Profile of Primary Pediatric Brain and Spinal Cord Tumors from North India
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2017; 38(01): 10-14
DOI: DOI: 10.4103/0971-5851.203514
Abstract
Background and Objective: The study was carried out to find the profile of pediatric brain and spinal cord tumors during 2006–2015 in a tertiary referral center of North India. Materials and Methods: It was a retrospective medical record-based observational study. All children <18 class="b" xss=removed>Results: Central nervous system (CNS) tumors constituted 5.6% of all pediatric solid malignancies in our hospital. A total of 54 brain tumors and 13 spinal cord tumors were studied. Medulloblastoma was the most common brain tumor (20.3%) followed by pilocytic astrocytoma (16.6%) and glioblastoma multiforme (9.2%). The most common spinal cord tumor was Ewing's sarcoma/primitive neuroectodermal tumor (30.7%) followed by ependymoma (23%). Mean age was 10.5 years and 12.1 years for brain and spinal cord tumors, respectively. There was male predominance in brain tumors while the sex ratio was almost equal in spinal cord tumors. Histomorphologically, necrosis and angiogenesis were associated with higher grades of tumor. Approximately 35% children were alive after a mean follow-up of 36 ± 6 months. Conclusion: Compared with most international studies, we found a higher percentage of medulloblastoma in the brain, thus stressing the role of regional and ethnic influences in the pathogenesis of CNS tumors.
Publication History
Article published online:
06 July 2021
© 2017. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Background and Objective:
The study was carried out to find the profile of pediatric brain and spinal cord tumors during 2006–2015 in a tertiary referral center of North India.
Materials and Methods:
It was a retrospective medical record-based observational study. All children <18>
Results:
Central nervous system (CNS) tumors constituted 5.6%-of all pediatric solid malignancies in our hospital. A total of 54 brain tumors and 13 spinal cord tumors were studied. Medulloblastoma was the most common brain tumor (20.3%) followed by pilocytic astrocytoma (16.6%) and glioblastoma multiforme (9.2%). The most common spinal cord tumor was Ewing's sarcoma/primitive neuroectodermal tumor (30.7%) followed by ependymoma (23%). Mean age was 10.5 years and 12.1 years for brain and spinal cord tumors, respectively. There was male predominance in brain tumors while the sex ratio was almost equal in spinal cord tumors. Histomorphologically, necrosis and angiogenesis were associated with higher grades of tumor. Approximately 35%-children were alive after a mean follow-up of 36 ± 6 months.
Conclusion:
Compared with most international studies, we found a higher percentage of medulloblastoma in the brain, thus stressing the role of regional and ethnic influences in the pathogenesis of CNS tumors.
Introduction
In developing countries like India, childhood mortality is still largely due to malnutrition and infections; however, pediatric tumors are rising in the country and constitute an important cause of mortality in children.[1] Brain tumors are the most common type of pediatric solid tumors and are the most common tumors after leukemia. They represent about 20% of all childhood cancers in patients under 15 years of age.[2] Pediatric central nervous system (CNS) (brain and spinal cord) tumors are different from their adult counterparts in many ways. These tumors are often misdiagnosed or diagnosed late because of their rarity. Moreover, treatment options available may damage the developing brain resulting in moderate to severe neurocognitive, psychological, and endocrine dysfunction. Extensive tumor resection and role of chemotherapy above radiation are suggested for pediatric tumors.[3] However, these tumors carry a better prognosis as compared to adults with a similar condition.[4] Prognosis and 5-year survival depend on the type of tumor, location, Grades (I–IV), duration of symptoms, speed of growth, and infiltration into normal brain tissue.[5,6]
Unlike adults, almost half of all the pediatric brain tumors are in the infratentorial region. In the infratentorial region, the common tumors are medulloblastoma, low-grade cerebellar astrocytoma, brain stem glioma, and ependymoma. In the supratentorial region, most of the pediatric tumors are in the supra- or parasellar region (craniopharyngioma, optico-chiasmal or hypothalamic gliomas), hemispheric gliomas/primitive neuroectodermal tumors (PNETs), or pineal region tumors.[7,8]
Population-based studies are required to determine the cancer burden due to pediatric CNS malignancies and for the morphological categorization of brain tumors in India. There are very few studies published from India describing the prevalence of pediatric brain and spinal cord tumors and none from the hilly state of Uttarakhand in North India. This data will greatly contribute to the Asian database of pediatric CNS tumors.
