Extranodal testicular anaplastic versus plasmablastic plasma cell tumor: A rare case with diagnostic dilemma in a developing country
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2011; 32(01): 49-54
DOI: DOI: 10.4103/0971-5851.81892
Abstract
Primary testicular plasmacytoma is rare, especially when occurring in the absence of a previous or concurrent diagnosis of multiple myeloma. An 84-year-old gentleman was admitted with complaints of swelling over the right side of scrotum for the past 2 months. Local examination revealed a 10×15 cm tense and tender swelling involving the right scrotum. Therefore, high orchidectomy with excision of hemiscrotum was done. The histopathology revealed testicular plasmacytoma, which was positive for CD 138.
Publication History
Article published online:
16 August 2021
© 2011. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Primary testicular plasmacytoma is rare, especially when occurring in the absence of a previous or concurrent diagnosis of multiple myeloma. An 84-year-old gentleman was admitted with complaints of swelling over the right side of scrotum for the past 2 months. Local examination revealed a 10×15 cm tense and tender swelling involving the right scrotum. Therefore, high orchidectomy with excision of hemiscrotum was done. The histopathology revealed testicular plasmacytoma, which was positive for CD 138.
INTRODUCTION
There are various causes for testicular swelling namely hernia, hydrocele, hematoma, testicular torsion, varicocele, germ cell tumors, and lymphomas. Extramedullary plasmacytoma (EMP) of testes is uncommon.[1] The prognosis of EMP involving the testis is much better than multiple myeloma (MM) involving the testis. Herein we present a case of an 84-year-old man who was diagnosed with testicular plasmacytoma due to its rarity and paucity of literature regarding its management.
CASE REPORT
An 84-year-old gentleman was admitted with complaints of swelling over the right side of scrotum for the past 2 months. The swelling was progressive in nature and was also associated with pain. It was not reducing on lying down. No history of fever or trauma. Patient gave a history of hemorrhoids and angioplasty done 8 years ago. Patient gives no other history of comorbid illness such as tuberculosis, diabetes mellitus, or hypertension.
On examination, performance status according to Eastern Cooperative Oncological Group[2] , Scoring was 2; all the vital parameters were normal. Local examination revealed a 10×15 cm tense, firm, and tender swelling involving the right scrotum. On palpation, the swelling was not reducible. One could get above the swelling. Testicular sensation was lost on the left side. The opposite side testis was normal. A computed tomography scan of the abdomen and pelvis showed heterogeneous soft tissue right testicular mass, which was measuring 10×6×5 cm in size with some evidence of necrosis within the right testicles and there were right inguinal lymph nodes [Figure 1]. At this time, the differential diagnosis was infected hydrocele/pyocele or organized hematoma was entertained. Preoperatively complete blood count, serum biochemistry, and thyroid function tests were normal; viral serology (retroviral and Epstein bar virus) was negative. Beta human chorionic gonadotropin and alpha-fetoprotein values were normal. Hence, he was taken up for surgery. Per-operatively, he seemed to have tumor testes infiltrating the scrotal wall. Therefore, high orchidectomy with excision of hemiscrotum was done. The opinions from four different pathologists were sought. The histopathology gave a differential diagnosis of testicular tumor with scrotal sac wall infiltration/diffuse large cell non-Hodgkins immunoblastic/anaplastic lymphoma; poorly differentiated carcinoma in favor of embryonal carcinoma; poorly differentiated malignant tumor most consistent with plasmacytoma. Immunohistochemistry showed Vimentin, CD30, CD 138 Lambda chains positive, increased Ki 67, EMA, CD79a, S100P positive, in favor of anaplastic plasmacytoma [Figures 2 ((aa–k) and 3 ((aa–i)]. EBER, cyclin D1, MiB1, and CD 56 were not done due to logistic reasons. In the meanwhile, workup for MM was done, which showed normal serum electrophoresis and β2 microglobulin level. Urine was negative for Bence Jones protein. Tc99m Bone scan and bone marrow reports were normal. After a lapse of 2 months due to the diagnostic dilemma, treatment was started for plasmacytoma with daily tab – thalidomide 100 mg weekly tab, dexamethasone 40 mg daily tab, melphalan 5 mg twice daily for 5 days. The patient has completed six cycles of chemotherapy and is in remission.
