Eosinophilic Liver Abcesses and Pyrexia of Unknown Origin in Idiopathic Hypereosinphilic Syndrome: Myeloproliferative or Mimic?
CC BY-NC-ND 4.0 ? Indian J Med Paediatr Oncol 2018; 39(01): 111-113
DOI: DOI: 10.4103/ijmpo.ijmpo_25_16
Abstract
We report a case which presented with pyrexia of unknown origin (PUO) with eosinophilia and multiple hypoechoic lesions in the liver resembling secondaries. After secondary causes were ruled out, aspiration of liver lesions revealed eosinophilic abcesses. A diagnosis of idiopathic hypereosinophilic syndrome (HES) was made and the patient responded to steroid therapy. HES remains a diagnosis of exclusion. HES presenting with PUO and liver abcesses is very rare. A high index of suspicion is required to recognize the involvement of different organ systems due to HES.
Keywords
Hypereosinophilic syndrome - liver abcess - pyrexia of unknown originPublication History
Article published online:
23 June 2021
? 2018. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
We report a case which presented with pyrexia of unknown origin (PUO) with eosinophilia and multiple hypoechoic lesions in the liver resembling secondaries. After secondary causes were ruled out, aspiration of liver lesions revealed eosinophilic abcesses. A diagnosis of idiopathic hypereosinophilic syndrome (HES) was made and the patient responded to steroid therapy. HES remains a diagnosis of exclusion. HES presenting with PUO and liver abcesses is very rare. A high index of suspicion is required to recognize the involvement of different organ systems due to HES.
Keywords
Hypereosinophilic syndrome - liver abcess - pyrexia of unknown originIntroduction
Hypereosinophilic syndrome (HES) is a heterogeneous group of uncommon diseases characterized by marked peripheral blood hypereosinophilia with evidence of eosinophil mediated end organ damage. HES is a diagnosis of exclusion and is considered only when the secondary causes of eosinophilia have been eliminated. Clinical manifestations usually cannot be differentiated from other causes of eosinophilia, and symptoms depend on the organ involved. Hepatic involvement in HES is uncommon. Here, we report an unusual presentation of HES with pyrexia of unknown origin (PUO) and isolated hepatic eosinophilic abscesses mimicking hepatic metastases.
Case Report
A 28-year-old homemaker presented to us with high-grade intermittent fever for 4 months with right upper abdominal pain for 2 weeks. She complained of decreased appetite with significant loss of weight in the previous 5 months. She had no history about other organ systems. She had no history of tuberculosis hypertension or diabetes. She had no history of high-risk sexual behavior or addictions; no history of previous hospitalization or history of contact with animals.
On examination, she was febrile with tender hepatomegaly. There was no pallor, icterus, cyanosis, clubbing, lymphadenopathy, or edema. The respiratory and cardiovascular examination were normal, with no neurological deficit.
Investigations showed Hb 10.9 g/dl, total leukocyte count - 16,000, with 40% eosinophils, absolute eosinophil count being 6400. Platelet count was normal. Liver transaminases were elevated serum glutamic oxaloacetic transaminase (47 IU/L) and serum glutamic pyruvic transaminase (80 IU/L). Kidney function tests were normal. Hepatitis B, hepatitis C, HIV I and II, ANA was negative. Malarial and microfilarial antigens were negative; blood culture showed no growth after 48 h, urine and stool examination showed no abnormality. Chest X-ray was normal. Ultrasound abdomen revealed multiple hypoechoic, cystic lesions in both lobes of the liver. The patient was given empirical intravenous antibiotics, with which leukocytosis normalized, but eosinophilia> 1500 and fever persisted.