Aims
- To study the prevalence of brain and spinal cord tumors in children <18>
- To study the clinical presentation, location, histopathological diagnosis, and grade of pediatric brain and spinal cord tumors operated at our hospital.
Materials and Methods
This study was a retrospective medical record-based observational study carried out in the department of pathology during July 2006 and June 2015 (10 years) at a tertiary referral center of North India. The data on patients were anonymized before inclusion to the study analysis.
Inclusion criteria
All patients of brain and spinal cord tumors under 18 years of age who were operated and treated in our hospital in the study duration were included in the study.
Exclusion criteria
- Patients who had received chemotherapy or radiotherapy before surgery
- Patients who had coexistent primary neoplasm elsewhere
- All cysts, hematomas, meningomyelocele, and other developmental malformations in CNS were excluded from the study.
The hospital records of all the patients fulfilling the inclusion criteria were analyzed, and descriptive epidemiological records were created for the patients by age, sex, and histological variables. The histological tumor types were grouped according to standard age at diagnosis (0–4, 4–9, 10–14, and 15–18 years age group). The histopathological variables tabulated were type and grade of tumor which were done according to the WHO grading of tumors.[5] Other histological variables such as invasion into the brain, necrosis, endothelial proliferation, and lymphomononuclear infiltrate were also taken into account. Immunohistochemistry glial fibrillary acidic protein, ki-67 (BioGenex antibodies) if already carried out on paraffin blocks were recorded and tabulated.
Results
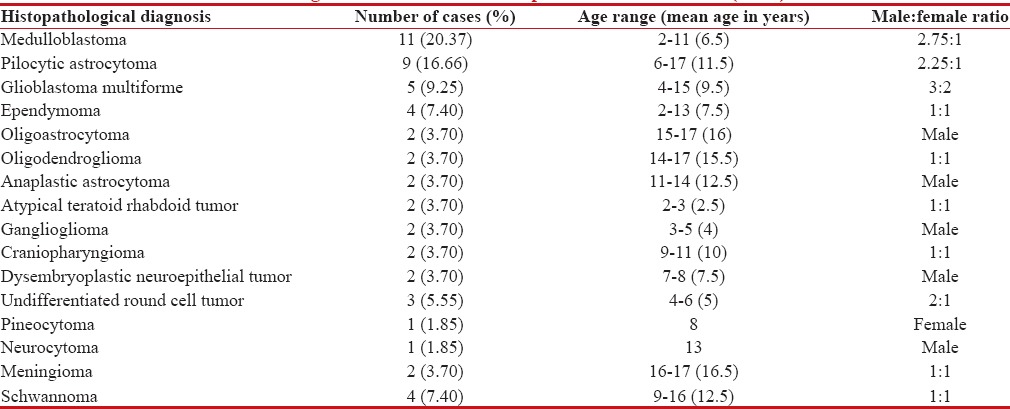
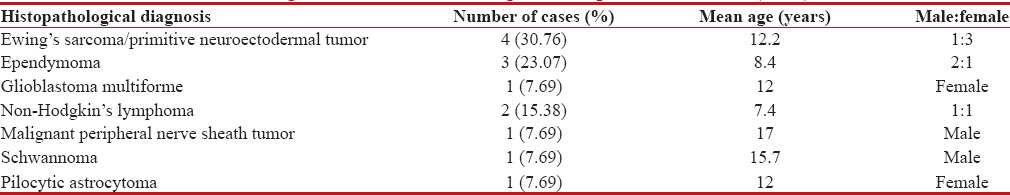
Over a period of 10 years, a total of 1194 nonhematopoietic pediatric malignancies were reported out of which 67 (5.6%) were CNS tumors. These included 54 brain tumors and 13 spinal cord tumors. The mean age for brain tumors was 10.5 years with a male:female ratio of 1.5:1 while the mean age for spinal cord tumors was 12.1 years with a male:female ratio of 1.1:1. Medulloblastoma (n = 11, 20.3%) was the most common tumor in the brain followed by pilocytic astrocytoma (n = 9, 16.6%) and glioblastoma multiforme (GBM) (n = 5, 9.25%) [Table 1 and Figure 1]. Ewing's sarcoma/PNET (n = 4, 30.7%) was the most common tumor in the spinal cord closely followed by ependymoma (n = 3, 23.07%) [Table 2 and Figure 2]. Ki-67 index >5% was seen in almost all the high-grade astrocytomas. Overall the highest incidence (46.2%) was found in the 5–9 years age group [Figure 3].
