Sociodemographic and Clinical Profile of Cervical Cancer Patients Visiting in a Tertiary Care Hospital in India
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2017; 38(03): 291-295
DOI: DOI: 10.4103/ijmpo.ijmpo_20_16
Abstract
Context: Cancer of the cervix is the most common genital tract malignancy in the female and is a major public health problem in the developing countries. Study of the sociodemographic and clinical profile of patients is the first step in planning control measures and treatment facilities. Aims: The aims of the study were to determine the sociodemographic and clinical profile of cervical cancer patients and study their association with other tumor-related factors. Settings and Design: This is a record-based retrospective study from a single institution. Subjects and Methods: The data on sociodemographic and clinical factors of 765 cervical cancer patients visited and treated at tertiary care cancer hospital in Mumbai in 1 year period were analyzed. Statistical Analysis: Data were analyzed using descriptive statistics. Kruskal–Wallis and Chi-square test were used to assess relationship between variables. Results: The median age of the cohort was 54 years and interquartile range was 16 years. Nearly 53.6% of patients were illiterate. About 88.10% of patient's had squamous cell carcinoma. Only 13% of cases had early stage disease and 77% of patient's had not taken any treatment before coming to the hospital. Of the total, about 26% patients also had concomitant comorbidities, of which hypertension was found to be the leading comorbid condition. Stage of disease was found to be significantly (P < 0 class="b" xss=removed>Conclusion: This study highlights certain important baseline characteristics of cervical cancer patients. This basic information on profile of patients can help plan and optimum utilization of hospital services, especially in resource-poor countries like India.
Publication History
Article published online:
04 July 2021
© 2017. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Context:
Cancer of the cervix is the most common genital tract malignancy in the female and is a major public health problem in the developing countries. Study of the sociodemographic and clinical profile of patients is the first step in planning control measures and treatment facilities.
Aims:
The aims of the study were to determine the sociodemographic and clinical profile of cervical cancer patients and study their association with other tumor-related factors.
Settings and Design:
This is a record-based retrospective study from a single institution.
Subjects and Methods:
The data on sociodemographic and clinical factors of 765 cervical cancer patients visited and treated at tertiary care cancer hospital in Mumbai in 1 year period were analyzed.
Statistical Analysis:
Data were analyzed using descriptive statistics. Kruskal–Wallis and Chi-square test were used to assess relationship between variables.
Results:
The median age of the cohort was 54 years and interquartile range was 16 years. Nearly 53.6% of patients were illiterate. About 88.10% of patient's had squamous cell carcinoma. Only 13% of cases had early stage disease and 77% of patient's had not taken any treatment before coming to the hospital. Of the total, about 26% patients also had concomitant comorbidities, of which hypertension was found to be the leading comorbid condition. Stage of disease was found to be significantly (P < 0>
Conclusion:
This study highlights certain important baseline characteristics of cervical cancer patients. This basic information on profile of patients can help plan and optimum utilization of hospital services, especially in resource-poor countries like India.
Introduction
Cancer of the cervix is the most common genital tract malignancy in the female and is a major public health problem in the developing countries.[1] Worldwide, about half a million new cases are seen each year, with majority coming from the developing nations. In India, more than 1.2 lac new cases of cancer of cervix uteri occurred in the year 2012 with age-specific incidence rate of 22 per 100,000.[2] It is estimated that cervical cancer will occur in approximately 1 in 53 Indian women during their lifetime compared with 1 in 100 women in more developed regions of the world. At current incidence rates, the annual burden of new cases in India is projected to increase to 225,000 by 2025.[3]
The exact cause of cervical cancer remains unknown. However, it is now well recognized that cervical cancer is more common among women living in poor conditions, with low-income levels and lack of education. There are abundant studies on risk factors related with cervical cancer. In addition to human papillomavirus, there are various risk factors associated with cervical cancer such as early age at marriage, early age at first sexual intercourse, more number of sexual partners, high parity, and smoking.[4,5,6,7] However, information about patients profile and utilization of hospital services is scarce.