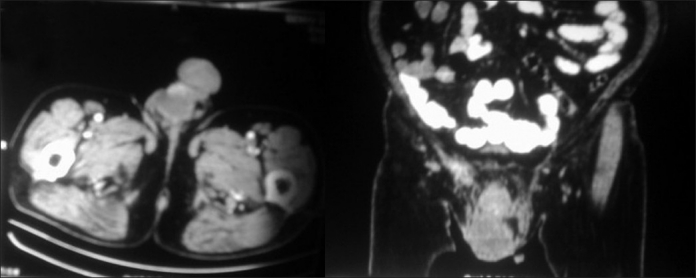
| Fig. 1 (a)Testicular plasmacytoma CT scan axial section preoperative picture showing right testicular mass. b: Testicular plasmacytoma CT scan coronal section preoperative picture showing right testicular mass
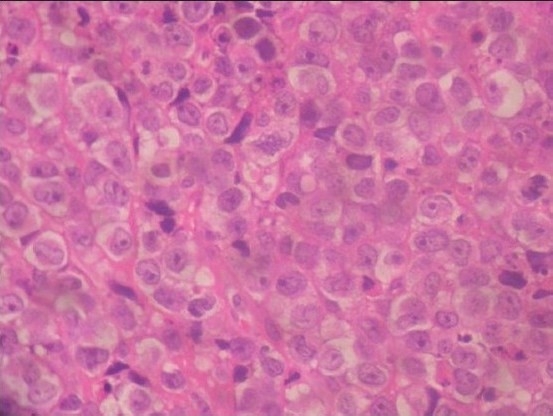
| Fig. 2a H and E
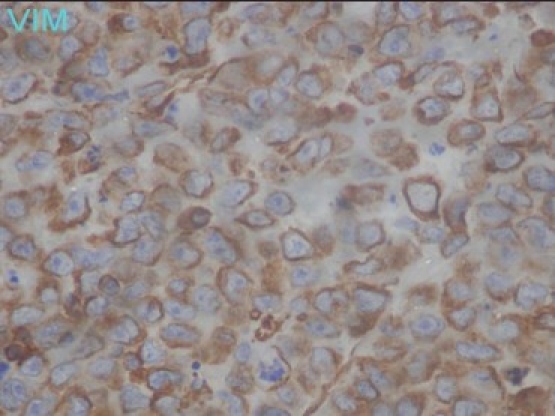
| Fig. 2k Vimentin positive
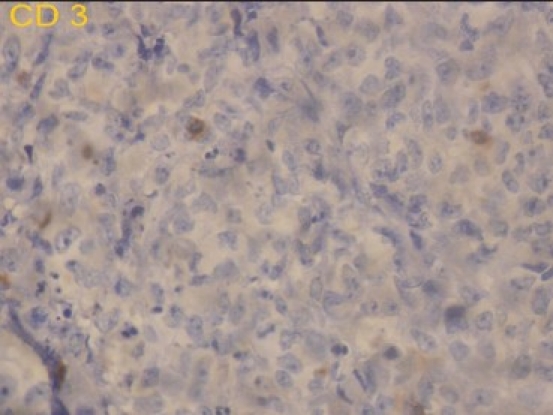
| Fig. 3a CD 3 negative
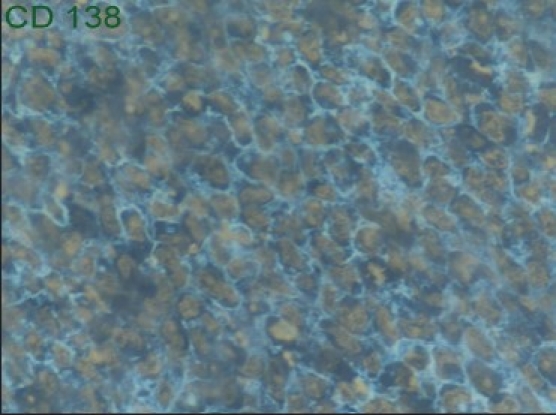
| Fig. 3i CD 138 positive
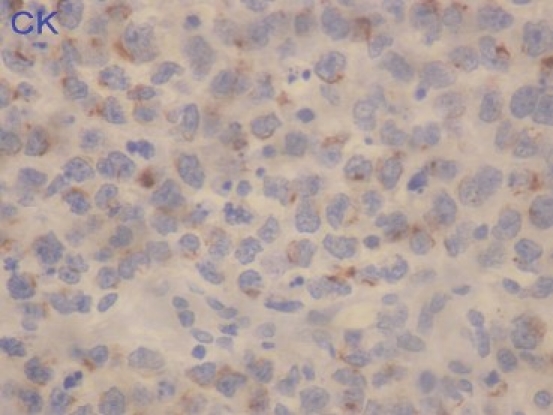
| Fig. 2b Cytokeratin
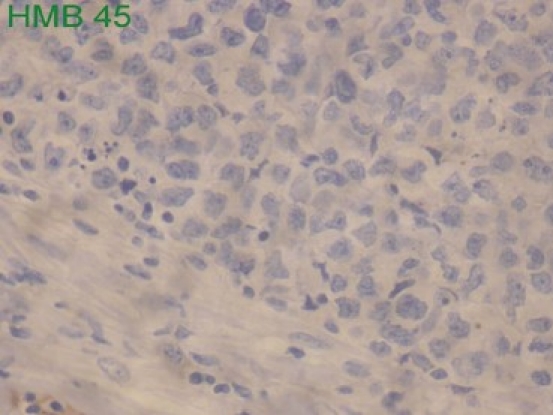
| Fig. 2c HMB 45 negative
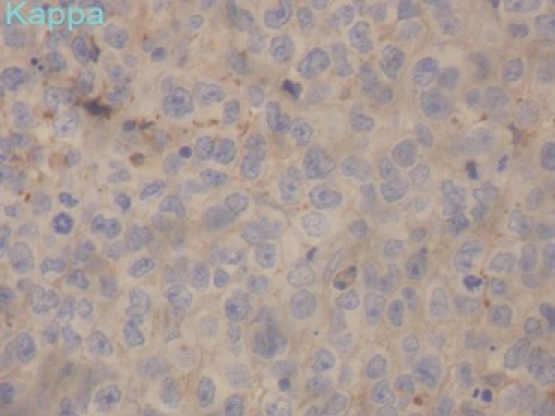
| Fig. 2d Kappa negative
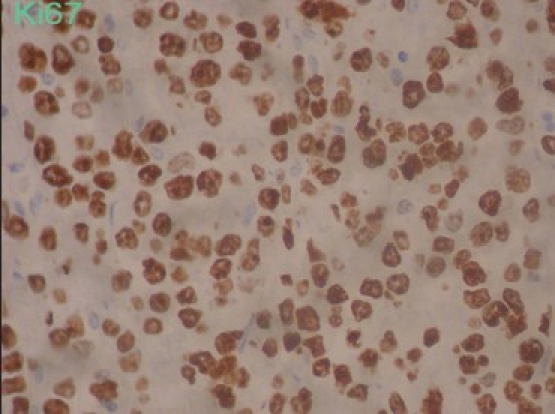
| Fig. 2e Ki 67 +90
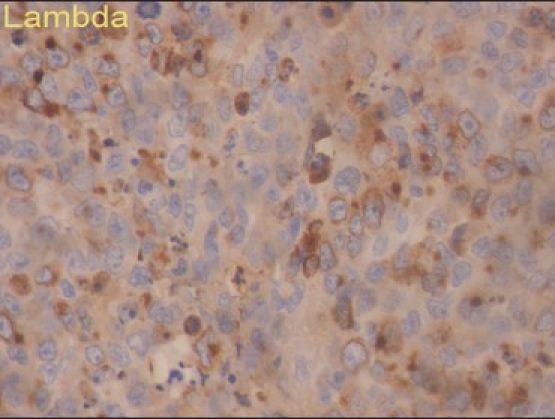
| Fig. 2f Lambda positive
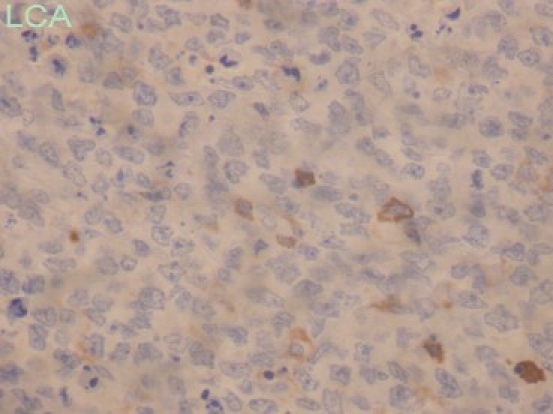
| Fig. 2g LCA negative
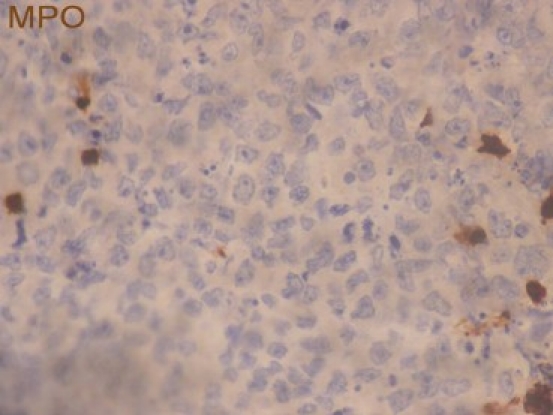
| Fig. 2h MPO negative