Table 1
Age and sex distribution of pediatric brain tumors (n=54)
|
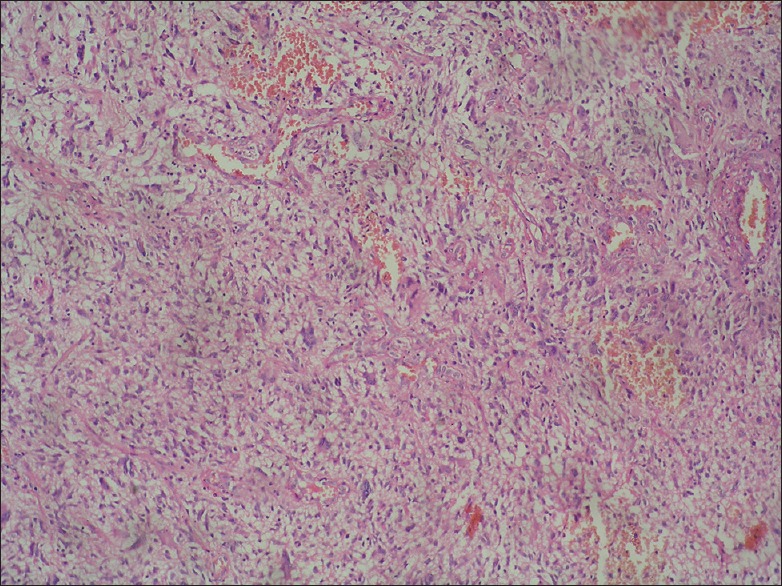
| Figure 1:Glioblastoma multiforme in the temporoparietal lobe of the brain, H and E: ×200
|
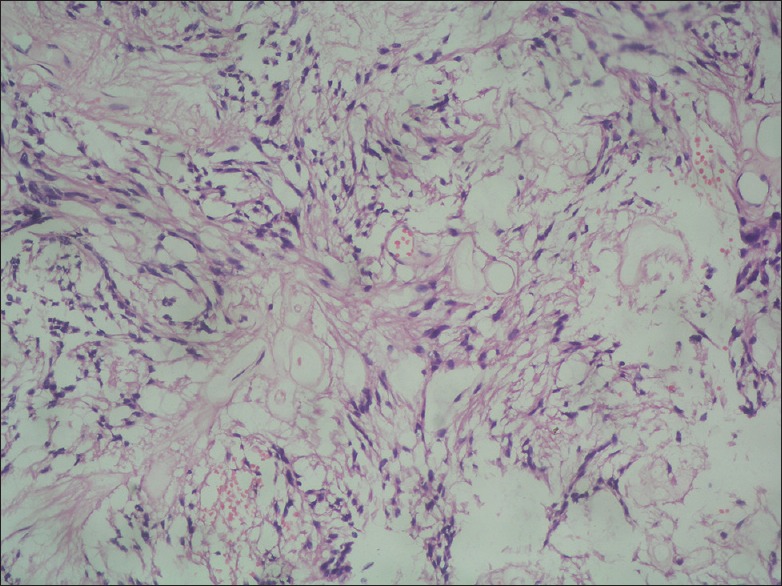
| Figure 2:Ependymoma in the spinal cord, H and E: ×200
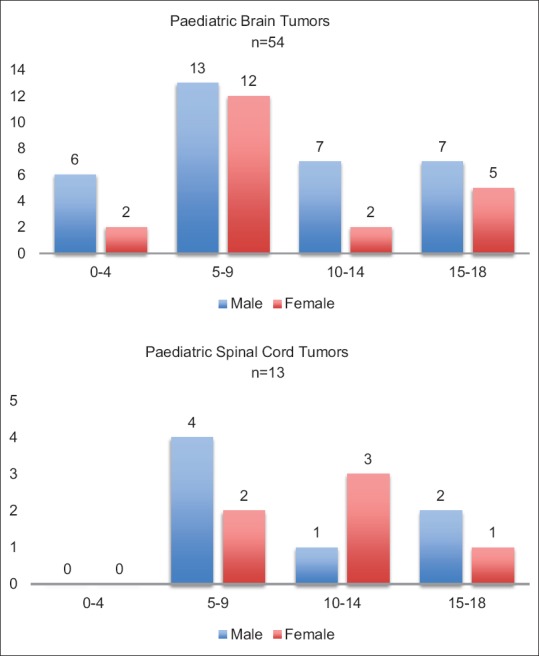
| Figure 3:Incidence of pediatric brain and spinal cord tumors
The children presented with headache, vomiting, seizures, and ataxia with duration ranging from 10 days to 1 year. One patient of GBM had coexistent neurofibromatosis while one patient of GBM had a history of being treated for low-grade glioma. Right temporoparietal region was the most frequently affected site after cerebellum for brain tumors on magnetic resonance imaging which revealed a contrast-enhancing lesion [Figure 4]. The dorsolumbar spine (D12-L2) was the most common site of involvement in the spinal cord. All the patients were treated by complete or near total surgical removal with irradiation of tumor bed. Among a total of 67 pediatric CNS tumors, only 42 children were available for long-term evaluation. Out of these 42, 27 died (19 treatment-related and 8 from relapse). Overall 15 (35.71%) were alive after a mean follow-up of 36 ± 6 months.