In India, huge section of the population is from below poverty line who are neither aware nor have accesses to cervical cancer screening, diagnosis, and treatment facilities. Furthermore, despite cervical cancer being the leading cause of cancer mortality in India, accounting for 17% of all cancer deaths among women aged 30–69 years.[3] There has been no synchronized national initiative from public health authorities. Study of the sociodemographic profile, additional comorbidities, and patient presentation is the first step in planning control measures and treatment facilities. Hence, in light of the above, the present study was planned to study the sociodemographic and clinical profile of cervical cancer patients visiting a tertiary care hospital in Mumbai.
Study design
This is a retrospective study based on hospital records of Tata Memorial Hospital, Mumbai, India.
Study population
Medical records of 765 cervical cancer patients reported to Tata Memorial Hospital, Mumbai, in 1 year period from January 1, 2007 to December 31, 2007 and treated were retrospectively analyzed. Patients who were registered before the study period and already on treatment were excluded from the study.
Data collection
The sociodemographic and clinical details obtained from the hospital records were age, residential address, religion, marital status, education, occupation status, treatment history, stage, tumor histology, performance status (score), and presence of comorbid conditions.
Statistical analysis
Data were analyzed using descriptive statistics. Kruskal–Wallis and Chi-square test were used to assess relationship between variables. All the analyses were done using Statistical Package for Social Science program (IBM SPSS Statistics for Windows, version 20.0. Armonk, NY: IBM Corp.). P < 0>
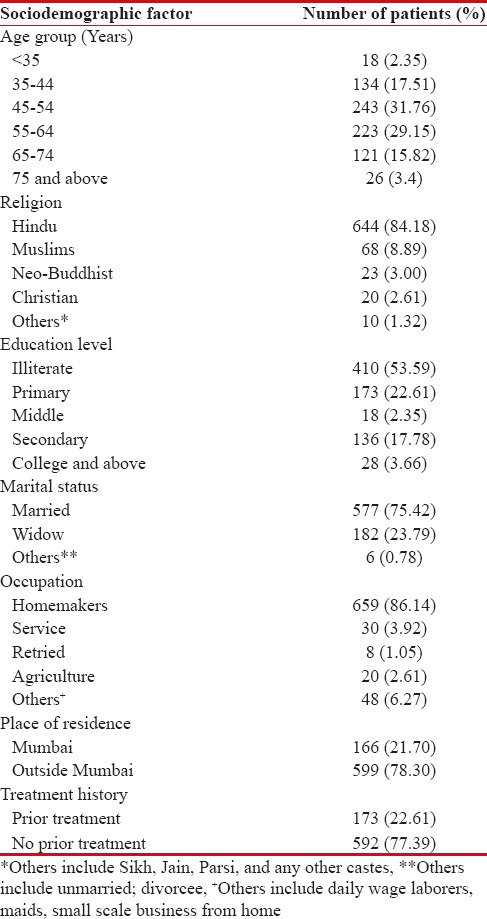
A total of 765 cervical cancer patients were included in this study. Table 1 portrays the sociodemographic profile of cervical cancer patients. Majority of the patients were in the age group of 45–54 (31.76%), followed by 55–64 (29.15%) and only one-fifth of the patients (19.87%) were below the age of 45. The median age of patients was found to be 54 years with interquartile range of 16 years. Most of the patients were Hindus (84.18%), followed by Muslims (8.89%) and very few (6.93%) were from other communities. More than half of the patients were illiterate (53.59%) and only 3.66% of the patients had completed college level education. Nearly 75.42% of patients were married, 23.79% were widows, and only 1 (0.13%) patient reported herself unmarried. Majority of the patients were homemakers (86.14%) and only 3.92% women reported to be employed in some job. Place of residence was categorized into two categories: Mumbai and outside Mumbai.[8,9,10] All those who were residing in Mumbai for more than 1 year were considered as resident of Mumbai. About 22% of patients were found to be resident of Mumbai. Out of total patients 23% had already taken some kind of cancer treatment before coming to this center [Table 1].
