Longitudinally Extensive Transverse Myelitis as Presenting Manifestation of Lung Adenocarcinoma
CC BY-NC-ND 4.0 ? Indian J Med Paediatr Oncol 2018; 39(01): 106-108
DOI: DOI: 10.4103/ijmpo.ijmpo_55_16
Abstract
Longitudinally extensive transverse myelitis (LETM) is an unusual manifestation of systemic malignancy. It has been mainly reported with lung cancers and lymphoproliferative malignancy. LETM in systemic malignancy can be caused by either intramedullary metastases or paraneoplastic syndrome. Occurrence of LETM as the first manifestation of malignancy has been rarely reported. We present clinical, laboratory, and imaging findings of a 66-year-old man with nonsmall-cell lung (adeno) carcinoma, who presented with LETM without having any cardinal manifestations of lung malignancy. The rarity of the disease and especially such a presentation can cause considerable delay in the diagnosis and treatment.
Publication History
23 June 2021
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Longitudinally extensive transverse myelitis (LETM) is an unusual manifestation of systemic malignancy. It has been mainly reported with lung cancers and lymphoproliferative malignancy. LETM in systemic malignancy can be caused by either intramedullary metastases or paraneoplastic syndrome. Occurrence of LETM as the first manifestation of malignancy has been rarely reported. We present clinical, laboratory, and imaging findings of a 66-year-old man with nonsmall-cell lung (adeno) carcinoma, who presented with LETM without having any cardinal manifestations of lung malignancy. The rarity of the disease and especially such a presentation can cause considerable delay in the diagnosis and treatment.
Keywords
Longitudinally extensive transverse myelitis - lung adenocarcinoma - systemic malignancy
Introduction
Longitudinally extensive transverse myelitis (LETM) is a term used to describe confluent lesions extending more than three spinal cord segments. LETM has a broad differential diagnosis, and etiologies include autoimmune, infectious, parainfectious, metabolic, and neoplastic causes.[1] However, the most common causes of LETM are inflammatory demyelinating diseases such as neuromyelitis optica and postinfectious encephalomyelitis. LETM as a presenting feature of systemic malignancy has been rarely reported.[2],[3] We herein report a case of nonsmall-cell lung carcinoma (CA) in a 66-year-old male, who presented with LETM without having any cardinal features of lung malignancy.
Case Report
A 66-year-old male without any comorbidity, chronic smoker presented with difficulty in walking for 4 months, insidious onset gradually progressing, bedbound for 3 weeks with urinary retention 2 weeks back for which he was catheterized. There was also history of fever for the past 5 days with altered sensorium for the past 3 days. There was also history of weight loss and anorexia. There was no history of trauma or seizures or vomiting or headache or diminution of vision or cough or hemoptysis or back/neck pain or any sensory symptom. On general examination, pulse rate was 110 bpm, blood pressure 130/90 mmHg, respiratory rate 18/min, and temperature 38.3?C.
On neurological examination, he was drowsy but arousable, cranial nerve examination was normal. On motor examination, there was hypertonia in all four limbs with motor power medical research council (MRC) grade 3/5 in the upper limbs and 2/5 in the lower limbs. Deep tendon reflexes were brisk in both the upper and lower limbs. Plantars were extensor bilaterally. Sensory system could not be accurately assessed as the patient was drowsy. Neck stiffness was present. Examination of other systems was normal.