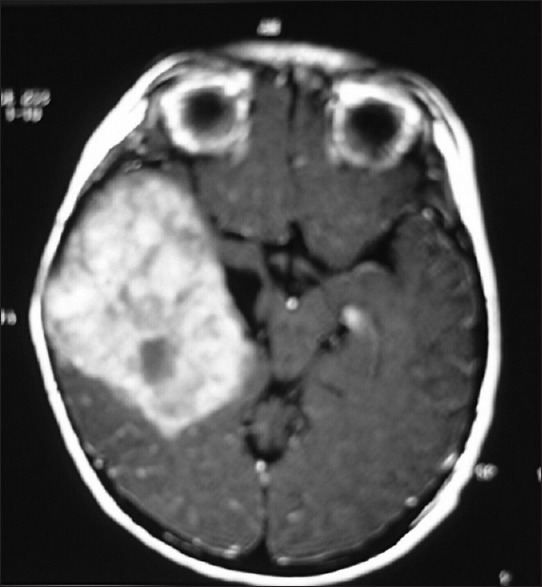
| Figure 4:Computed tomography scan showing high-grade astrocytoma: Contrast-enhancing lesion in the temporoparietal lobe
Discussion
Children constitute a large part of population in a developing country where life expectancy is lower than in the developed world.[9,10] One of the earliest studies on brain tumors is by Cushing in 1927.[11] In our study, pediatric CNS tumors constituted 5.6% of all pediatric solid tumors which is much lower as compared to a study by Rathi et al. in 2007 where the incidence was 18.2%;[1] however, it is comparable to a study conducted by Bhalodia and Patel in Southern Gujarat in 2011 where the incidence was 6.9%.[9] The male:female ratio in our study is 1.5:1 which is almost comparable to the study by Yeole et al.[12] and Nasir et al.[13] Male preponderance in India may also be the result of cultural factors wherein boys get more attention and are brought to the hospital more often for management.[12] Few ongoing investigations are underway which suggest that sexual dimorphism in tumor biology could account for this gender disparity, thereby warranting further studies elaborating the role of sex hormones on brain tumorigenesis.[14]
The mean age of pediatric brain tumors in our study is higher than that observed in the study by Nasir et al. (6.7 years)[13] and Mehrazin and Yavari (8.7 years).[15] Even though certain tumors occur more frequently at certain specific ages, it is of no particular importance in diagnosing tumor type preoperatively. All the tumors can occur at any age throughout childhood. Our series had more children in the second hemidecade of life (5–10 years) similar to earlier studies by Cushing,[11] Koos and Miller,[16] and Ahmed et al.[17] The peak age of brain tumors was 6 years in our study while Matson reported a high peak at age 4 years and a second peak at age 7 years followed by a steady decline.[18]
Symptoms and signs depend on the growth rate of the tumor, its location in the CNS, and age of the child.[19] Neurological symptoms produced by brain tumors are general or local. General symptoms result from increased intracranial pressure, which results directly from progressive enlargement of the tumor within the limited volume of the cranial vault; local symptoms are due to the effects of the tumor on contiguous areas of the brain. The most common presenting complaint for brain tumors in our study was headache (79.6%), seizures (56.2%), and vomiting (37.8%) while ataxia (45.5%) was the most common clinical feature in spinal cord tumors.