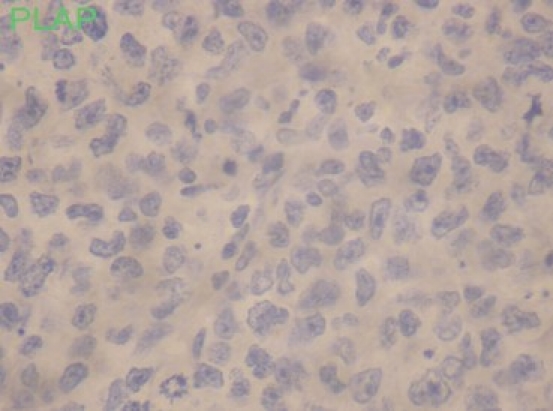
| Fig. 2i PLAP negative
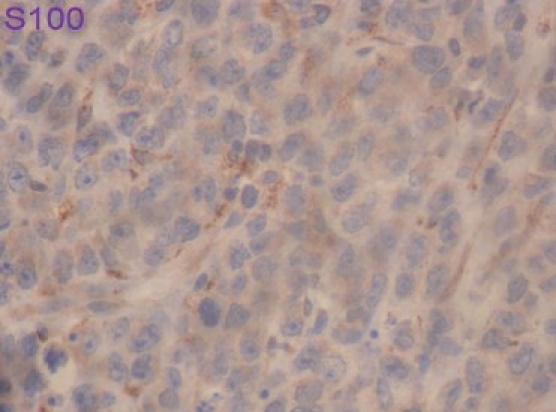
| Fig. 2j S 100 negative
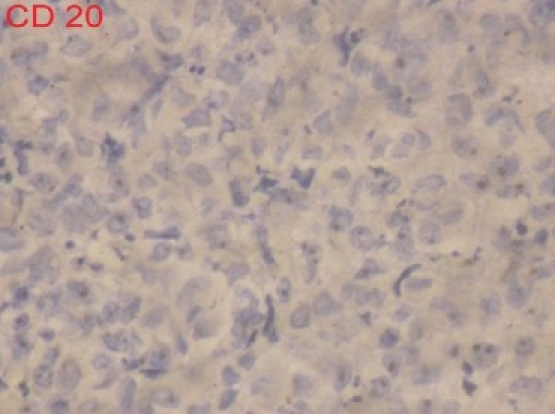
| Fig. 3b CD 20 negative
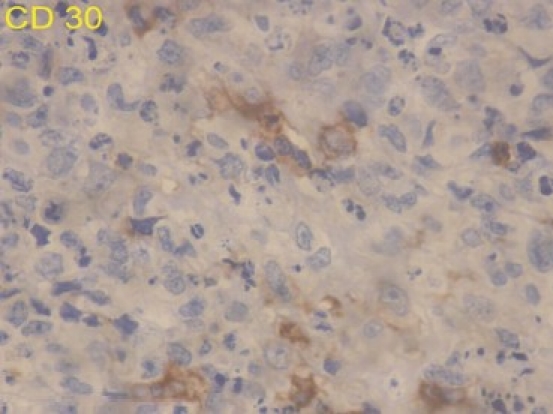
| Fig. 3c CD 30 focal positive
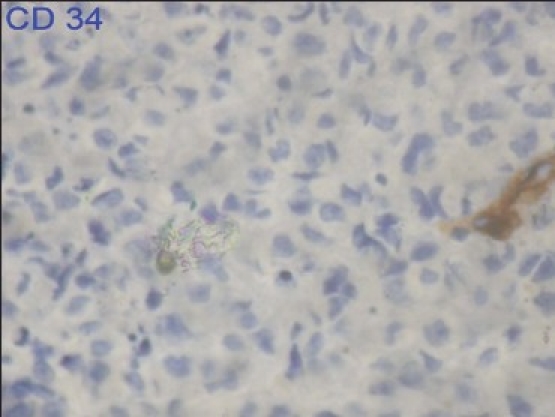
| Fig. 3d CD 34 negative
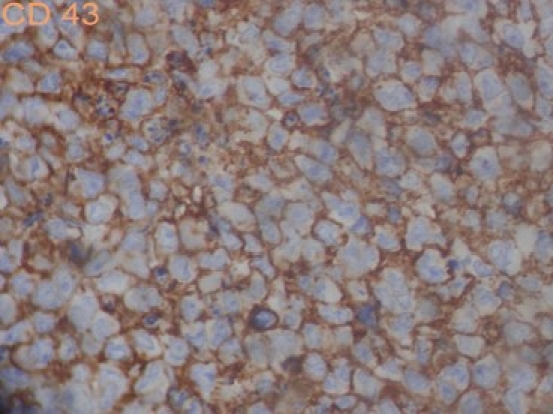
| Fig. 3e CD 43 positive
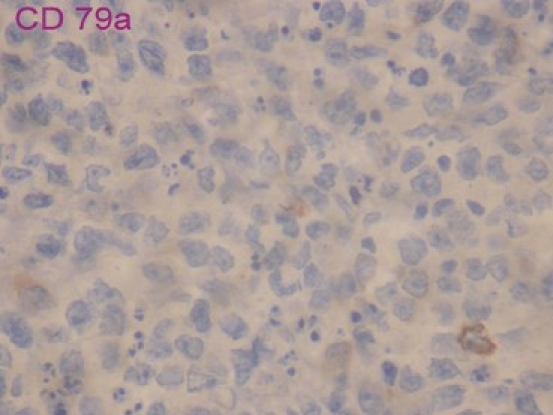
| Fig. 3f CD 79a negative
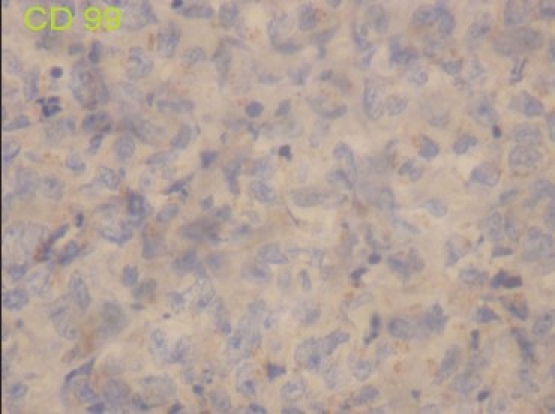
| Fig. 3g CD 99 negative
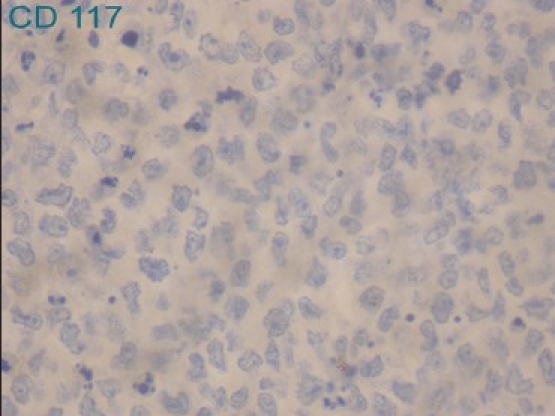
| Fig. 3h CD 117 negative
DISCUSSION
EMP originating from the testis is called primary testicular plasmacytoma. Testicular plasmacytoma presenting with MM invading testis is called secondary testicular plasmacytoma. Primary MM, the neoplasm of monoclonal plasmocytes, is mainly located in the bone marrow, but neoplastic cells may generally and frequently invade other tissues and organs, such as the liver, lung, spleen, pancreas, kidney, lymph nodes, digestive tract, thyroid, heart, testis, ovary, and skin.