Table 1
Sociodemographic profile of cervical cancer patients
|
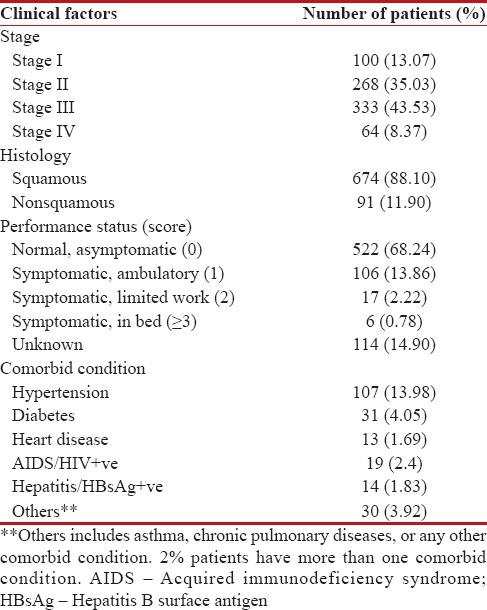
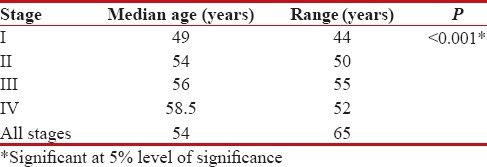
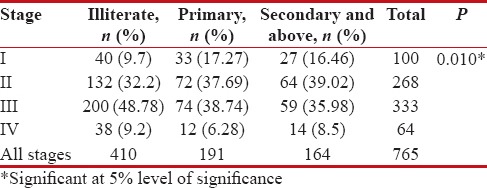
Clinical stage of disease, tumor histology, performance status, and major comorbid conditions were considered to describe the clinical profile of patients. Stage-wise distribution of cervical cancer patients shows that a very small percentage of patients (13%) were diagnosed at early stage. Majority of the patients were diagnosed with Stage 2 (35%) or 3 (43.5%) disease. Nearly 88% of patients had squamous cell carcinoma. Performance status was recorded on the basis of Eastern Cooperative Oncology Group scale. The findings of performance status reveal that about 68% of patients were able to carry out all normal activities without restriction. Moreover, only a very small proportion (<1>Table 2]. Furthermore, we tried to analyze if there is any association between stage of disease and sociodemographic factors such as age and level of education. Stage of disease was found to be significantly (P < 0>[Tables33 and and44].
Table 2
Clinical profile of cervical cancer patients
|
Table 3
Comparison of age with respect to stage
|
Table 4
Association between stage and education
|
Discussion
India is an ethnically diverse country with a growing population of 1.2 billion. In contrast to developed countries, cervical cancer is a major public health problem in India. In developed countries, conventional cytology screening programs have shown a marked decline in the incidence of cervical cancer.[11,12] However, the same not feasible in low-resource settings of our country where a high risk of cervical cancer is experienced. Therefore, a substantial part for cancer control is through early diagnosis and treatment of disease in tertiary cancer care institutes. To plan future control and treatment activities, correct data on patient's sociodemographic profile and clinical presentation are very essential. Hence, this study was conducted to assess various characteristics of patients visiting a tertiary care cancer hospital.
The median age of cervical cancer patients in our study was 54 years, which is similar (54.7 years) to the average age reported by Sankaranarayanan et al.[13] in his study of 452 cervical cancer patients in Kerala. The average age of patients in our study was found to be slightly higher than average reported by other researchers in Western literature.[14] This older age indicates a relative lack of awareness and nonavailability of screening facilities for about cervical cancer in our country.[15,16] However, when the patients were grouped age wise, majority of them belonged to 45–54-year followed by 55–59-year age groups. Similar age-wise distribution has been reported by many researchers.[17,18,19,20,21,22] Our study also found a significant difference in median age of patients when patients were categorized as per stage, i.e., median age of patients with higher stage disease was found to significantly higher than patients with lower stage disease. This finding has been also reported by Flores-Luna et al.[14] Late diagnosis of cervical cancer can be the likely explanation of higher median age of patients with advanced stage disease. Further, it is also likely that the findings reflect differences in awareness of cervical cancer symptoms in older women and/or differences in healthcare-seeking behavior.[23] This suggests that equipping older women with the knowledge, skills, and confidence to present promptly with cervical cancer symptoms might help downstage cervical cancer in older women and thereby improve their survival.