Medulloblastomas typically arise from the 4th ventricle and often invade the cerebellar vermis. It comprises poorly differentiated epithelial cells. The Chang staging system is often used for treatment and prognostic purposes.[15] This system classifies tumors by size and local infiltration (T1–T4) as well as degree of cerebrospinal fluid dissemination (M0–M4). M-stage is found to be predictive of outcome while T-stage has no significant role. Age is related to survival with younger age being associated with poor prognosis.[20] Medulloblastoma was the most common neoplasm in our series similar to study by Smoll and Drummond[21] and Nasir et al.[13] and in contrast to Western studies by Koos and Miller[16] and Matson[18] and Keith et al.,[22] where they found astrocytomas to be the predominant pediatric brain tumor. Dominance of astrocytoma has also been reported from other Middle Eastern countries including Iran and Kuwait.[15,23,24] The incidence of pilocytic astrocytoma was 16.6%-which is much lower than a study by Katchy et al. where these tumors constituted 29% of all pediatric brain tumors.[24] Resection is usually incomplete in diffuse astrocytomas due to permeative margins. Limited field external beam irradiation or stereotactic irradiation is the treatment of choice. We found a lesser incidence of craniopharyngiomas (3.7%) in contrast to a study by Aghayan Golkashani et al. where craniopharyngiomas (14%) were the most common tumors after medulloblastomas and astrocytomas.[25] Most common spinal cord tumor in our study was Ewing's sarcoma/PNET (n = 4, 30.7%) in contrast to a study by Wilson et al. where they found a high incidence of teratomas (31%) followed by astrocytomas.[26] Zhou et al. in China found that the most common pediatric spinal cord tumors in their center were ependymomas followed by astrocytic tumors.[27]
We can say that the comparison of cancer frequency and incidence is dependent to a large extent on variability in diagnosis and classification, differential access to medical care, and incomplete registration.
Conclusion
Pediatric brain and spinal cord tumors vary considerably in their histological, topographical, and gender distribution throughout childhood and adolescence. The results of this study highlight the high incidence of pediatric CNS tumors in North India. Compared with published Western data, we found a higher incidence of medulloblastomas. Analyzing differences in molecular and genetic pathways could aid in the development of targeted, individualized therapies and for planning treatment protocols and strategies. This may also result in adjustment of health programs according to statistics.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Rathi AK, Kumar S, Ashu A, Singh K, Bahadur AK. Epidemiology of pediatric tumors at a tertiary care centre. Indian J Med Paediatr Oncol 2007;28:33-5.
- Echevarría ME, Fangusaro J, Goldman S. Pediatric central nervous system germ cell tumors: A review. Oncologist 2008;13:690-9.
- Albright AL. Brain tumors in neonates, infants and toddlers. Contemp Neurosurg 1985;7:1-8.
- Hutter A, Schwetye KE, Bierhals AJ, McKinstry RC. Brain neoplasms: Epidemiology, diagnosis, and prospects for cost-effective imaging. Neuroimaging Clin N Am 2003;13:237-50.
- Kleihues P, Cavenee WK, editors. Pathology and Genetics of Tumors of the Nervous System. Lyon, France: International Agency for Research on Cancer; 2000.p314
- Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol 2007;114:97-109.
- Koeller KK, Sandberg GD; Armed Forces Institute of Pathology. From the archives of the AFIP. Cerebral intraventricular neoplasms: Radiologic-pathologic correlation. Radiographics 2002;22:1473-505.
- Schneider JH Jr., Raffel C, McComb JG. Benign cerebellar astrocytomas of childhood. Neurosurgery 1992;30:58-62.
- Bhalodia JN, Patel MM. Profile of pediatric malignancy: A three year study. Natl J Community Med 2011;2:24-7.
- Jabeen S, Haque M, Islam MJ, Talukdar MH. Profile of pediatric malignancies: A five year study. J Dhaka Med Coll 2010;19:33-8.
- ;Cushing H. The intracranial tumors of pre adolescence. Am J Dis Child 1927;33:551-84.
- Yeole BB, Advani SH, Sunny L. Epidemiological features of childhood cancers in greater Mumbai. Indian Pediatr 2001;38:1270-7.
