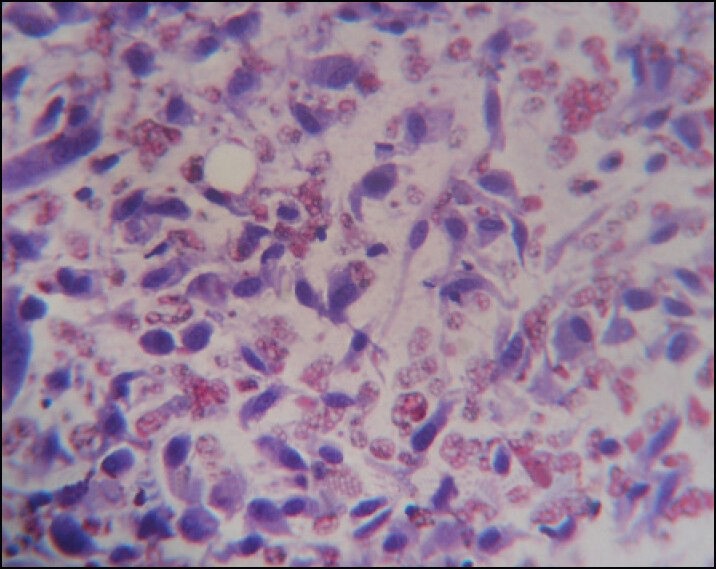
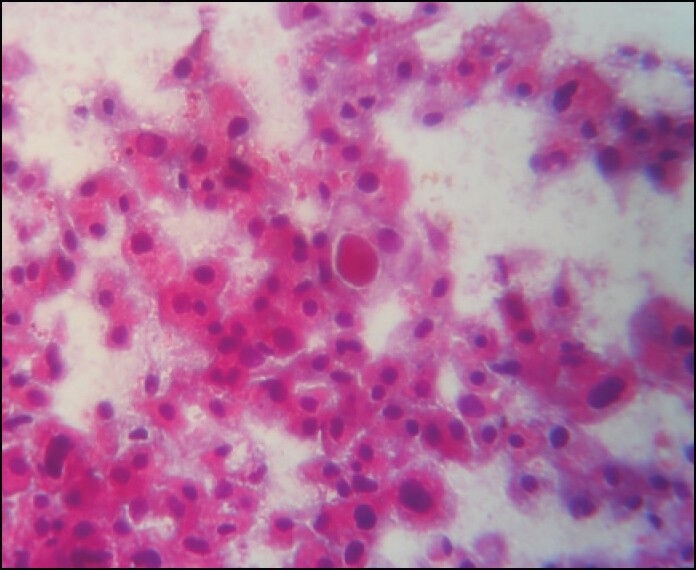
Image-guided aspirations from radiologically diagnosed renal masses yield six cases of conventional renal cell carcinoma (RCC), and one case of transitional cell carcinoma and angiomyolipoma each. One case of papillary variant of RCC was wrongly diagnosed as a benign renal cyst due to the presence of numerous foamy histiocytes aspirated from the stroma. Rest of the aspirates demonstrated loosely cohesive groups of cells with small hyperchromatic nuclei and finely vacuolated cytoplasm [Figure 5]. We also came across one case of chromophobe variant of RCC [Figure 6]. The cytological finding in smear of angiomyolipoma was unsatisfactory consisting of only blood elements.