In our study, 54% of patients were illiterate, whereas only 4% have had qualification of college and above. We also found an association between educational status and stage. This finding is in consonance with many studies which has found illiteracy as a risk factor for cervical cancer.[24,25,26] Similarly, lack of education has also been linked early marriage and high parity which are also considered as risk factors for cervical cancer, thus improving the educational status of women in our country is an essential component of holistic approach for cervical cancer control in India. In addition, improving in living standards and formulating public health policies aimed at increasing awareness and coverage of cervical cancer screening programs would go a long way in reducing cervical cancer in our country.[24] We found that 75.42% patients were currently married, which is higher than 62.4% reported by Sankaranarayanan et al.[13] but lower than 88.61% reported by Thulaseedharan et al.[18] Of the total, 26% patients also had concomitant comorbidities, of which hypertension was found to be the leading comorbid condition. Prevalence of comorbid conditions reported in this study was higher than reported by Ibfelt et al.[19] Distribution of religion reported in this study is similar to results obtained by other authors.[15]
In our study, 13%-cases had early stage disease (Stage I) and more than 50%-patients had presented with advanced stage disease (Stage III and IV). Similar stage-wise distribution has been reported by Nandakumar et al. in their population cancer registry-based study conducted in Bengaluru[16] and Shrivastava et al. in their retrospective study of 6234 patients.[27] Histologically, majority (88.10%) of our patients had squamous cell carcinoma which is similar to results obtained by many other researchers.[19,28] Nearly 68% of our patients were fully active (performance status 0); these figures are much lower than 81%-and 91.82%-fully active performance status reported by Sankaranarayanan et al.,[13] i.e., 81% by Vishma Baliyada Kaverappa et al. (2015)[26] 91.82%.
There were several limitations of our study which need to be acknowledged. Our study was not able to reflect some important characteristics such as patient's socioeconomic status and family income. Furthermore, this study failed to report time of incidence of comorbid conditions. These limitations are because the study was based on secondary data and only those factors which were recorded in the medical documents have been taken into consideration. Nevertheless, the strength of this study lies in the fact that there are very few Indian studies which have described patient's sociodemographic profile, and clinical profile as well as explore the relationship between patient's characteristics and tumor-related factors.
Conclusion
In India, there are very few studies describing profile of cancer patients visiting health-care facilities. This basic information on profile of patients can help to plan and ensure efficient utilization of hospital services in resource-poor countries like India. Further, the scope of studying sociodemographic factors is not limited to hospital services, and this information can also be utilized while making public health policies and implementation of cervical cancer control programs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Awodele O, Adeyomoye AA, Awodele DF, Kwashi V, Awodele IO, Dolapo DC, et al. A study on cervical cancer screening amongst nurses in Lagos university teaching hospital, Lagos, Nigeria. J Cancer Educ 2011;26:497-504.
- Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, et al. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC Cancer Base No. 11. Lyon, France: International Agency for Research on Cancer; 2013. Available from: http://www.globocan.iarc.fr. [Last accessed on 2015 Aug 03].
- Institute for Health Metrics and Evaluation. The Challenge Ahead: Progress in Breast and Cervical Cancer. Institute of Health Metrics and Evaluation; 2011. Available from: http://www.healthmetricsandevaluation.org/publications/policyreport/challenge-ahead-progress-and-setbacks-breastand-cervical-cancer. [Last accessed on 2013 Jan 21].
- International Collaboration of Epidemiological Studies of Cervical Cancer. Comparison of risk factors for invasive squamous cell carcinoma and adenocarcinoma of the cervix: Collaborative reanalysis of individual data on 8,097 women with squamous cell carcinoma and 1,374 women with adenocarcinoma from 12 epidemiological studies. Int J Cancer 2007;120:885-91.
- Franceschi S, Plummer M, Clifford G, de Sanjose S, Bosch X, Herrero R, et al. Differences in the risk of cervical cancer and human papillomavirus infection by education level. Br J Cancer 2009;101:865-70.