- Nasir S, Jamila B, Khaleeq S. A retrospective study of primary brain tumors in children under 14 years of age at PIMS, Islamabad. Asian Pac J Cancer Prev 2010;11:1225-7.
- Sun T, Warrington NM, Rubin JB. Why does Jack, and not Jill, break his crown? Sex disparity in brain tumors. Biol Sex Differ 2012;3:3.
- Mehrazin M, Yavari P. Morphological pattern and frequency of intracranial tumors in children. Childs Nerv Syst 2007;23:157-62.
- Koos WT, Miller MH. Intracranial Tumors of Infants and Children. St. Louis: CV Moosby; 1971.
- Ahmed N, Bhurgri Y, Sadiq S, Shakoor KA. Pediatric brain tumours at a tertiary care hospital in Karachi. Asian Pac J Cancer Prev 2007;8:399-404.
- Matson DD. Neurosurgery of Infancy and Childhood. Springfield, IL, Charles C Thomas; 1969.
- Packer RJ, MacDonald T, Vezina G. Central nervous system tumors. Pediatr Clin North Am 2008;55:121-45.
- French LA. Tumors-intracranial and cranial. In: Jackson IJ, Thompson RK, editors. Pediatric Neurosurgery. Springfield, IL: Charles C Thomas; 1959. p. 224.
- Smoll NR, Drummond KJ. The incidence of medulloblastomas and primitive neurectodermal tumours in adults and children. J Clin Neurosci 2012;19:1541-4.
- Keith HM, Craig WM, Kernohan JW. Brain tumors in children. Pediatrics 1949;3:839-44.
- Kadri H, Mawla AA, Murad L. Incidence of childhood brain tumors in Syria (1993-2002). Pediatr Neurosurg 2005;41:173-7.