| Figure 5:Cytology of Renal clear cell carcinoma ×1000
| Figure 6:Cytology of chromophobe renal cell carcinoma ×400
Adrenal lesions
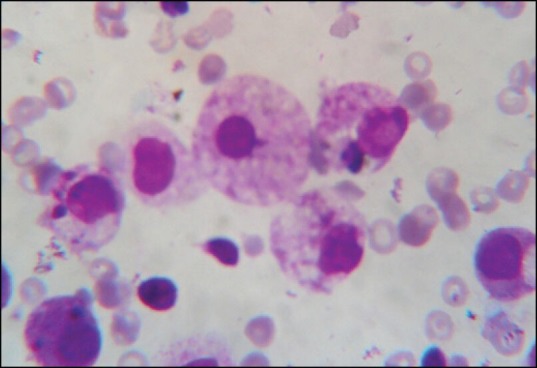
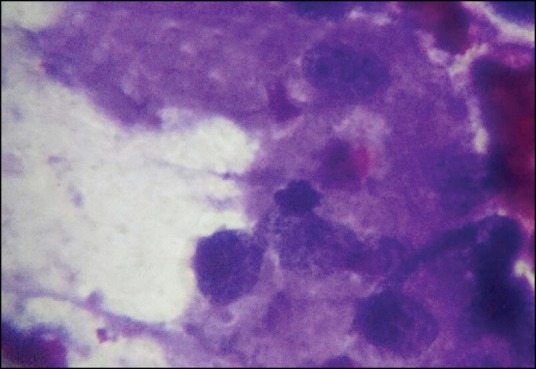
Among the diagnostic smears, three cases were benign lesions and rests were malignant (five cases). Benign lesions included two cases of infectious conditions in the form of adrenal tuberculosis and adrenal histoplasmosis [Figure 7]. We came across only one case of myelolipoma, which showed mature fat containing normal hematopoietic cells on cytological examination.
| Figure 7:Cytology of Histoplasma ×1000
Malignant conditions comprised of both primary and metastatic conditions. Pheochromocytoma and adrenocortical carcinoma were primary malignant lesions. Aspirate from the former one revealed loosely clustered cells with indistinct cell borders and prominent anisokaryosis [Figure 8]. Cytology smears of adrenocortical carcinoma showed large pleomorphic malignant cells singly and in loose groups. Metastatic malignancies consisted of one case of lymphoma, carcinoma and malignant melanoma each.
| Figure 8:Cytology of pheochromocytoma ×400
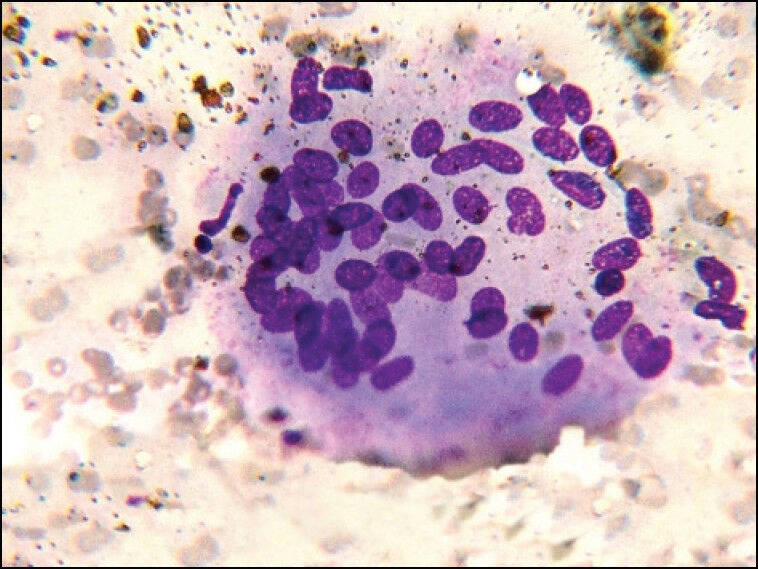
Germ cell tumors
Four cases extragonadal germ cell tumor was grouped under this category comprising of three cases of mature teratoma and one case of seminoma. Aspirates from mature cystic teratoma yielded squamous keratotic debris against a mucoid background. The case of seminoma was diagnosed both on cytology and histology. Cytology smears showed dispersed, uniform, medium-sized cell having delicate chromatin and prominent nucleoli against a tigroid background [Figure 9].
| Figure 9:Cytology of seminoma ×400
Miscellaneous lesions
We observed four cases of pancreatic mass under this category. Smears obtained from two cases demonstrated pleomorphic malignant cells arranged in sheets and acinar pattern. The diagnosis of pancreatic adenocarcinoma was considered. One case of a pseudo-pancreatic cyst showed unsatisfactory smear on cytological examination. Cyto-histopathological correlation was not possible in last case diagnosed as chronic pancreatitis. This case was treated conservatively.