Routine investigations including hematology, biochemistry, and electrocardiogram were normal. X-ray chest was grossly normal. Magnetic resonance imaging (MRI) brain revealed age-related atrophy and ischemic demyelination [Figure 1]. MRI spine revealed myelitis involving entire length of the spinal cord right from lower medulla up to lumbar region [Figure 1]. Cerebrospinal fluid (CSF) examination revealed cell count: 4 (L 100%), protein: 359.8, glucose: 29, and adenosine deaminase assay: 0.5 with negative microbiologic results. CSF malignant cells were positive. CSF Siemsa and Papanicolaou stain revealed tumor cells with vacuolated cytoplasm, dense chromatin, and prominent nucleoli. CSF thyroid transcription factor-1 nuclear positivity suggested malignancy of pulmonary origin. CSF cytokeratin positivity revealed tumor of epithelial origin [Figure 2]. CSF paraneoplastic neuronal autoantibody profile (Ma, Hu, Ri, Yo, and Amphiphysin) was also sent which was negative. Whole-body positron emission tomography-computed tomography was planned which revealed fluorodeoxyglucose (FDG)-avid nodular mass lesion in apical segment of the right upper lung with FDG-avid mediastinal lymph nodes [Figure 3]. It also revealed increased FDG uptake in the cervical and upper thoracic spinal cord [Figure 3]. Bronchoscopy-guided biopsy was taken which revealed adeno CA lung [Figure 4]. Hence, the final diagnosis was nonsmall-cell (adeno CA) CA lung presenting as carcinomatous meningitis and LETM. Oncology consultation was sought and he was advised for intrathecal chemotherapy and whole-brain radiation, but the patient self-discharged against medical advice and did not return for outpatient follow-up appointments.{Figure 1}{Figure 2}{Figure 3}{Figure 4}
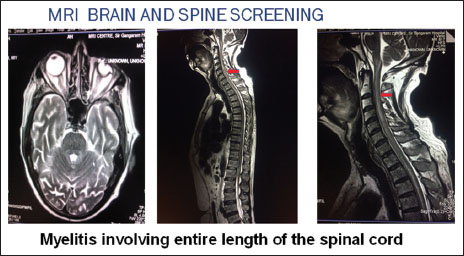
|?Figure.1Myelitis involving entire length of spinal cord
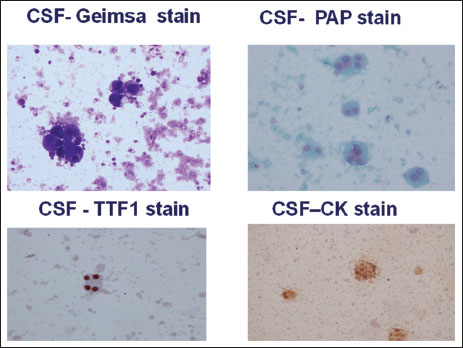
|?Figure.2Various cerebrospinal fluid stains
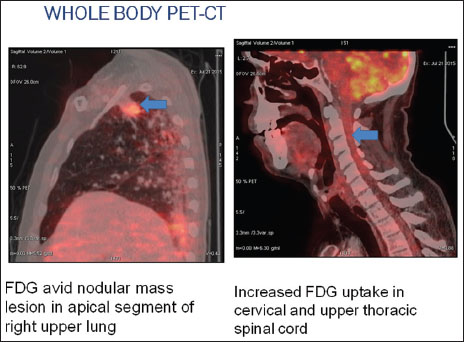
|?Figure.3Whole-body positron emission tomography-computed tomography revealing fluorodeoxyglucose-avid nodular mass lesion in apical segment of the right upper lung
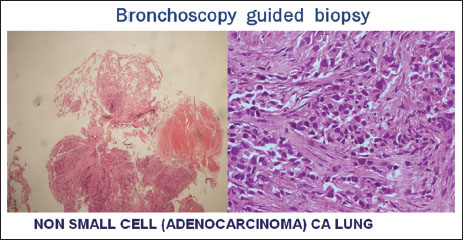
|?Figure.4Bronchoscopy-guided biopsy suggestive of lung adenocarcinoma
Discussion
Neoplastic diseases can cause long-segment myelitis through intramedullary metastases, intramedullary tumor, such as ependymoma, intravascular lymphoma, and paraneoplastic syndrome.[4] LETM due to intramedullary spinal cord metastases (ISCM) is very rare. ISCM is seen in only 0.1%?0.4% of patients of neoplastic diseases.[4] The common underlying malignancies are lung, breast, renal cell CAs and melanoma.[5],[6] The literature on ISCM is limited to case reports, relatively small case series, literature reviews, and autopsy series.[7]
As for the development of ISCMs, several pathophysiologic mechanisms have been described, including arterial spread, retrograde venous spread (through Batson venous plexus), meningeal spread, perineural lymphatic spread, and direct invasion from a contiguous structure.[8],[9] Of these proposed mechanisms for the pathogenesis of ISCMs, spread through the arterial route is generally favored as the most common though the mechanism may differ, depending on the primary tumor cell type.