[3,4] EMP occur most commonly in the nasopharyngeal area; the other frequently involved sites include the liver, spleen, lymph nodes, and kidneys, although involvement of nearly every organ and tissue in the body by myeloma cells has been reported.[3,4] Testicular plasmacytoma is a rare cause of intratesticular neoplasia. Only seven cases among 6000 testicular and peritesticular primary and secondary tumors on file at the Armed Forces Institute of Pathology in 1970 have been reported.[5] Only 52 total cases of testicular plasmacytoma published between 1939 and 2002.[6] Most of these cases had previous or concurrent MM or EMP. Cases of solitary testicular plasmacytoma at onset are few, with about 17 reported cases.[6] Many of these initially solitary lesions progressed to MM. To our knowledge, fewer than 10 cases of primary testicular plasmacytoma did not progress to MM, with variable periods of follow-up.[6] Along term observation for about at least 1 year may be essential to determine the primary or secondary nature of an EMP, although MM can develop years later.[7] Perhaps more importantly, this finding may herald the diagnosis of concurrent or subsequent MM. The incidence of testis plasmacytoma accounted 0.03% of all testicular neoplasms, and 0.6% of all MM types.[6] EMP originates from other extramedullary tissues with a male predilection (3:1=male: female) and accounts for < 4% of malignant plasma cell tumors.[8,9] The criteria for diagnosis of EMP are as follows: (1) biopsy demonstrates a single extramedullary site of the plasmacytoma, with or without involvement of lymphoid tissue, and without changes to the skeleton (which may exclude the possibility of MM); (2) bone marrow aspiration reveals < 5% plasmacytes; and (3) other parameters of the bone marrow are normal.