Cyto-histological correlation
Histocytological correlation was done in 31 out of 45 cases. The overall sensitivity in our study to diagnose benign and malignant tumors by cytology is 86% and the specificity is 96% with positive and negative predictive value of 86% and 96%, respectively. Diagnostic accuracy was 93.55% with high statistical significance (P < 0>
DISCUSSION
Image-guided FNAC has facilitated easy collection of cellular material with greater accuracy.[3] Previously inaccessible sites, like retroperitoneal lesions, can be safely sampled and are now routinely aspirated under image guidance to yield cellular material. The assessment of the cellular yield of the specimen by the cytopathologist and increase in the number of sampling by changing the direction of the needle improves the adequacy rate of the technique.[4] Thus, image guidance and presence of on-site pathologist yield smears with better cytomorphological features.[5,6,7,8,9]
In our study, we came across no major complication. Other major studies showed same result.[10,11,12,13]
A total number of 45 cases aged between 15 and 70 years were studied with 62.2% malignant lesions. Miralles et al.,[14] Nagira et al.,[15] Mangal et al.[13] also showed predominance of malignant lesions.
According to radiological and cytologic findings, retroperitoneal lymphadenopathy was the most common finding in our study. These findings were corroborative with the findings from the study by Gangopadhyay et al.[16] Cytological diagnoses in all cases of lymphoma were consistent with histopathological findings achieving diagnostic accuracy of 100%. Better cyto-histological concordance was noted in our study compare to previously reported observation by other authors (80% by Juul et al.[17] and 86% by Droese et al.[18]). The probable explanation was less no of cases were reported by us in present study. Among the benign condition, tuberculous lymphadenopathy was the most common one which corroborates with the finding of Ahmed et al.[12] [Table 4].
Table 4
Statistical results-comparative analysis
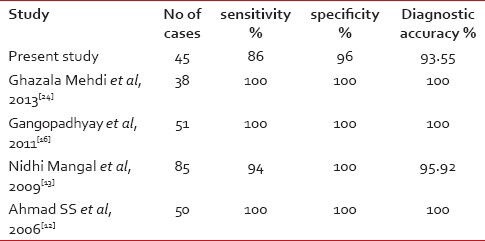
|
The incidence of benign mesenchymal tumor is less than sarcoma and pleomorphic undifferentiated tumor had the highest frequency. Similar finding was also described by Rekhi et al.[19]
Aspirates from RCC showed cytohistological correlation except one case of papillary RCC. Classical cytological features were demonstrated as described by Kristensen et al.[20] and Renshaw et al.[21] Only one case of angiomyolipoma was observed by us in concordance with that reported by Ahmad et al.[12]
Neoplastic adrenal lesions were correctly differentiated from non-neoplastic mass and sub-classified into primary and secondary in our study. Rana et al.[22] also described the role of image-guided FNAC in both benign and malignant adrenal lesions.
We reported only one case of retroperitoneal seminoma which was similar to Tao et al.[23]
The overall sensitivity in our study to diagnose benign and malignant tumors by cytology is 86% and the specificity is 96%. High rates of sensitivity and specificity were recorded by other studies.[12,13]
In present study, the overall diagnostic accuracy of minimally invasive aspiration cytology in retroperitoneal masses is on par with other series.[24] With an accuracy of 93.55% for retroperitoneal lesions, the significance of FNAC as a rapid diagnostic method was established.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Mankin HJ, Lange TA, Spanier SS. The hazards of biopsy in patients with malignant primary bone and soft tissue tumour. J Bone Joint Surg Am 1982;64:1121-7.
- Rajwanshi A, Srinivas R, Upasana G. Malignant small round cell tumors. J Cytol 2009;26:1-10.