A contrast enhanced computed tomography abdomen showed multiple hypoechogenic hepatic lesions, with a moth-eaten appearance resembling extensive hepatic metastases [Figure 1]. An ultrasound guided liver biopsy was taken which was suggestive of extensive infiltration of hepatic parenchyma with eosinophils, with areas of eosinophilic abscesses. There was no evidence of granuloma, atypical cells or parasitic body. Liver abscess aspirate for fungal culture was negative. She was given a 14-day course of albendazole, to which there was no response. Due to the endemicity of filariasis, a full course of diethylcarbamazine was also tried. Upper gastrointestinal endoscopy and bronchoscopy with cytology of bronchoalveolar lavage were unremarkable. Bone marrow aspirate showed increased eosinophilic precursors, with no evidence of increased blasts or granuloma. Fungal smear and Ziehl?Neelsen stain of bone marrow aspirate was negative. Echocardiography was unremarkable
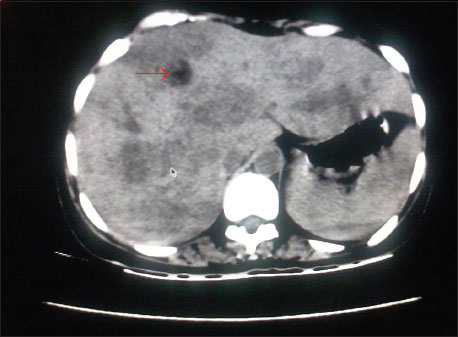
|?Figure.1Contrast-enhanced computed tomography abdomen showing right lobe liver abcess
Thus, reactive causes for persistent eosinophilia were ruled out. As there were <5>
On follow-up after a month, the patient was afebrile with an absolute eosinophil count of 340, mild hepatomegaly and no radiological evidence of hepatic cysts. The patient was thus a case of PUO due to HES with eosinophilic liver abscesses.
Discussion
The idiopathic hypereosinphilic syndrome was described first in 1975 by Chusid?et al.[1] The initial approach for this degree of eosinophilia is to rule out secondary causes of eosinophilia, namely, parasitic infestations, drug hypersensitivity reactions, allergic disorders, neoplasms such as lymphoma, leukemia, connective tissue disorders such as Churg-Strauss disease, hypoadrenalism, and eosinophilic pneumonia. When a secondary cause for eosinophilia is not found after thorough investigations, it is necessary to consider a diagnosis of HES.[2],[3] Recent studies have led to the formulation of two major variants of HES. The first being a myeloproliferative variant (M-HES); manifested by features such as hepatosplenomegaly, anemia, thrombocytopenia, circulating myeloid precursors, and increased serum Vitamin B-12 levels. This is characterized by the expression of the FIP1-like 1/platelet-derived growth factor receptor ? fusion protein, an activated tyrosine kinase causing clonal expansion of eosinophils. Cytogenetic remission is generally achieved with Imatinib.[4] The other variant of HES is lymphocytic, with cutaneous manifestations, polyclonal eosinophilic expansion due to deregulated T cells causing interlukin-5 overproduction.[5] This variant is managed with high dose corticosteroids.[2]
However, the majority of cases of HES fall in neither category of HES. In such cases, management is determined by the clinical presentation and the degree of organ damage. Corticosteroids form the first line of management for decreasing the eosinophil count. Second-line steroid sparing agents include hydroxyurea and imatinib.
Our case was unusual in several respects. In our patient, the majority of the secondary causes were ruled out. She showed a remarkable response to steroids with complete remission of fever, eosinophilia, and radiological disappearance of hepatic abscesses. There have been reported cases with a similar presentation, but the eosinophilia was due to visceral larva migrans, caused by toxocara larva.[6],[7] Such cases responded well to antihelminthic therapy and showed clinical worsening with corticosteroids.
HES involves tissue infiltration of eosinophils, with activation, degranulation and release of preformed mediators causing tissue damage. Usually, skin, gastrointestinal tract, heart, and the nervous system are affected. HES presenting as isolated hepatic eosinophilic abscesses is rare.[8],[9] The radiological appearance of the eosinophilic abscesses resembled hepatic metastases, which was another unusual finding in our case.[10]
HES is an uncommon differential diagnosis in a case of PUO with eosinophilia. A thorough evaluation is necessary to rule out the secondary causes of eosinophilia and the primary eosinophilic disorders like eosinophilic pneumonia and eosinophilic gastroenteritis. Organ damage due to eosinophil infiltration can be extensive and can present as isolated hepatic involvement. Corticosteroids form the first line of management. The radiological appearance of eosinophilic hepatic abscesses can be misleading and can mimic malignancy. Hence, needle biopsy is essential for diagnosis.
Conflict of Interest
There are no conflicts of interest.