Patients with EMP need follow-up after orchiectomy. If EMP involves other tissues or organs, radiotherapy should be considered first, as EMP is hypersensitive to radiotherapy. When confined lymph nodes are involved in EMP, radiotherapy should be performed in an extended field. Radio-resistant or recurrent and residual foci after radiotherapy should be treated with surgery. For tumors with recurrence metastasis, radiotherapy or surgery is recommended.[10] The prognosis of EMP is relatively good. The 5-year survival reaches 50–70%. In case of plasmablastic plasma cell tumor, the clinical course is very aggressive with most of the patients dying in the first year of diagnosis.[11,12] However in this case the patient has survived more than 2 years; hence through the clinical history and survival data we conclude that this patient is diagnosed to have anaplastic testicular plasmacytoma. Primary testicular plasmacytoma now has turned out to be an important, though a rare, differential diagnosis of elderly individuals with testicular swelling. No consensus for the treatment modalities has been arrived as yet due to the paucity of literature on management details.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
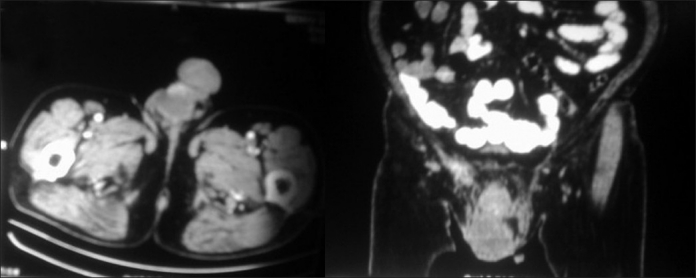
| Fig. 1 (a)Testicular plasmacytoma CT scan axial section preoperative picture showing right testicular mass. b: Testicular plasmacytoma CT scan coronal section preoperative picture showing right testicular mass
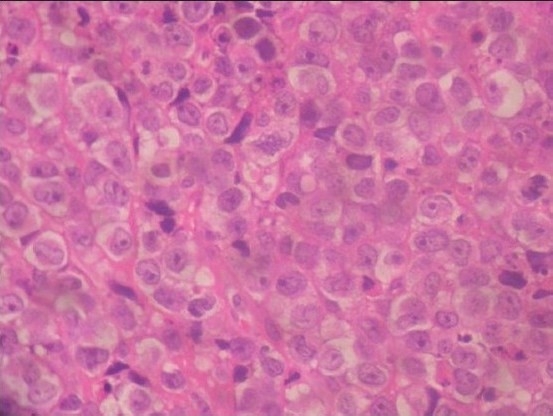
| Fig. 2a H and E
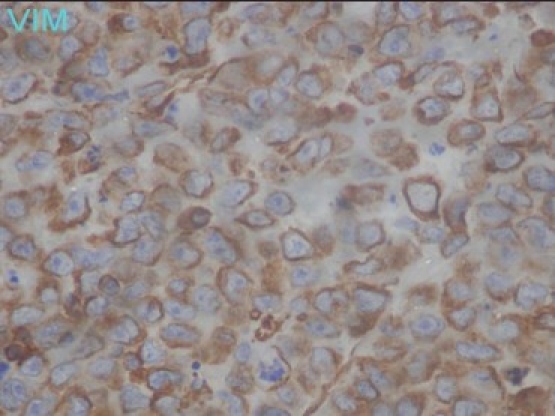
| Fig. 2k Vimentin positive
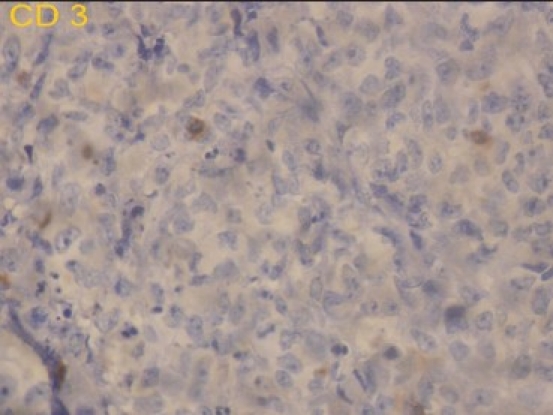
| Fig. 3a CD 3 negative
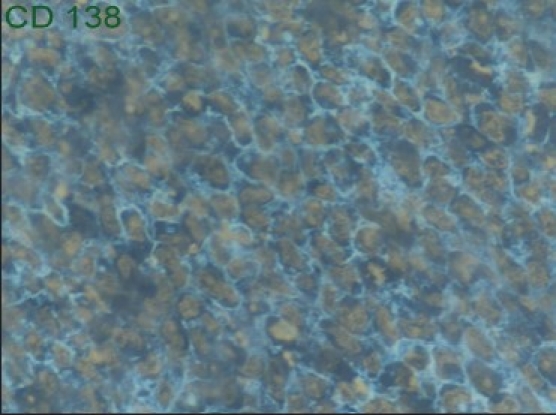
| Fig. 3i CD 138 positive
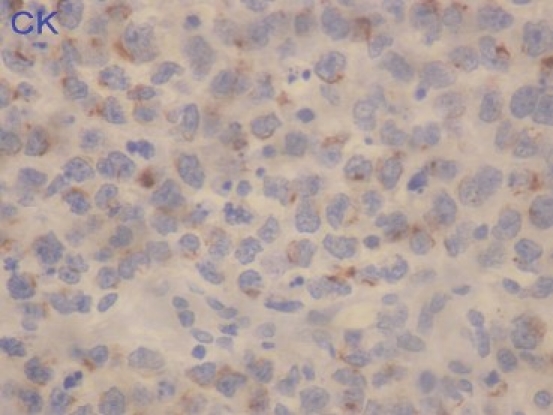
| Fig. 2b Cytokeratin
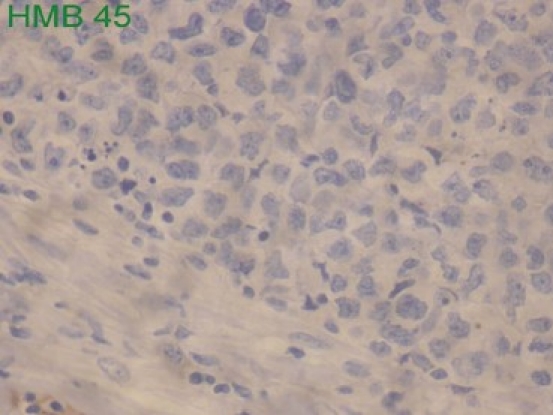
| Fig. 2c HMB 45 negative
