Pseudoepitheliomatous Hyperplasia: A Diagnostic Dilemma
CC BY-NC-ND 4.0 ? Indian J Med Paediatr Oncol 2018; 39(01): 114-116
DOI: DOI: 10.4103/ijmpo.ijmpo_198_16
Abstract
Pseudoepitheliomatous hyperplasia (PEH) is a benign reactive inflammatory reaction of the epithelial cells to various conditions. It is a diagnostic dilemma which simulates malignancy, especially squamous cell carcinoma (SCC). Many articles of PEH involving the oral mucosa are available on the internet, but ocular involvement is infrequent. The ocular lesion in our case resembled SCC but turned out to be PEH. We report a rare case of PEH in a 20-year-old male.
Publication History
Article published online:
23 June 2021
? 2018. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Pseudoepitheliomatous hyperplasia (PEH) is a benign reactive inflammatory reaction of the epithelial cells to various conditions. It is a diagnostic dilemma which simulates malignancy, especially squamous cell carcinoma (SCC). Many articles of PEH involving the oral mucosa are available on the internet, but ocular involvement is infrequent. The ocular lesion in our case resembled SCC but turned out to be PEH. We report a rare case of PEH in a 20-year-old male.
Introduction
PEH is a reactive epithelial proliferation an its diagnosis can be a great challange as this condition mimics many other malignant lesions. Hence, until a biopsy is performed, even the most experienced medical practitioner may get mislead in diagnosing this condition. Herein, we report an interesting case of PEH.
Case Report
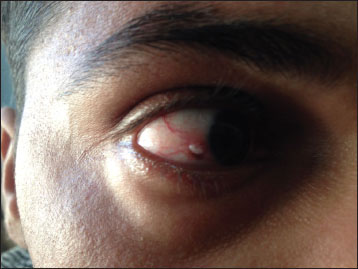
A 20-year-old male [Figure 1] and [Figure 2] presented to the department of ophthalmology with a history of mass/growth in the
right eye for the past 3 months which was progressively increasing in size. There was no other ocular complaint.
There was a history of recurrent gingivitis for which he had previous dental consultations. There was neither other
significant medical, surgical, personal, family, or drug abuse history nor the previous history of ocular
disease/trauma. The patient was nonsmoker, nonalcoholic, and vegetarian. His general physical and systemic
examination including oral mucosa was within normal limits. His visual acuity was 6/6 in both the eyes; pupillary
reactions, ocular movements, color vision, intraocular pressure, fundus examination, and B-scan ultrasonography were
normal. Torch light and slit lamp examination revealed a nodular mass, 2> < 2>
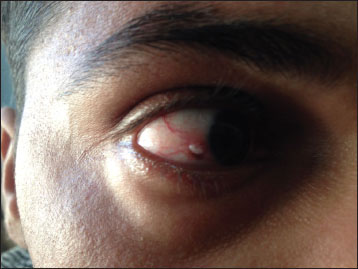
|?Figure.1Patients photo 1

|?Figure.2Patients photo 2
Routine blood investigations were normal. We planned a surgical excision biopsy of the lesion and the patient was fully informed of the procedure. Excision biopsy was conducted following ?Shield?s no touch technique?, and the specimen was sent for histopathological examination. Postoperatively [Figure 3], the patient was put on the topical antibiotic-steroids combination. The patient reported back to us after 1 week with the histopathology report [Figure 4] of his lesion which showed ?stratified squamous mucosa which showed focal keratosis, hyperplasia, and irregular acanthosis. The cells lining the hyperplastic mucosa were orderly arranged. Few showed the presence of intranuclear inclusions which are amphophilic. Some showed more than one inclusions. The submucosa showed inflammatory granulation tissue in the form of lymphomononuclear cells and congested blood vessels.? Sections from all the surgical margins were free from the lesion. The findings were consistent with pseudoepitheliomatous hyperplasia (PEH). Radiological investigations of the chest and abdomen were normal. Facility for immunohistochemical markers such as p53, E-Cadherin, and matrix metalloproteinases-1 (MMP-1) was not available with us. The patient is on regular follow-up with us for the past 3 months, and his ocular and systemic examination is This is an open access article distributed under the terms of the within the normal limits to date.

