Smokeless Tobacco and Its Ill-Effects: Recent Literature Update
CC BY-NC-ND 4.0 ? Indian J Med Paediatr Oncol 2021; 42(05): 486-490
DOI: DOI: 10.1055/s-0041-1735598
Abstract
According to the Global Adult Tobacco Survey part 2 (GATS-2), approximately 200 million adult Indians consume smokeless tobacco (SLT). Circumvention of SLT product ban has been observed. We conducted a review of the literature to summarize the ill effects of tobacco for the articles published from 2019 to 2020. A systematic search of the databases PubMed (2019 onward) and Web of Science (2019 onward), through February 2021 was done. Search yielded 1,061 articles and after excluding articles based on the inclusion criteria, 37 articles were taken in to consideration. The review shows that differential SLT product has specific odds of oral carcinogenesis. Review also indicates the emerging data of cardiovascular risk due to higher use of SLT products along with its known cause of oral cancer. It also cautions about the adverse consequences of pregnancy associated with SLT use.
Publication History
Publication Date:
05 December 2021 (online)
? 2021. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
According to the Global Adult Tobacco Survey part 2 (GATS-2), approximately 200 million adult Indians consume smokeless tobacco (SLT). Circumvention of SLT product ban has been observed. We conducted a review of the literature to summarize the ill effects of tobacco for the articles published from 2019 to 2020. A systematic search of the databases PubMed (2019 onward) and Web of Science (2019 onward), through February 2021 was done. Search yielded 1,061 articles and after excluding articles based on the inclusion criteria, 37 articles were taken in to consideration. The review shows that differential SLT product has specific odds of oral carcinogenesis. Review also indicates the emerging data of cardiovascular risk due to higher use of SLT products along with its known cause of oral cancer. It also cautions about the adverse consequences of pregnancy associated with SLT use.
Smokeless Tobacco and Its Ill Effects: Recent Literature Update
Oral cavity cancers are among the most common cancers affecting males in India.[1] Tobacco, alcohol, and areca nut are the root causes for high incidence of oral cancer in India.[2] However, tobacco has widespread effects on oral health, apart from oral cavity cancers, it is also responsible for 7 million deaths worldwide.[3] Smokeless tobacco not only causes cancer of the oral cavity, it is also responsible for higher incidence of esophageal and pancreatic cancers.[4] It has been documented to increase the risk of stroke and cardiovascular diseases. Consumption of smokeless tobacco (SLT) during pregnancy can also lead to higher chances of reduced gestation age and birth weight.[5]
According to the Global Adult Tobacco Survey part 2 (GATS-2) India survey,[6] incidence of SLT use is significantly more than combustible tobacco product. It has also shown that in India, states like Madhya Pradesh, Odisha, Bihar, Jharkhand, Chhattisgarh, and Northwestern states have high incidence of SLT use (above 30%) while Maharashtra, Gujrat, and Uttar Pradesh fall in moderate category (20?30%) and North and South Indian states have incidence of SLT use ranging from 10 to 20%. More than 30 types of SLT are consumed in India. To curb its usage and production, government has enacted many tobacco control legislations. As of May 2013, few SLT product involving pan masala and gutkha are banned in 24 states and 3 union territories in India.[7] However, the Federal Food Safety and Regulation act 2011 allows harmful product to be banned for a year after which it needs to be renewed every year based on the current evidence. Thus, primary aim of the study was to update the literature with the latest available evidence on the ill effect of SLT in India, as well as globally.
Methods
A systematic search of the databases PubMed (2019 onward) and Web of Science (2019 onward) through February 2021 was done. Relevant articles were identified. The search terms used were ?smokeless tobacco,? ?cancer,? ?oral cancer,? ?ill effects,? ?cardiovascular disease,? ?stroke,? ?pregnancy,? ?potentially malignant lesion,? ?precancer,? ?gutkha,? and ?gutka.? These were searched as text, as well as in combination using Boolean ?AND.? The cross-reference lists of relevant articles were also screened for suitable studies. This search yielded 1,061 articles. Inclusion criteria involved those articles which were published between the year 2019 and 2021, those published in English literature, studies including exposed individuals consuming SLT leading to oral cancer or cancer or any ill-health effects were included in the review. Articles were excluded from the review if they failed to describe the factors of interest of the study. Search strategy is described in [Fig. 1]. Among these articles, 37 articles were included in the narrative review which described SLT and its ill effects on health. [Table 1] presents the recent studies showing relationship between SLT use and oral cancer/cardiovascular diseases.