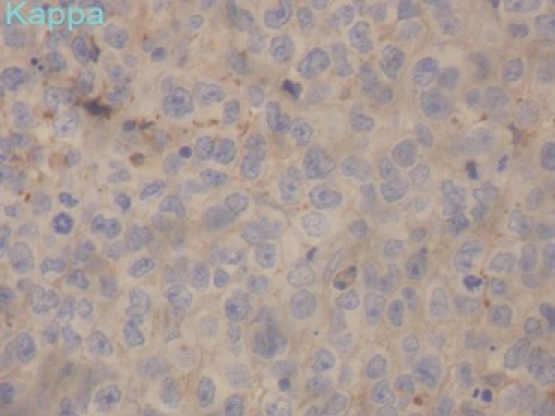
| Fig. 2d Kappa negative
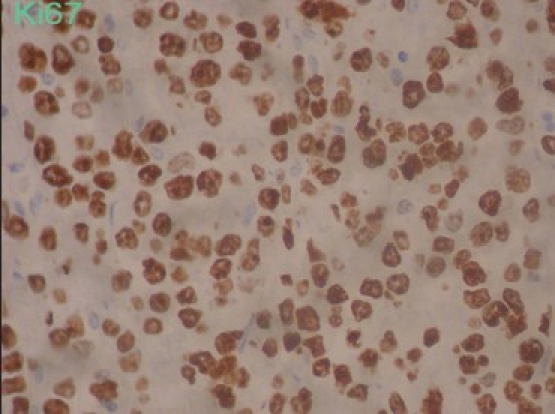
| Fig. 2e Ki 67 +90
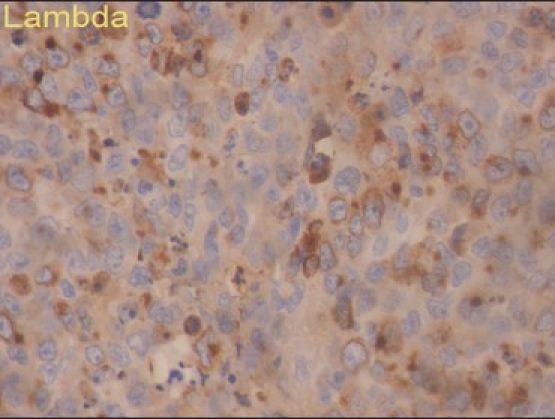
| Fig. 2f Lambda positive
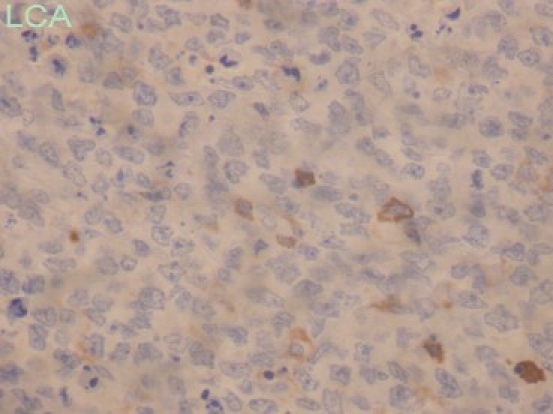
| Fig. 2g LCA negative
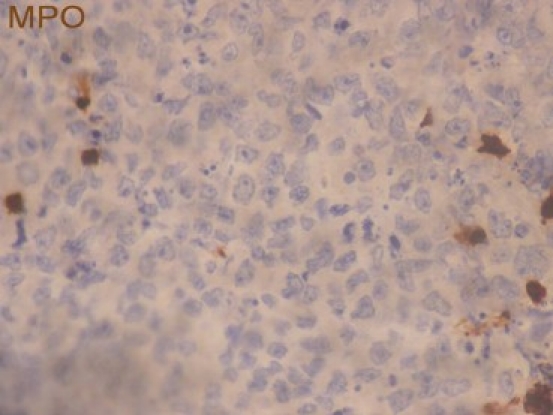
| Fig. 2h MPO negative
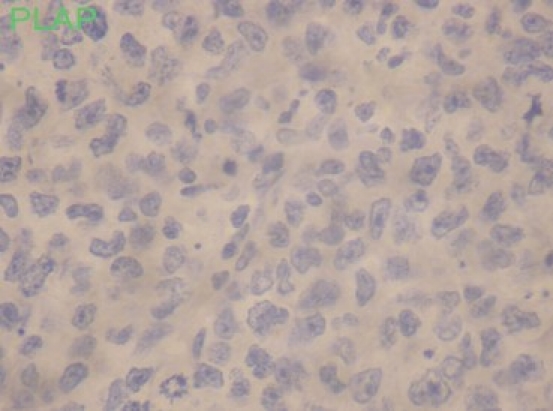
| Fig. 2i PLAP negative
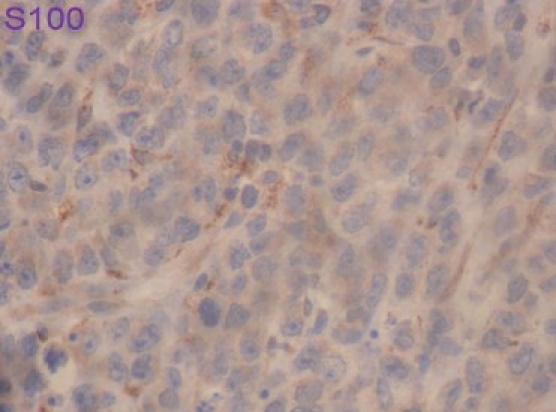
| Fig. 2j S 100 negative
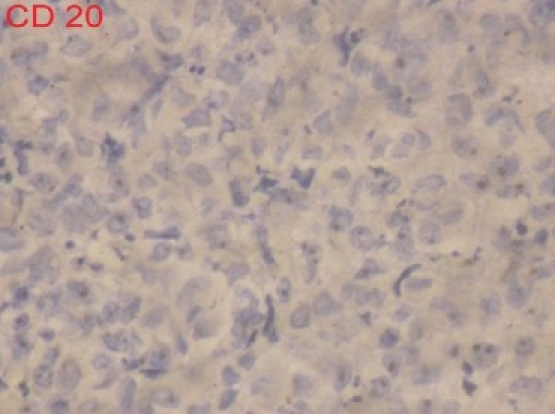
| Fig. 3b CD 20 negative
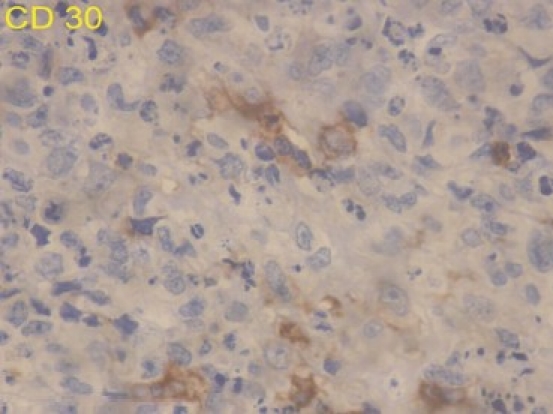
| Fig. 3c CD 30 focal positive
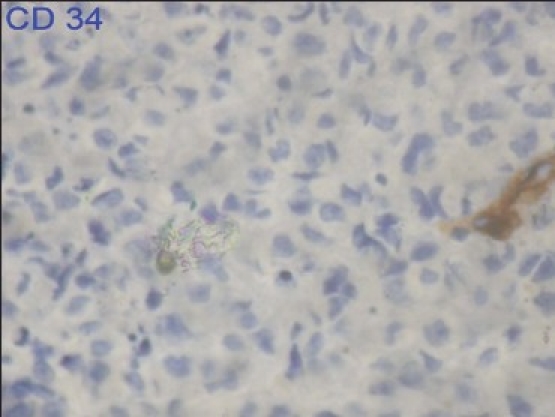
| Fig. 3d CD 34 negative
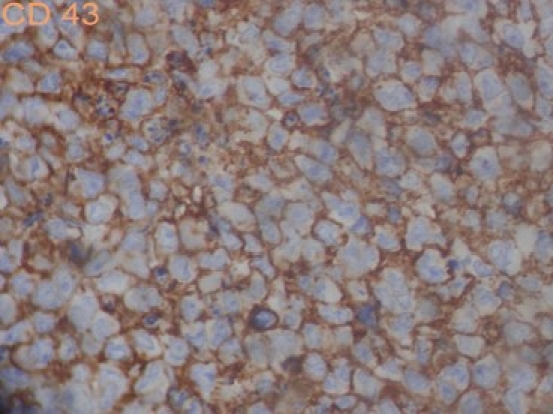
| Fig. 3e CD 43 positive
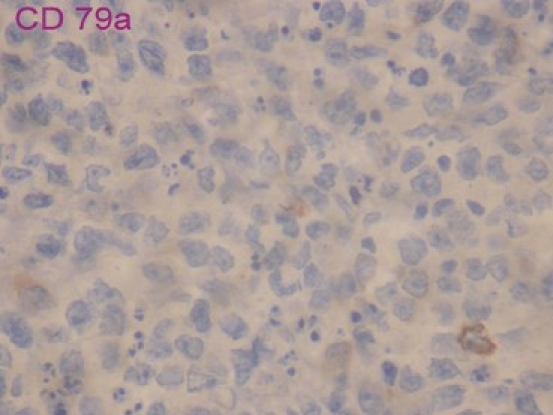
| Fig. 3f CD 79a negative
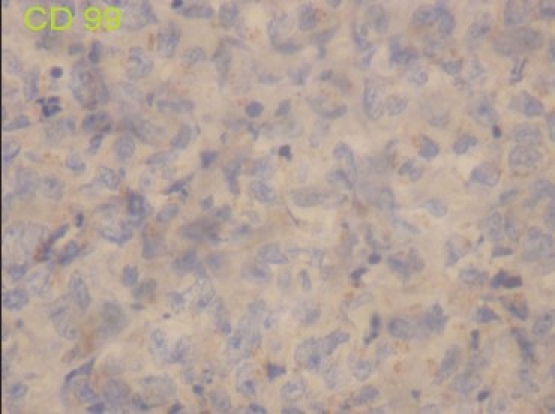
| Fig. 3g CD 99 negative
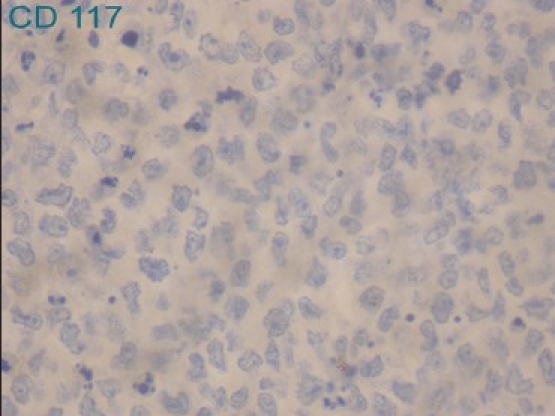
| Fig. 3h CD 117 negative


 PDF
PDF  Views
Views  Share
Share