|?Figure.3Patients postoperative day 1 photo
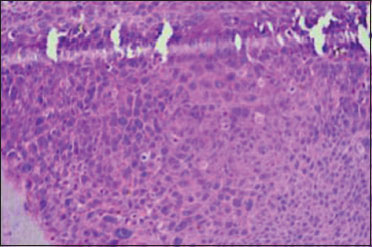
|?Figure.4Histopathological report
Disussion
PEH is a benign condition characterized by hyperplasia of the epidermis and adnexal epithelium. PEH may be primary (e.g., primal gingival PEH) or secondary (e.g., granular cell tumor or chronic irritation).[1] It can be a result of various conditions such as infections, inflammation, trauma, and malignancy and is also referred to as pseudocarcinomatous hyperplasia. Usually, PEH appears as a well-demarcated plaque or nodule with scaling and crusting. Papules or nodules may range from <1 href="https://www.thieme-connect.com/products/ejournals/html/10.4103/ijmpo.ijmpo_198_16#JR_2" xss=removed>2] Pathogenesis of PEH is probably the release of cytokines produced by the tumor and inflammatory cells lead to a proliferation of the overlying epithelium.[3]
Histological grading of PEH puts it into three types:[4]
-
Grade I: Hyperplasia, acanthosis, elongation of rete ridges to sweat glands, and intact basement membrane
-
Grade II: Noticeable proliferation of the rete ridges and extension deeper, irregular interpapillary projections, indefinite basement membrane, and cells epithelial down growth assumes embryonic character
-
Grade III: Mixture of irregular extensions of the epithelial down growth with the granulomatous formation and embryonic cell character. Appearance similar to well-differentiated SCC.
The differential diagnosis of PEH is SCC, keratoacanthoma, granular cell tumor, necrotizing sialometaplasia, malignant melanoma, and verrucous carcinoma.[4]
It is often difficult to distinguish PEH from SCC. The SCC shows increased staining for p53 and MMP-1 and less intense staining for E-cadherin [5] plus, the universal cytological criteria for SCC are nuclear enlargement, hyperchromasia, irregular nuclear outline, coarse nuclear chromatin, and prominent nucleoli.[6] The presence of a nodular lesion with feeder vessels and intrinsic vascularity should raise a suspicion of invasive SCC [7] as was seen in our case, and hence, the word ?diagnostic dilemma? is one of the most appropriate words for this lesion.
Complete excision and additional cryotherapy is the most appropriate management for this condition as difficulty prevails in clinically and histologically differentiating PEH from low-grade SCC,[8] while the use of photodynamic therapy and microdebrider shaver in its treatment of has also been reported.[9]
Conclusion
Whether PEH possesses a malignant potential or not is still a dilemma. Some studies consider it having a premalignant potential. Complete surgical excision of the lesion is a known treatment modality for malignancy while wait and watch is mostly advocated for benign lesions. The authors consider complete surgical excision of any suspicious ocular mass so that not only a good biopsy is achieved, but any future ocular threat to the eye is avoided.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflict of Interest
There are no conflicts of interest.
References
- Chakrabarti S, Chakrabarti PR, Agrawal D, Somanath S.?Pseudoepitheliomatous hyperplasia: A clinical entity mistaken for squamous cell carcinoma. J Cutan Aesthet Surg 2014; 7: 232-4
- Nayak VN, Uma K, Girish HC, Murgod S, Shyamala K, Naik RB.?et al.?Pseudoepitheliomatous hyperplasia in oral lesions: A Review. J Int Oral Health 2015; 7: 148-52
- Gattuso P, Candel AG, Castelli MJ, Kowal-Vern A, Gamelli RL, Herman C.?et al.?Pseudoepitheliomatous hyperplasia in chronic cutaneous wounds. A flow cytometric study. J Cutan Pathol 1994; 21: 312-5
- Sarangarajan R, Vedam VK, Sivadas G, Krishnaraj R, Sarangarajan A, Shanmugam KT.?Pseudoepitheliomatous hyperplasia: Relevance in oral pathology. J Int Oral Health 2015; 7: 132-6
- Zarovnaya E, Black C.?Distinguishing pseudoepitheliomatous hyperplasia from squamous cell carcinoma in mucosal biopsy specimens from the head and neck. Arch Pathol Lab Med 2005; 129: 1032-6
- Mittal R, Rath S, Vemuganti GK.?Ocular surface squamous neoplasia - Review of etio-pathogenesis and an update on clinico-pathological diagnosis. Saudi J Ophthalmol 2013; 27: 177-86
- Dandala PP, Malladi P. Kavitha.?Ocular Surface Squamous Neoplasia (OSSN): A Retrospective Study. J Clin Diagn Res 2015; 9: NC10-3
- Honavar SG, Manjandavida FP.?Tumors of the ocular surface: A review. Indian J Ophthalmol 2015; 63: 187-203
- Sarin V, Bhardwaj B, Gill JS, Singh B.?Pseudoepitheliomatous hyperplasia of tongue treated by microdebrider shaver. Pak J Otolaryngol 2013; 29: 47-8
Address for correspondence
Publication History
Article published online:
23 June 2021
? 2018. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2,
Noida-201301 UP, India
|?Figure.1Patients photo 1