There is no definitive evidence existing with regard to the therapy of choice in patients with ISCM. Conservative approaches including radiation and chemotherapy have been adopted more widely because of the common presence of other systemic diseases. The use of radiation treatment with or without concomitant steroids is frequently described in the literature. Radiation therapy usually halts the growth of the tumor and provides stabilization of further neurological deterioration. However, its efficacy may be limited to patients with radiosensitive tumors such as lymphoma, breast cancer, and small-cell lung CA. Prognosis is poor, with an overall median survival of 4 months from the time of diagnosis.[5]
Paraneoplastic myelitis usually occurs in association with the involvement of other areas of the nervous system; examples include encephalitis, sensory neuronopathy, chorea, and optic neuropathy. Most patients present clinically with an insidiously progressive myelopathy with fewer patients presenting subacutely over a few weeks and even fewer with a relapsing remitting course. It has been postulated that the underlying malignancy and part of the involved nervous system share common antigens, thereby mounting an autoimmune response. Several antibodies such as CRMP-5, VGCC, amphiphysin, ganglionic acetylcholine receptor, VGKC, and ANNA-1,2 have been associated with paraneoplastic spinal cord lesions. Associated antibodies most frequently detected are anti-Hu, anti-CRMP5/CV2, and less frequently, anti-amphiphysin antibodies. The usual culprit is small-cell lung cancer.[10]
Conclusion
This case highlights the importance of recognizing the broad differential diagnosis of LETM. LETM is a rare presenting manifestation of malignancy. When an elderly patient comes with LETM, possibility of any underlying malignancy should always be sought with thorough workup, as the demyelinating diseases are rare in this age group.
Conflict of Interest
There are no conflicts of interest.
References
- itley JL, Leite MI, George JS, Palace JA.?The differential diagnosis of longitudinally extensive transverse myelitis. Mult Scler 2012; 18: 271-85
- jeda VJ.?Necrotizing myelopathy associated with malignancy. A clinicopathologic study of two cases and literature review. Cancer 1984; 53: 1115-23
- ain RS, Gupta PK, Agrawal R, Tejwani S, Kumar S.?Longitudinally extensive transverse myelitis as presenting manifestation of small cell carcinoma lung. Oxf Med Case Reports 2015; 2015: 208-10
- hargava P, Elble RJ.?Clinical reasoning: An unusual cause of transverse myelitis?. Neurology 2014; 82: e46-50
- ung WS, Sung MJ, Chan JH, Manion B, Song J, Dubey A.?et al.?Intramedullary spinal cord metastases: A 20-year institutional experience with a comprehensive literature review. World Neurosurg 2013; 79: 576-84
- ishioka K, Tanaka R, Tsutsumi S, Shimura H, Oji Y, Saeki H.?et al.?Longitudinally extensive transverse myelitis with intramedullary metastasis of small-cell lung carcinoma: An autopsy case report. Case Rep Neurol Med 2013; 2013: 305670