- Katchy KC, Alexander S, Al-Nashmi NM, Al-Ramadan A. Epidemiology of primary brain tumors in childhood and adolescence in Kuwait. Springerplus 2013;2:58.
- Aghayan Golkashani H, Hatami H, Farzan A, Mohammadi HR, Nilipour Y, Khoddami M, et al. Tumors of the central nervous system: An 18-year retrospective review in a tertiary pediatric referral center. Iran J Child Neurol 2015;9:24-33.
- Wilson PE, Oleszek JL, Clayton GH. Pediatric spinal cord tumors and masses. J Spinal Cord Med 2007;30 Suppl 1:S15-20.
- Zhou D, Zhang Y, Liu H, Luo S, Luo L, Dai K. Epidemiology of nervous system tumors in children: A survey of 1,485 cases in Beijing Tiantan Hospital from 2001 to 2005. Pediatr Neurosurg 2008;44:97-103.
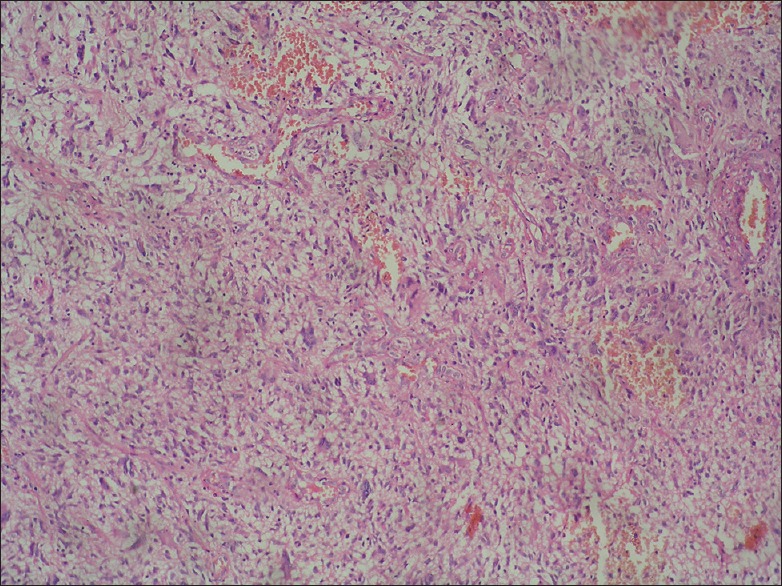
| Figure 1:Glioblastoma multiforme in the temporoparietal lobe of the brain, H and E: ×200
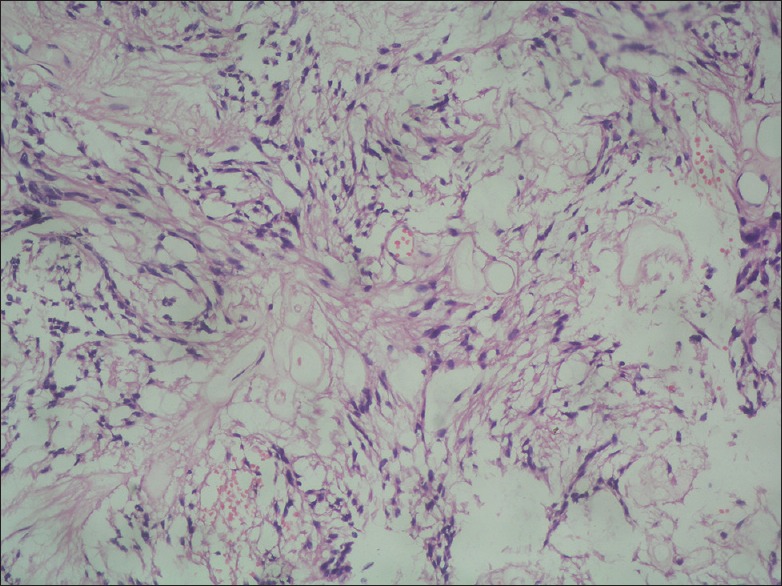
| Figure 2:Ependymoma in the spinal cord, H and E: ×200
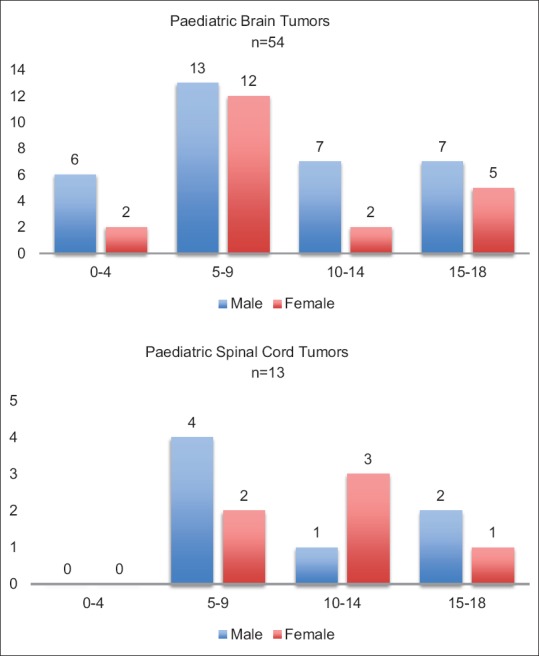
| Figure 3:Incidence of pediatric brain and spinal cord tumors
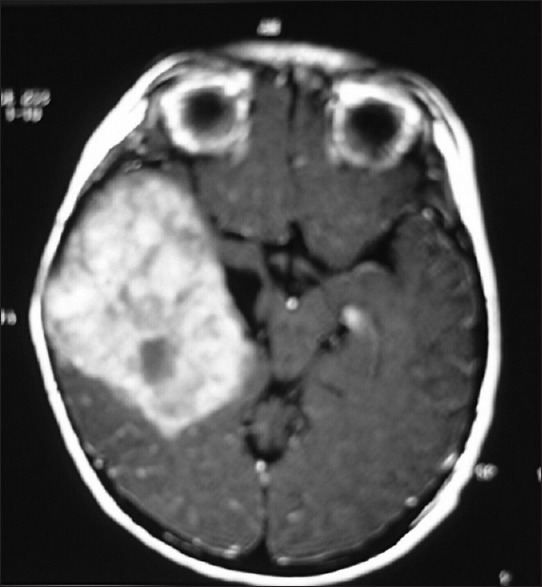
| Figure 4:Computed tomography scan showing high-grade astrocytoma: Contrast-enhancing lesion in the temporoparietal lobe
References
- Rathi AK, Kumar S, Ashu A, Singh K, Bahadur AK. Epidemiology of pediatric tumors at a tertiary care centre. Indian J Med Paediatr Oncol 2007;28:33-5.