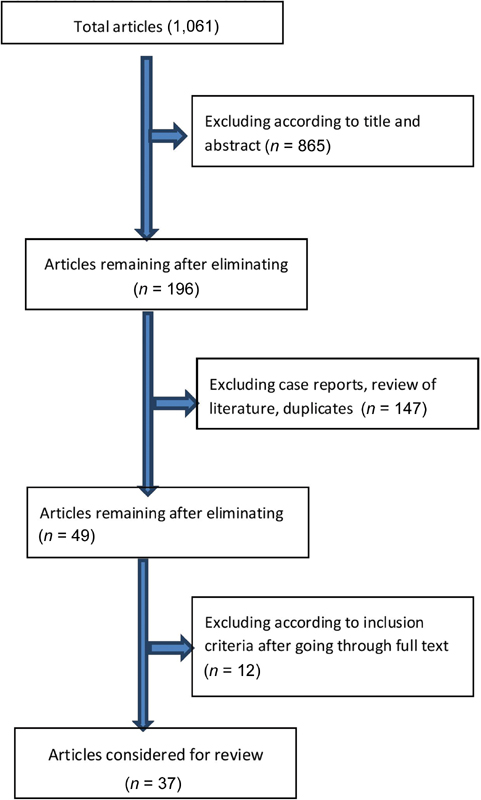
|?Fig. 1? A flowchart depicting the study selection.|
|
Sl. no. |
Author |
Study type |
Site |
Outcome |
Type of SLT |
OR |
HR |
CI (95%) |
|---|---|---|---|---|---|---|---|---|
|
1 |
Khan et al[16] |
Case-control |
India |
OSMF |
SLT |
18 |
? |
NA |
|
2 |
Khan et al[16] |
Case-control |
India |
OSMF |
Gutkha?+?bidi |
12.3 |
? |
NA |
|
3 |
Patil et al[10] |
Systematic review |
Africa |
Oral cancer/OPMD |
Shammah |
? |
38.74 |
19.50?76.96 |
|
4 |
Asthana et al[8] |
Systematic review |
SEAR |
Oral cancer |
SLT |
4.44 |
? |
3.51?5.61 |
|
5 |
Asthana et al[8] |
Systematic review |
EMR |
Oral cancer |
SLT |
1.28 |
? |
1.04?1.56 |
|
6 |
Asthana et al[8] |
Systematic review |
WHO (six) |
Oral cancer |
Gutkha |
8.67 |
? |
3.59?20.93 |
|
7 |
Asthana et al[8] |
Systematic review |
WHO (six) |
Oral cancer |
Pan masala |
7.18 |
? |
5.48?9.41 |
|
8 |
Asthana et al[8] |
Systematic review |
WHO (six) |
Oral cancer |
Oral snuff |
4.18 |
? |
2.37?7.38 |
|
9 |
Asthana et al[8] |
Systematic review |
WHO (six) |
Oral cancer |
Manipuri tobacco |
3.32 |
? |
2.32?8.36 |
|
10 |
Byhamre et al[31] |
Cohort |
Sweden |
Cancer |
Snus |
? |
1.12 |
1.00?1.26 |
|
11 |
Khan et al[12] |
Case control |
Pakistan |
Oral cancer |
Snuff |
4.82 |
? |
2.37?9.80 |
|
12 |
Khan et al[12] |
Case control |
Pakistan |
Oral cancer |
Betel leaf |
4.42 |
? |
1.66?11.91 |
|
13 |
Byhamre et al[31] |
Cohort |
Sweden |
Cardiovascular |
Snus |
? |
1.27 |
1.15?1.41 |
|
14 |
Gupta et al[11] |
Systematic review |
WHO |
CHD (fatal) |
Snus |
1.1 |
? |
1.00?1.20 |
- Sung H, Ferlay J, Siegel RL. et al.?Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021; 71 (03) 209-249
- Singhavi HR, Singh A, Bhattacharjee A, Talole S, Dikshit R, Chaturvedi P.?Alcohol and cancer risk: a systematic review and meta-analysis of prospective Indian studies. Indian J Public Health 2020; 64 (02) 186-190
- GBD 2017 Risk Factor Collaborators.?Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990?2017: a systematic analysis for the Global Burden of Disease Study. Lancet 2017; 390 (10100): 1345-1422
- Gupta S, Gupta R, Sinha DN, Mehrotra R.?Relationship between type of smokeless tobacco & risk of cancer: a systematic review. Indian J Med Res 2018; 148 (01) 56-76
- Gupta PC, Subramoney S.?Smokeless tobacco use, birth weight, and gestational age: population based, prospective cohort study of 1217 women in Mumbai, India. BMJ 2004; 328 (7455): 1538
- Gupta PC, Ray CS, Narake SS. et al.?Profile of dual tobacco users in India: an analysis from Global Adult Tobacco Survey, 2009-10. Indian J Cancer 2012; 49 (04) 393-400