- elaid I, Jlassi H, Debbiche G, Rais H, Ben AyedF.?Lung adenocarcinoma with intramedullary spinal cord metastasis: A case report and review of the literature. Rev Pneumol Clin 2013; 69: 149-51
- atanabe M, Nomura T, Sato M, Mochida J.?Intramedullary spinal cord metastasis: A clinical and imaging study of seven patients. J Spinal Disord Tech 2006; 19: 43-7
- shii T, Terao T, Komine K, Abe T.?Intramedullary spinal cord metastases of malignant melanoma: An autopsy case report and review of the literature. Clin Neuropathol 2010; 29: 334-40
- Kannoth S.?Paraneoplastic neurologic syndrome: A practical approach. Ann Indian Acad Neurol 2012; 15: 6-12
Address for correspondence
Publication History
23 June 2021
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
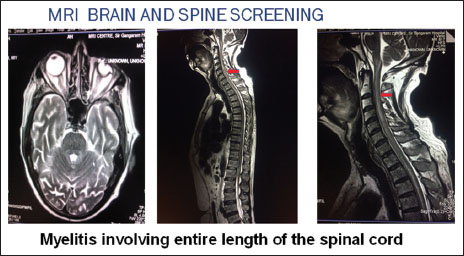
|?Figure.1Myelitis involving entire length of spinal cord
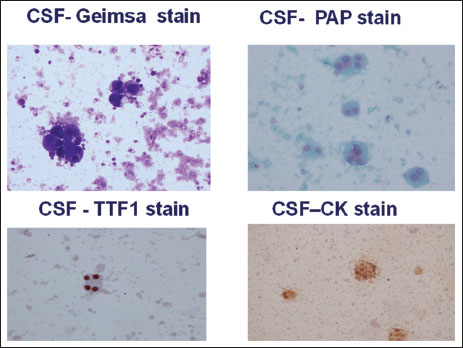
|?Figure.2Various cerebrospinal fluid stains
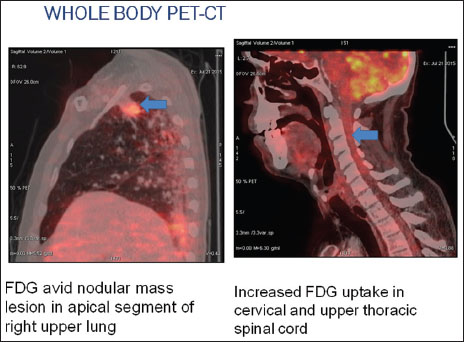
|?Figure.3Whole-body positron emission tomography-computed tomography revealing fluorodeoxyglucose-avid nodular mass lesion in apical segment of the right upper lung
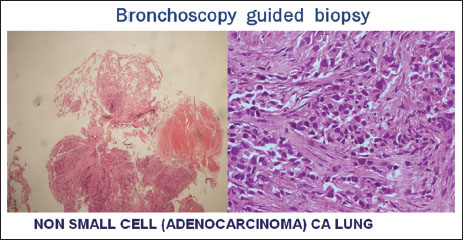
|?Figure.4Bronchoscopy-guided biopsy suggestive of lung adenocarcinoma
References
- itley JL, Leite MI, George JS, Palace JA.?The differential diagnosis of longitudinally extensive transverse myelitis. Mult Scler 2012; 18: 271-85
- jeda VJ.?Necrotizing myelopathy associated with malignancy. A clinicopathologic study of two cases and literature review. Cancer 1984; 53: 1115-23
- ain RS, Gupta PK, Agrawal R, Tejwani S, Kumar S.?Longitudinally extensive transverse myelitis as presenting manifestation of small cell carcinoma lung. Oxf Med Case Reports 2015; 2015: 208-10
- hargava P, Elble RJ.?Clinical reasoning: An unusual cause of transverse myelitis?. Neurology 2014; 82: e46-50
- ung WS, Sung MJ, Chan JH, Manion B, Song J, Dubey A.?et al.?Intramedullary spinal cord metastases: A 20-year institutional experience with a comprehensive literature review. World Neurosurg 2013; 79: 576-84
- ishioka K, Tanaka R, Tsutsumi S, Shimura H, Oji Y, Saeki H.?et al.?Longitudinally extensive transverse myelitis with intramedullary metastasis of small-cell lung carcinoma: An autopsy case report. Case Rep Neurol Med 2013; 2013: 305670
- elaid I, Jlassi H, Debbiche G, Rais H, Ben AyedF.?Lung adenocarcinoma with intramedullary spinal cord metastasis: A case report and review of the literature. Rev Pneumol Clin 2013; 69: 149-51
- atanabe M, Nomura T, Sato M, Mochida J.?Intramedullary spinal cord metastasis: A clinical and imaging study of seven patients. J Spinal Disord Tech 2006; 19: 43-7
- shii T, Terao T, Komine K, Abe T.?Intramedullary spinal cord metastases of malignant melanoma: An autopsy case report and review of the literature. Clin Neuropathol 2010; 29: 334-40
- Kannoth S.?Paraneoplastic neurologic syndrome: A practical approach. Ann Indian Acad Neurol 2012; 15: 6-12


 PDF
PDF  Views
Views  Share
Share