- Nobrega J, dos Santos G. Aspiration cytology with fine needle in the abdomen, retroperitoneum and pelvic cavity: A seven year experience of the Portuguese institute of oncology. Eur J Surg Oncol 1994;20:37-42.
- Stewart CJ, Stewart IS. Immediate assessment of fine needle aspiration cytology of lung. J Clin Pathol 1996;49:839-43.
- Orell SR. The diagnosis of solid renal and adrenal masses by aspiration cytology. In: Luciani L, Piscioli F, editors. Aspiration cytology in the staging of urological cancer. Berlin: Springer; 1988. p. 215-23.
- Saboorian MH, Katz RL, Charnsangavej C. Fine needle aspiration cytology of primary and metastatic lesions of the adrenal gland. A series of 188 biopsies with radiologic correlation. Acta Cytol 1995;39:843-51.
- Fassina AS, Borsato S, Fedeli U. Fine needle aspiration cytology (FNAC) of adrenal masses. Cytopathology 2000;11:302-11.
- Zamboni GA, D′Onofrio M, Idili A, Malagò R, Iozzia R, Manfrin E, et al. Ultrasound-guided percutaneous fine-needle aspiration of 545 focal pancreatic lesions. AJR Am J Roentgenol 2009;193:1691-5.
- Akerman M, Rydholm A. Aspiration cytology of lipomatous tumors: A 10-year experience at an orthopedic oncology center. Diagn Cytopathol 1987;3:295-302.
- Guo Z, Kurtycz DF, De Las Casas LE, Hoerl HD. Radiologically guided percutaneous fine-needle aspiration biopsy of pelvic and retroperitoneal masses: A retrospective study of 68 cases. Diagn Cytopathol 2001;25:43-9.
- Sauthier PG, Bélanger R, Provencher DM, Gauthier P, Drouin P. Clinical value of image-guided fine needle aspiration of retroperitoneal masses and lymph nodes in gynecologic oncology Gynecol Oncol 2006;103:75-80.
- Ahmad SS, Akhtar K, Akhtar SS, Nasir A, Khalid M, Mansoor T. Ultrasound guided fine needle aspiration biopsy of retroperitoneal masses. J Cytol 2007;24:41-5.
- Mangal N, Sharma VK, Verma N, Agarwal AK, Sharma SP, Aneja S. Ultrasound guided fine needle aspiration cytology in the diagnosis of retroperitoneal masses: A study of 85 cases. J Cytol 2009;26:97-101.
- Miralles TG, Gosalbez F, Menéndez P, Astudillo A, Torre C, Buesa J. Fine needle aspiration cytology of soft-tissue lesions. Acta Cytol 1986;30:671-8.
- Nagira K, Yamamoto T, Akisue T, Marui T, Hitora T, Nakatani T, et al. Reliability of fine-needle aspiration biopsy in the initial diagnosis of soft-tissue lesions. Diagn Cytopathol 2002;27:354-61.
- Gangopadhyay M, Bhattacharyya NK, Ray S, Chakrabarty S, Pandit N. Guided fine needle aspiration cytology of retroperitoneal masses - Our experience. J Cytol 2011;28:20-4.
- Juul N, Pederson ST, Holm HH. Ultrasonographically guided FNAB of retroperitoneal masses. Br J Radiol 1984;57:43-6.
- Droese M, Altmannsberger M, Kehl A, Lankisch PG, Weiss R, Weber K, et al. Percutaneous FNAB of retroperitoneal masses - accuracy of cytology in the diagnosis of malignancy and cytologic tumour typing. Acta Cytol 1984;28:368-84.
- Rekhi B, Gorad BD, Kakade AC, Chinoy R. Scope of FNAC in the diagnosis of soft tissue tumours-A study from a tertiary cancer referral center in India. Cytojournal 2007;4:20.
- Kristensen JK, Bartels E, Jorgensen HE. Percutaneous renal biopsy under the guidance of ultrasound. Scand J Urol Nephrol 1972;8:223-6.
- Renshaw AA, Granter SR, Cibas ES. Fine-needle aspiration of the adult kidney. Cancer 1997;81:71-88.