- Green J, Berrington de Gonzalez A, Sweetland S, Beral V, Chilvers C, Crossley B, et al. Risk factors for adenocarcinoma and squamous cell carcinoma of the cervix in women aged 20-44 years: The UK national case-control study of cervical cancer. Br J Cancer 2003;89:2078-86.
- Rajkumar T, Franceschi S, Vaccarella S, Gajalakshmi V, Sharmila A, Snijders PJ, et al. Role of paan chewing and dietary habits in cervical carcinoma in Chennai, India. Br J Cancer 2003;88:1388-93.
- Balasubramaniam G, Sushama S, Rasika B, Mahantshetty U. Hospital-based study of endometrial cancer survival in Mumbai, India. Asian Pac J Cancer Prev 2013;14:977-80.
- Balasubramaniam G, Talole S, Mahantshetty U, Saoba S, Shrivastava S. Prostate cancer: A hospital-based survival study from Mumbai, India. Asian Pac J Cancer Prev 2013;14:2595-8.
- Ganesh B, Swaminathan R, Mathew A, Sankaranarayanan R, Hakama M. Loss-adjusted hospital and population-based survival of cancer patients. IARC Sci Publ 2011;162:15-21.
- IARC. Handbooks on Cancer Prevention. Cervix Cancer Screening. Vol. 10. Lyon: IARC Press; 2004.
- Sankaranarayanan R, Budukh AM, Rajkumar R. Effective screening programmes for cervical cancer in low- and middle-income developing countries. Bull World Health Organ 2001;79:954-62.
- Sankaranarayanan R, Nair MK, Jayaprakash PG, Stanley G, Varghese C, Ramadas V, et al. Cervical cancer in Kerala: A hospital registry-based study on survival and prognostic factors. Br J Cancer 1995;72:1039-42.
- Flores-Luna L, Salazar-Martinez E, Escudero-De los Rios P, Gonzalez-Lira G, Zamora-Muñoz S, Lazcano-Ponce E, et al. Prognostic factors related to cervical cancer survival in Mexican women. Int J Gynaecol Obstet 2001;75:33-42.
- Kaverappa VB, Prakash B, Kulkarni P, Renuka M. Sociodemographic profile of patients with cervical cancer in a tertiary-care cancer hospital in Mysuru, Karnataka. Int J Med Sci Public Health 2015;4:1187-90.
- Nandakumar A, Anantha N, Venugopal TC. Incidence, mortality and survival in cancer of the cervix in Bangalore, India. Br J Cancer 1995;71:1348-52.
- Rajarao P, Hemanth Kumar B. Study of socio demographic profile of cancer cervix patients in tertiary care hospital, Karimnagar (Andhra Pradesh). Int J Biol Med Res 2012;3:2306-10.
- Thulaseedharan JV, Malila N, Hakama M, Esmy PO, Cheriyan M, Swaminathan R, et al. Socio demographic and reproductive risk factors for cervical cancer – A large prospective cohort study from rural India. Asian Pac J Cancer Prev 2012;13:2991-5.
- Ibfelt EH, Kjær SK, Høgdall C, Steding-Jessen M, Kjær TK, Osler M, et al. Socioeconomic position and survival after cervical cancer: Influence of cancer stage, comorbidity and smoking among danish women diagnosed between 2005 and 2010. Br J Cancer 2013;109:2489-95.
- National Cancer Registry Programme (NCRP), Indian Council of Medical Research (ICMR). An Assessment of the Burden and Care of Cancer Patients: Consolidated Report of Hospital Based Cancer Registries, 2001-2003. Bangalore: NCRP, ICMR; 2007. Available from: http://www.icmr.nic.in/ncrp/cancer_reg.htm. [Last accessed on 2015 Feb 21].
- Rajesh N, Sreelakshmi K, Ramesh K. Sociodemographic profile of patients with cancer of cervix attending tertiary care hospital. Int J Sci Res 2014;3:331-2.