- Kumar S.?Indian state bans tobacco based chewing products. BMJ 2002; 325 (7357): 184
- Asthana S, Labani S, Kailash U, Sinha DN, Mehrotra R.?Association of smokeless tobacco use and oral cancer: a systematic global review and meta-analysis. Nicotine Tob Res 2019; 21 (09) 1162-1171
- Asthana S, Vohra P, Labani S.?Association of smokeless tobacco with oral cancer: a review of systematic reviews. Tob Prev Cessat 2019; 5: 34
- Patil S, Alamir AWH, Arakeri G. et al.?The relationship of shammah (Arabian snuff) chewing to the risk of oral cancer and oral potentially malignant disorders. J Oral Pathol Med 2019; 48 (06) 425-432
- Gupta R, Gupta S, Sharma S, Sinha DN, Mehrotra R.?Risk of coronary heart disease among smokeless tobacco users: results of systematic review and meta-analysis of global data. Nicotine Tob Res 2019; 21 (01) 25-31
- Khan SZ, Farooq A, Masood M. et al.?Smokeless tobacco use and risk of oral cavity cancer. Turk J Med Sci 2020; 50 (01) 291-297
- Bastakoti S, Shrestha G, Kumar Gautam D. et al.?Clinico-pathological spectrum of oral cavity lesions at a tertiary care center in central nepal: a descriptive cross-sectional study. JNMA J Nepal Med Assoc 2021; 59 (234) DOI:?10.31729/jnma.5539.
- Sinha DN, Bajracharya B, Khadka BB, Rinchen S, Bhattad VB, Singh PK.?Smokeless tobacco use in Nepal. Indian J Cancer 2012; 49 (04) 352-356
- Pandey A, Singh A, Singh S. et al.?Oral smokeless tobacco consumption pattern among rural Indian cancer patients: a prospective survey. South Asian J Cancer 2020; 9 (01) 17-19
- Khan A, Ongole R, Baptist J, Srikant N, Lukmani F.?Patterns of tobacco use and its relation to oral precancers and cancers among individuals visiting a tertiary hospital in South India. J Contemp Dent Pract 2020; 21 (03) 304-309
- Rao NR, Villa A, More CB, Jayasinghe RD, Kerr AR, Johnson NW.?Oral submucous fibrosis: a contemporary narrative review with a proposed inter-professional approach for an early diagnosis and clinical management. J Otolaryngol Head Neck Surg 2020; 49 (01) 3
- Mishra GA, Pimple SA, Gupta SD.?Smokeless tobacco use and oral neoplasia among urban Indian women. Oral Dis 2019; 25 (07) 1724-1734
- Bhattacharjee T, Mandal P, Gangopadhyay S.?Smokeless tobacco use and related oral mucosal changes in Bengali Women. J Family Med Prim Care 2020; 9 (06) 2741-2746
- Rupani MP, Parikh KD, Kakadia MJ, Pathak MM, Patel MR, Shah MA.?Cross-sectional study on smokeless tobacco use, awareness and expenditure in an urban slum of Bhavnagar, western India. Natl Med J India 2019; 32 (03) 137-140