- Rana C, Krishnani N, Kumari N. Spectrum of adrenal lesions on fine needle aspiration cytology. Ind J Path and Micro 2012;55:461-6.
- Tao LC, Negin ML, Donat E. Primary retroperitoneal seminoma diagnosed by FNAB - a case report. Acta Cytol 1984;28: 598-600.
- Mehdi G, Maheshwari V, Afzal S, Ansari H, Ahmad I. Image-guided fine-needle aspiration of retroperitoneal masses: The role of the cytopathologist. J Cytol 2013;30:36-41.
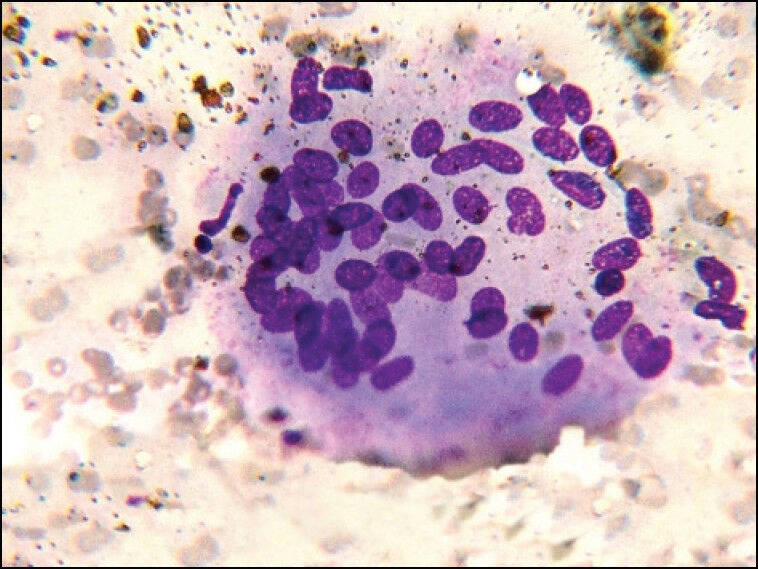
| Figure 1:Cytology of granuloma ×400
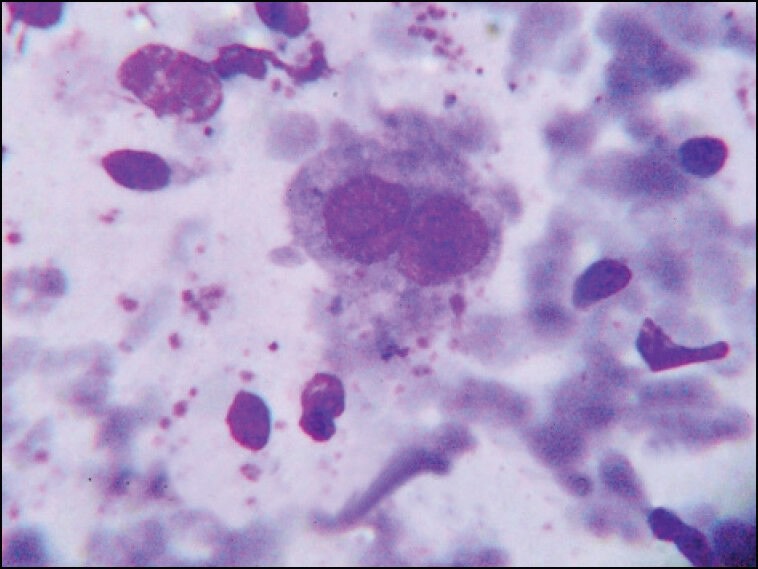
| Figure 2:Cytology of Hodgkins disease ×1000
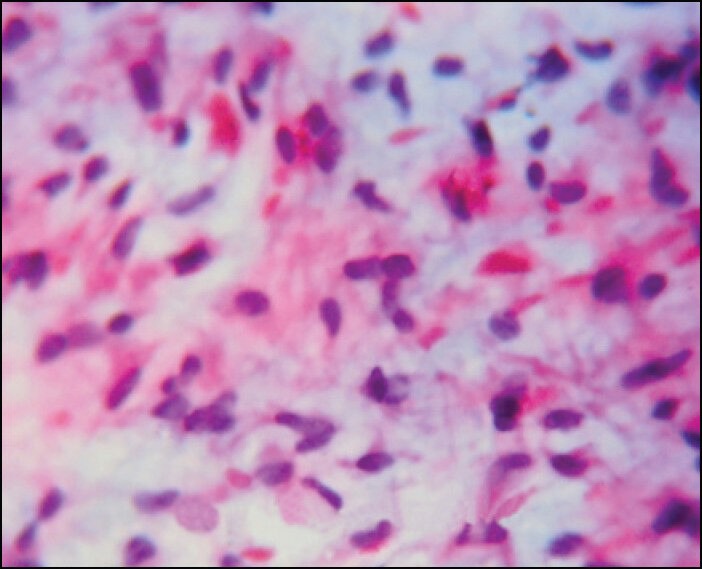
| Figure 3:Cytology of myxoid tumor ×400
| Figure 4:Cytology of malignant spindle cell tumor ×400
| Figure 5:Cytology of Renal clear cell carcinoma ×1000
| Figure 6:Cytology of chromophobe renal cell carcinoma ×400
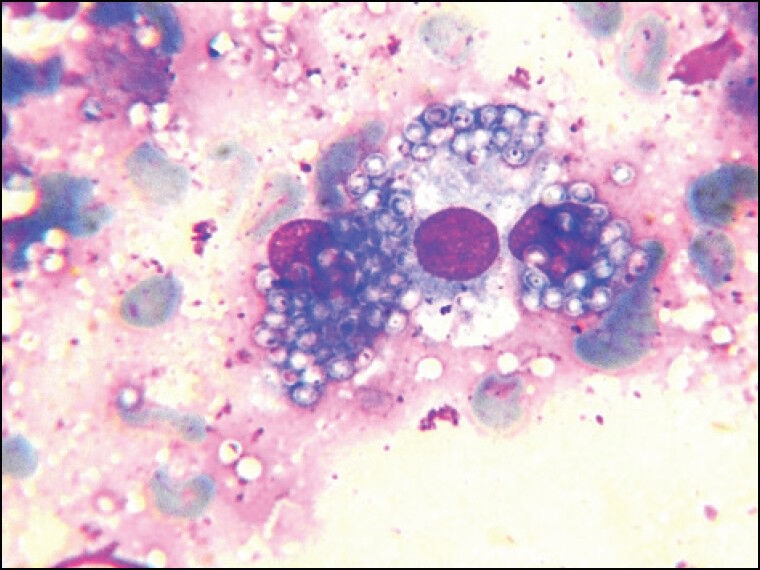
| Figure 7:Cytology of Histoplasma ×1000
| Figure 8:Cytology of pheochromocytoma ×400
| Figure 9:Cytology of seminoma ×400
References
- Mankin HJ, Lange TA, Spanier SS. The hazards of biopsy in patients with malignant primary bone and soft tissue tumour. J Bone Joint Surg Am 1982;64:1121-7.
- Rajwanshi A, Srinivas R, Upasana G. Malignant small round cell tumors. J Cytol 2009;26:1-10.
- Nobrega J, dos Santos G. Aspiration cytology with fine needle in the abdomen, retroperitoneum and pelvic cavity: A seven year experience of the Portuguese institute of oncology. Eur J Surg Oncol 1994;20:37-42.
- Stewart CJ, Stewart IS. Immediate assessment of fine needle aspiration cytology of lung. J Clin Pathol 1996;49:839-43.
- Orell SR. The diagnosis of solid renal and adrenal masses by aspiration cytology. In: Luciani L, Piscioli F, editors. Aspiration cytology in the staging of urological cancer. Berlin: Springer; 1988. p. 215-23.