- Echevarría ME, Fangusaro J, Goldman S. Pediatric central nervous system germ cell tumors: A review. Oncologist 2008;13:690-9.
- Albright AL. Brain tumors in neonates, infants and toddlers. Contemp Neurosurg 1985;7:1-8.
- Hutter A, Schwetye KE, Bierhals AJ, McKinstry RC. Brain neoplasms: Epidemiology, diagnosis, and prospects for cost-effective imaging. Neuroimaging Clin N Am 2003;13:237-50.
- Kleihues P, Cavenee WK, editors. Pathology and Genetics of Tumors of the Nervous System. Lyon, France: International Agency for Research on Cancer; 2000.p314
- Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol 2007;114:97-109.
- Koeller KK, Sandberg GD; Armed Forces Institute of Pathology. From the archives of the AFIP. Cerebral intraventricular neoplasms: Radiologic-pathologic correlation. Radiographics 2002;22:1473-505.
- Schneider JH Jr., Raffel C, McComb JG. Benign cerebellar astrocytomas of childhood. Neurosurgery 1992;30:58-62.
- Bhalodia JN, Patel MM. Profile of pediatric malignancy: A three year study. Natl J Community Med 2011;2:24-7.
- Jabeen S, Haque M, Islam MJ, Talukdar MH. Profile of pediatric malignancies: A five year study. J Dhaka Med Coll 2010;19:33-8.
- ;Cushing H. The intracranial tumors of pre adolescence. Am J Dis Child 1927;33:551-84.
- Yeole BB, Advani SH, Sunny L. Epidemiological features of childhood cancers in greater Mumbai. Indian Pediatr 2001;38:1270-7.
- Nasir S, Jamila B, Khaleeq S. A retrospective study of primary brain tumors in children under 14 years of age at PIMS, Islamabad. Asian Pac J Cancer Prev 2010;11:1225-7.
- Sun T, Warrington NM, Rubin JB. Why does Jack, and not Jill, break his crown? Sex disparity in brain tumors. Biol Sex Differ 2012;3:3.
- Mehrazin M, Yavari P. Morphological pattern and frequency of intracranial tumors in children. Childs Nerv Syst 2007;23:157-62.
- Koos WT, Miller MH. Intracranial Tumors of Infants and Children. St. Louis: CV Moosby; 1971.
- Ahmed N, Bhurgri Y, Sadiq S, Shakoor KA. Pediatric brain tumours at a tertiary care hospital in Karachi. Asian Pac J Cancer Prev 2007;8:399-404.
- Matson DD. Neurosurgery of Infancy and Childhood. Springfield, IL, Charles C Thomas; 1969.
- Packer RJ, MacDonald T, Vezina G. Central nervous system tumors. Pediatr Clin North Am 2008;55:121-45.
- French LA. Tumors-intracranial and cranial. In: Jackson IJ, Thompson RK, editors. Pediatric Neurosurgery. Springfield, IL: Charles C Thomas; 1959. p. 224.
- Smoll NR, Drummond KJ. The incidence of medulloblastomas and primitive neurectodermal tumours in adults and children. J Clin Neurosci 2012;19:1541-4.
- Keith HM, Craig WM, Kernohan JW. Brain tumors in children. Pediatrics 1949;3:839-44.
- Kadri H, Mawla AA, Murad L. Incidence of childhood brain tumors in Syria (1993-2002). Pediatr Neurosurg 2005;41:173-7.
- Katchy KC, Alexander S, Al-Nashmi NM, Al-Ramadan A. Epidemiology of primary brain tumors in childhood and adolescence in Kuwait. Springerplus 2013;2:58.
- Aghayan Golkashani H, Hatami H, Farzan A, Mohammadi HR, Nilipour Y, Khoddami M, et al. Tumors of the central nervous system: An 18-year retrospective review in a tertiary pediatric referral center. Iran J Child Neurol 2015;9:24-33.
- Wilson PE, Oleszek JL, Clayton GH. Pediatric spinal cord tumors and masses. J Spinal Cord Med 2007;30 Suppl 1:S15-20.
- Zhou D, Zhang Y, Liu H, Luo S, Luo L, Dai K. Epidemiology of nervous system tumors in children: A survey of 1,485 cases in Beijing Tiantan Hospital from 2001 to 2005. Pediatr Neurosurg 2008;44:97-103.


 PDF
PDF  Views
Views  Share
Share