- Tirukkovalluri SS, Luck CP, Makesh RLS. et al.?Workplace based potentially malignant oral lesions screening among tobacco consuming migrant construction site workers in Chennai, South India: a pilot study. J Family Med Prim Care 2020; 9 (09) 5004-5009
- Datta KK, Patil S, Patel K. et al.?Chronic exposure to chewing tobacco induces metabolic reprogramming and cancer stem cell-like properties in esophageal epithelial cells. Cells 2019; 8 (09) 949
- Pansare K, Gardi N, Kamat S. et al.?Establishment and genomic characterization of gingivobuccal carcinoma cell lines with smokeless tobacco associated genetic alterations and oncogenic PIK3CA mutation. Sci Rep 2019; 9 (01) 8272
- Doherty Lyons S, Blum JL, Hoffman-Budde C. et al.?Prenatal exposure to gutkha, a globally relevant smokeless tobacco product, induces hepatic changes in adult mice. Int J Environ Res Public Health 2020; 17 (21) 7895
- Ta? B, G?re AO.?The effect of Maras powder and smoking on the microRNA deregulation of oral mucosa. J Appl Oral Sci 2020; 28: e20190382
- Choudhary AK, Qudeer A.?Smokeless tobacco: risk factor for cardiovascular and breathing in young Indian adolescent. Hipertens Riesgo Vasc 2019; 36 (04) 176-183
- Diend?r? J, Zeba AN, Niki?ma L. et al.?Smokeless tobacco use: its prevalence and relationships with dental symptoms, nutritional status and blood pressure among rural women in Burkina Faso. BMC Public Health 2020; 20 (01) 579
- Zutshi DV, Gupta MD, Girish MP. et al.?Evaluation of systemic inflammatory and thrombotic markers of cardiovascular risk among young Indian oral tobacco users. Indian Heart J 2020; 72 (05) 389-393
- Shrestha S, Mishra DR, Dhakal N, Bhandari S, Khanal S, Lamsal M.?Correlation of urinary cotinine with cardiovascular risk factors in pan masala tobacco users. Indian Heart J 2019; 71 (06) 459-463
- Titova OE, Baron JA, Micha?lsson K, Larsson SC.?Swedish snuff (snus) and risk of cardiovascular disease and mortality: prospective cohort study of middle-aged and older individuals. BMC Med 2021; 19 (01) 111
- Byhamre ML, Araghi M, Alfredsson L. et al.?Swedish snus use is associated with mortality: a pooled analysis of eight prospective studies. Int J Epidemiol 2021; 49 (06) 2041-2050
- De Queiroz Andrade E, Da Silva Sena CR, Collison A. et al.?Association between active tobacco use during pregnancy and infant respiratory health: a systematic review and meta-analysis. BMJ Open 2020; 10 (09) e037819
-
Ratsch A, Bogossian F,
Steadman K.?Central Australian Aboriginal women's pregnancy, labour and birth
outcomes following maternal smokeless tobacco (pituri) use, cigarette use