- Saboorian MH, Katz RL, Charnsangavej C. Fine needle aspiration cytology of primary and metastatic lesions of the adrenal gland. A series of 188 biopsies with radiologic correlation. Acta Cytol 1995;39:843-51.
- Fassina AS, Borsato S, Fedeli U. Fine needle aspiration cytology (FNAC) of adrenal masses. Cytopathology 2000;11:302-11.
- Zamboni GA, D′Onofrio M, Idili A, Malagò R, Iozzia R, Manfrin E, et al. Ultrasound-guided percutaneous fine-needle aspiration of 545 focal pancreatic lesions. AJR Am J Roentgenol 2009;193:1691-5.
- Akerman M, Rydholm A. Aspiration cytology of lipomatous tumors: A 10-year experience at an orthopedic oncology center. Diagn Cytopathol 1987;3:295-302.
- Guo Z, Kurtycz DF, De Las Casas LE, Hoerl HD. Radiologically guided percutaneous fine-needle aspiration biopsy of pelvic and retroperitoneal masses: A retrospective study of 68 cases. Diagn Cytopathol 2001;25:43-9.
- Sauthier PG, Bélanger R, Provencher DM, Gauthier P, Drouin P. Clinical value of image-guided fine needle aspiration of retroperitoneal masses and lymph nodes in gynecologic oncology Gynecol Oncol 2006;103:75-80.
- Ahmad SS, Akhtar K, Akhtar SS, Nasir A, Khalid M, Mansoor T. Ultrasound guided fine needle aspiration biopsy of retroperitoneal masses. J Cytol 2007;24:41-5.
- Mangal N, Sharma VK, Verma N, Agarwal AK, Sharma SP, Aneja S. Ultrasound guided fine needle aspiration cytology in the diagnosis of retroperitoneal masses: A study of 85 cases. J Cytol 2009;26:97-101.
- Miralles TG, Gosalbez F, Menéndez P, Astudillo A, Torre C, Buesa J. Fine needle aspiration cytology of soft-tissue lesions. Acta Cytol 1986;30:671-8.
- Nagira K, Yamamoto T, Akisue T, Marui T, Hitora T, Nakatani T, et al. Reliability of fine-needle aspiration biopsy in the initial diagnosis of soft-tissue lesions. Diagn Cytopathol 2002;27:354-61.
- Gangopadhyay M, Bhattacharyya NK, Ray S, Chakrabarty S, Pandit N. Guided fine needle aspiration cytology of retroperitoneal masses - Our experience. J Cytol 2011;28:20-4.
- Juul N, Pederson ST, Holm HH. Ultrasonographically guided FNAB of retroperitoneal masses. Br J Radiol 1984;57:43-6.
- Droese M, Altmannsberger M, Kehl A, Lankisch PG, Weiss R, Weber K, et al. Percutaneous FNAB of retroperitoneal masses - accuracy of cytology in the diagnosis of malignancy and cytologic tumour typing. Acta Cytol 1984;28:368-84.
- Rekhi B, Gorad BD, Kakade AC, Chinoy R. Scope of FNAC in the diagnosis of soft tissue tumours-A study from a tertiary cancer referral center in India. Cytojournal 2007;4:20.
- Kristensen JK, Bartels E, Jorgensen HE. Percutaneous renal biopsy under the guidance of ultrasound. Scand J Urol Nephrol 1972;8:223-6.
- Renshaw AA, Granter SR, Cibas ES. Fine-needle aspiration of the adult kidney. Cancer 1997;81:71-88.
- Rana C, Krishnani N, Kumari N. Spectrum of adrenal lesions on fine needle aspiration cytology. Ind J Path and Micro 2012;55:461-6.
- Tao LC, Negin ML, Donat E. Primary retroperitoneal seminoma diagnosed by FNAB - a case report. Acta Cytol 1984;28: 598-600.
- Mehdi G, Maheshwari V, Afzal S, Ansari H, Ahmad I. Image-guided fine-needle aspiration of retroperitoneal masses: The role of the cytopathologist. J Cytol 2013;30:36-41.


 PDF
PDF  Views
Views  Share
Share