References
- husid MJ, Dale DC, West BC, Wolff SM.?The hypereosinophilic syndrome: Analysis of fourteen cases with review of the literature. Medicine (Baltimore) 1975; 54: 1-27
- oufosse F, Weller PF.?Practical approach to the patient with hypereosinophilia. J Allergy Clin Immunol 2010; 126: 39-44
- lion AD.?How I treat hypereosinophilic syndromes. Blood 2009; 114: 3736-41
- ools J, DeAngelo DJ, Gotlib J, Stover EH, Legare RD, Cortes J.?et al.?A tyrosine kinase created by fusion of the PDGFRA and FIP1L1 genes as a therapeutic target of imatinib in idiopathic hypereosinophilic syndrome. N Engl J Med 2003; 348: 1201-14
- oufosse F, Cogan E, Goldman M.?Lymphocytic variant hypereosinophilic syndromes. Immunol Allergy Clin North Am 2007; 27: 389-413
- aplan KJ, Goodman ZD, Ishak KG.?Eosinophilic granuloma of the liver: A characteristic lesion with relationship to visceral larva migrans. Am J Surg Pathol 2001; 25: 1316-21
- im JH, Lee KS.?Eosinophilic infiltration in Korea: Idiopathic?. Korean J Radiol 2006; 7: 4-6
- ng KA, Remotti H, Olsson R.?Eosinophilic hepatic necrosis in hypereosinophilic syndrome. J Clin Gastroenterol 2000; 31: 323-7
- keda H, Katayanagi K, Kurumaya H, Sato Y, Sasaki M.?et al.?A case of hypereosinophilia-associated multiple mass lesions of liver showing non-granulomatous eosinophilic hepatic necrosis. Gastroenterology Res 2011; 4: 168-73
- Won JH, Kim MJ, Kim BN, Ji H, Chung JJ, Yoo HS.?et al.?Focal eosinophilic infiltration of the liver: A mimick of hepatic metastasis. Abdom Imaging 1999; 24: 369-72
Address for correspondence
Publication History
23 June 2021
? 2018. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2,
Noida-201301 UP, India
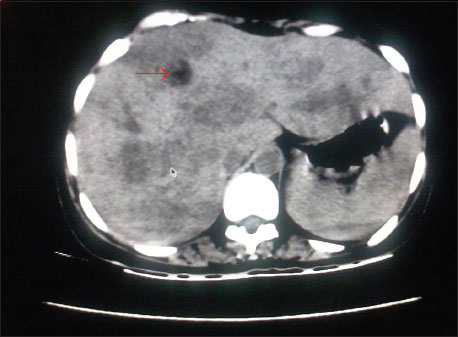
|?Figure.1Contrast-enhanced computed tomography abdomen showing right lobe liver abcess
References
- husid MJ, Dale DC, West BC, Wolff SM.?The hypereosinophilic syndrome: Analysis of fourteen cases with review of the literature. Medicine (Baltimore) 1975; 54: 1-27
- oufosse F, Weller PF.?Practical approach to the patient with hypereosinophilia. J Allergy Clin Immunol 2010; 126: 39-44
- lion AD.?How I treat hypereosinophilic syndromes. Blood 2009; 114: 3736-41
- ools J, DeAngelo DJ, Gotlib J, Stover EH, Legare RD, Cortes J.?et al.?A tyrosine kinase created by fusion of the PDGFRA and FIP1L1 genes as a therapeutic target of imatinib in idiopathic hypereosinophilic syndrome. N Engl J Med 2003; 348: 1201-14
- oufosse F, Cogan E, Goldman M.?Lymphocytic variant hypereosinophilic syndromes. Immunol Allergy Clin North Am 2007; 27: 389-413
- aplan KJ, Goodman ZD, Ishak KG.?Eosinophilic granuloma of the liver: A characteristic lesion with relationship to visceral larva migrans. Am J Surg Pathol 2001; 25: 1316-21
- im JH, Lee KS.?Eosinophilic infiltration in Korea: Idiopathic?. Korean J Radiol 2006; 7: 4-6
- ng KA, Remotti H, Olsson R.?Eosinophilic hepatic necrosis in hypereosinophilic syndrome. J Clin Gastroenterol 2000; 31: 323-7
- keda H, Katayanagi K, Kurumaya H, Sato Y, Sasaki M.?et al.?A case of hypereosinophilia-associated multiple mass lesions of liver showing non-granulomatous eosinophilic hepatic necrosis. Gastroenterology Res 2011; 4: 168-73
- Won JH, Kim MJ, Kim BN, Ji H, Chung JJ, Yoo HS.?et al.?Focal eosinophilic infiltration of the liver: A mimick of hepatic metastasis. Abdom Imaging 1999; 24: 369-72


 PDF
PDF  Views
Views  Share
Share