or no-tobacco use: a prospective cohort study. BMC Public Health 2021; 21 (01) 814
Address for correspondence
Publication History
Publication Date:
05 December 2021 (online)
? 2021. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
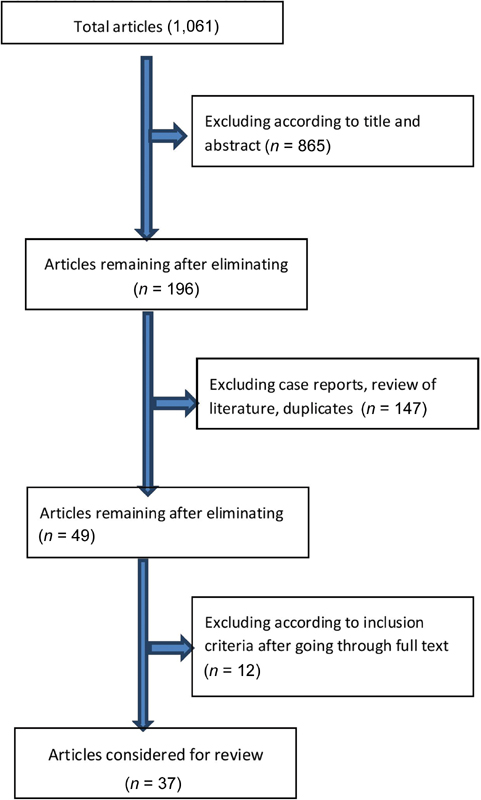
|?Fig. 1? A flowchart depicting the study selection.|
References
- Sung H, Ferlay J, Siegel RL. et al.?Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021; 71 (03) 209-249
- Singhavi HR, Singh A, Bhattacharjee A, Talole S, Dikshit R, Chaturvedi P.?Alcohol and cancer risk: a systematic review and meta-analysis of prospective Indian studies. Indian J Public Health 2020; 64 (02) 186-190
- GBD 2017 Risk Factor Collaborators.?Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990?2017: a systematic analysis for the Global Burden of Disease Study. Lancet 2017; 390 (10100): 1345-1422
- Gupta S, Gupta R, Sinha DN, Mehrotra R.?Relationship between type of smokeless tobacco & risk of cancer: a systematic review. Indian J Med Res 2018; 148 (01) 56-76
- Gupta PC, Subramoney S.?Smokeless tobacco use, birth weight, and gestational age: population based, prospective cohort study of 1217 women in Mumbai, India. BMJ 2004; 328 (7455): 1538
- Gupta PC, Ray CS, Narake SS. et al.?Profile of dual tobacco users in India: an analysis from Global Adult Tobacco Survey, 2009-10. Indian J Cancer 2012; 49 (04) 393-400
- Kumar S.?Indian state bans tobacco based chewing products. BMJ 2002; 325 (7357): 184
- Asthana S, Labani S, Kailash U, Sinha DN, Mehrotra R.?Association of smokeless tobacco use and oral cancer: a systematic global review and meta-analysis. Nicotine Tob Res 2019; 21 (09) 1162-1171
- Asthana S, Vohra P, Labani S.?Association of smokeless tobacco with oral cancer: a review of systematic reviews. Tob Prev Cessat 2019; 5: 34
- Patil S, Alamir AWH, Arakeri G. et al.?The relationship of shammah (Arabian snuff) chewing to the risk of oral cancer and oral potentially malignant disorders. J Oral Pathol Med 2019; 48 (06) 425-432
- Gupta R, Gupta S, Sharma S, Sinha DN, Mehrotra R.?Risk of coronary heart disease among smokeless tobacco users: results of systematic review and meta-analysis of global data. Nicotine Tob Res 2019; 21 (01) 25-31
- Khan SZ, Farooq A, Masood M. et al.?Smokeless tobacco use and risk of oral cavity cancer. Turk J Med Sci 2020; 50 (01) 291-297
- Bastakoti S, Shrestha G, Kumar Gautam D. et al.?Clinico-pathological spectrum of oral cavity lesions at a tertiary care center in central nepal: a descriptive cross-sectional study. JNMA J Nepal Med Assoc 2021; 59 (234) DOI:?10.31729/jnma.5539.