|?Figure.2Patients photo 2

|?Figure.3Patients postoperative day 1 photo
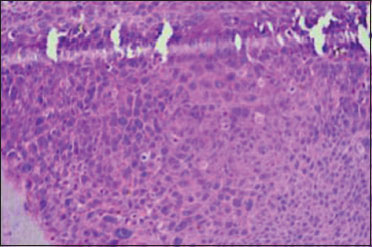
|?Figure.4Histopathological report
References
- Chakrabarti S, Chakrabarti PR, Agrawal D, Somanath S.?Pseudoepitheliomatous hyperplasia: A clinical entity mistaken for squamous cell carcinoma. J Cutan Aesthet Surg 2014; 7: 232-4
- Nayak VN, Uma K, Girish HC, Murgod S, Shyamala K, Naik RB.?et al.?Pseudoepitheliomatous hyperplasia in oral lesions: A Review. J Int Oral Health 2015; 7: 148-52
- Gattuso P, Candel AG, Castelli MJ, Kowal-Vern A, Gamelli RL, Herman C.?et al.?Pseudoepitheliomatous hyperplasia in chronic cutaneous wounds. A flow cytometric study. J Cutan Pathol 1994; 21: 312-5
- Sarangarajan R, Vedam VK, Sivadas G, Krishnaraj R, Sarangarajan A, Shanmugam KT.?Pseudoepitheliomatous hyperplasia: Relevance in oral pathology. J Int Oral Health 2015; 7: 132-6
- Zarovnaya E, Black C.?Distinguishing pseudoepitheliomatous hyperplasia from squamous cell carcinoma in mucosal biopsy specimens from the head and neck. Arch Pathol Lab Med 2005; 129: 1032-6
- Mittal R, Rath S, Vemuganti GK.?Ocular surface squamous neoplasia - Review of etio-pathogenesis and an update on clinico-pathological diagnosis. Saudi J Ophthalmol 2013; 27: 177-86
- Dandala PP, Malladi P. Kavitha.?Ocular Surface Squamous Neoplasia (OSSN): A Retrospective Study. J Clin Diagn Res 2015; 9: NC10-3
- Honavar SG, Manjandavida FP.?Tumors of the ocular surface: A review. Indian J Ophthalmol 2015; 63: 187-203
- Sarin V, Bhardwaj B, Gill JS, Singh B.?Pseudoepitheliomatous hyperplasia of tongue treated by microdebrider shaver. Pak J Otolaryngol 2013; 29: 47-8


 PDF
PDF  Views
Views  Share
Share