- Sinha DN, Bajracharya B, Khadka BB, Rinchen S, Bhattad VB, Singh PK.?Smokeless tobacco use in Nepal. Indian J Cancer 2012; 49 (04) 352-356
- Pandey A, Singh A, Singh S. et al.?Oral smokeless tobacco consumption pattern among rural Indian cancer patients: a prospective survey. South Asian J Cancer 2020; 9 (01) 17-19
- Khan A, Ongole R, Baptist J, Srikant N, Lukmani F.?Patterns of tobacco use and its relation to oral precancers and cancers among individuals visiting a tertiary hospital in South India. J Contemp Dent Pract 2020; 21 (03) 304-309
- Rao NR, Villa A, More CB, Jayasinghe RD, Kerr AR, Johnson NW.?Oral submucous fibrosis: a contemporary narrative review with a proposed inter-professional approach for an early diagnosis and clinical management. J Otolaryngol Head Neck Surg 2020; 49 (01) 3
- Mishra GA, Pimple SA, Gupta SD.?Smokeless tobacco use and oral neoplasia among urban Indian women. Oral Dis 2019; 25 (07) 1724-1734
- Bhattacharjee T, Mandal P, Gangopadhyay S.?Smokeless tobacco use and related oral mucosal changes in Bengali Women. J Family Med Prim Care 2020; 9 (06) 2741-2746
- Rupani MP, Parikh KD, Kakadia MJ, Pathak MM, Patel MR, Shah MA.?Cross-sectional study on smokeless tobacco use, awareness and expenditure in an urban slum of Bhavnagar, western India. Natl Med J India 2019; 32 (03) 137-140
- Tirukkovalluri SS, Luck CP, Makesh RLS. et al.?Workplace based potentially malignant oral lesions screening among tobacco consuming migrant construction site workers in Chennai, South India: a pilot study. J Family Med Prim Care 2020; 9 (09) 5004-5009
- Datta KK, Patil S, Patel K. et al.?Chronic exposure to chewing tobacco induces metabolic reprogramming and cancer stem cell-like properties in esophageal epithelial cells. Cells 2019; 8 (09) 949
- Pansare K, Gardi N, Kamat S. et al.?Establishment and genomic characterization of gingivobuccal carcinoma cell lines with smokeless tobacco associated genetic alterations and oncogenic PIK3CA mutation. Sci Rep 2019; 9 (01) 8272
- Doherty Lyons S, Blum JL, Hoffman-Budde C. et al.?Prenatal exposure to gutkha, a globally relevant smokeless tobacco product, induces hepatic changes in adult mice. Int J Environ Res Public Health 2020; 17 (21) 7895
- Ta? B, G?re AO.?The effect of Maras powder and smoking on the microRNA deregulation of oral mucosa. J Appl Oral Sci 2020; 28: e20190382
- Choudhary AK, Qudeer A.?Smokeless tobacco: risk factor for cardiovascular and breathing in young Indian adolescent. Hipertens Riesgo Vasc 2019; 36 (04) 176-183
- Diend?r? J, Zeba AN, Niki?ma L. et al.?Smokeless tobacco use: its prevalence and relationships with dental symptoms, nutritional status and blood pressure among rural women in Burkina Faso. BMC Public Health 2020; 20 (01) 579
- Zutshi DV, Gupta MD, Girish MP. et al.?Evaluation of systemic inflammatory and thrombotic markers of cardiovascular risk among young Indian oral tobacco users. Indian Heart J 2020; 72 (05) 389-393
- Shrestha S, Mishra DR, Dhakal N, Bhandari S, Khanal S, Lamsal M.?Correlation of urinary cotinine with cardiovascular risk factors in pan masala tobacco users. Indian Heart J 2019; 71 (06) 459-463
- Titova OE, Baron JA, Micha?lsson K, Larsson SC.?Swedish snuff (snus) and risk of cardiovascular disease and mortality: prospective cohort study of middle-aged and older individuals. BMC Med 2021; 19 (01) 111
- Byhamre ML, Araghi M, Alfredsson L. et al.?Swedish snus use is associated with mortality: a pooled analysis of eight prospective studies. Int J Epidemiol 2021; 49 (06) 2041-2050
- De Queiroz Andrade E, Da Silva Sena CR, Collison A. et al.?Association between active tobacco use during pregnancy and infant respiratory health: a systematic review and meta-analysis. BMJ Open 2020; 10 (09) e037819
- Ratsch A, Bogossian F, Steadman K.?Central Australian Aboriginal women's pregnancy, labour and birth outcomes following maternal smokeless tobacco (pituri) use, cigarette use or no-tobacco use: a prospective cohort study. BMC Public Health 2021; 21 (01) 814


 PDF
PDF  Views
Views  Share
Share