- Fotra R, Gupta S, Gupta S. Sociodemographic risk factors for cervical cancer in Jammu region of J and K state of India first ever report from Jammu. Indian J Sci Res 2014;9:105-10.
- Ertem G. Awareness of cervical cancer risk factors and screening behaviour among nurses in a rural region of turkey. Asian Pac J Cancer Prev 2009;10:735-8.
- Thakur A, Gupta B, Gupta A, Chauhan R. Risk factors for cancer cervix among rural women of a hilly state: A case-control study. Indian J Public Health 2015;59:45-8.
- Patil V, Wahab SN, Zodpey S, Vasudeo ND. Development and validation of risk scoring system for prediction of cancer cervix. Indian J Public Health 2006;50:38-42.
- Kaverappa VB, Boralingaiah P, Kulkarni P, Manjunath R. Determinants of survival among patients with cervical cancer: A hospital based study. Natl J Community Med 2015;6:4-9.
- Shrivastava S, Mahantshetty U, Engineer R, Tongaonkar H, Kulkarni J, Dinshaw K. Treatment and outcome in cancer cervix patients treated between 1979 and 1994: A single institutional experience. J Cancer Res Ther 2013;9:672-9.
- Kumar S, Rana ML, Verma K, Singh N, Sharma AK, Maria AK, et al. PrediQt-cx: Post treatment health related quality of life prediction model for cervical cancer patients. PLoS One 2014;9:e89851.
References
- Awodele O, Adeyomoye AA, Awodele DF, Kwashi V, Awodele IO, Dolapo DC, et al. A study on cervical cancer screening amongst nurses in Lagos university teaching hospital, Lagos, Nigeria. J Cancer Educ 2011;26:497-504.
- Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, et al. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC Cancer Base No. 11. Lyon, France: International Agency for Research on Cancer; 2013. Available from: http://www.globocan.iarc.fr. [Last accessed on 2015 Aug 03].
- Institute for Health Metrics and Evaluation. The Challenge Ahead: Progress in Breast and Cervical Cancer. Institute of Health Metrics and Evaluation; 2011. Available from: http://www.healthmetricsandevaluation.org/publications/policyreport/challenge-ahead-progress-and-setbacks-breastand-cervical-cancer. [Last accessed on 2013 Jan 21].
- International Collaboration of Epidemiological Studies of Cervical Cancer. Comparison of risk factors for invasive squamous cell carcinoma and adenocarcinoma of the cervix: Collaborative reanalysis of individual data on 8,097 women with squamous cell carcinoma and 1,374 women with adenocarcinoma from 12 epidemiological studies. Int J Cancer 2007;120:885-91.
- Franceschi S, Plummer M, Clifford G, de Sanjose S, Bosch X, Herrero R, et al. Differences in the risk of cervical cancer and human papillomavirus infection by education level. Br J Cancer 2009;101:865-70.
- Green J, Berrington de Gonzalez A, Sweetland S, Beral V, Chilvers C, Crossley B, et al. Risk factors for adenocarcinoma and squamous cell carcinoma of the cervix in women aged 20-44 years: The UK national case-control study of cervical cancer. Br J Cancer 2003;89:2078-86.
- Rajkumar T, Franceschi S, Vaccarella S, Gajalakshmi V, Sharmila A, Snijders PJ, et al. Role of paan chewing and dietary habits in cervical carcinoma in Chennai, India. Br J Cancer 2003;88:1388-93.
- Balasubramaniam G, Sushama S, Rasika B, Mahantshetty U. Hospital-based study of endometrial cancer survival in Mumbai, India. Asian Pac J Cancer Prev 2013;14:977-80.
- Balasubramaniam G, Talole S, Mahantshetty U, Saoba S, Shrivastava S. Prostate cancer: A hospital-based survival study from Mumbai, India. Asian Pac J Cancer Prev 2013;14:2595-8.
- Ganesh B, Swaminathan R, Mathew A, Sankaranarayanan R, Hakama M. Loss-adjusted hospital and population-based survival of cancer patients. IARC Sci Publ 2011;162:15-21.
- IARC. Handbooks on Cancer Prevention. Cervix Cancer Screening. Vol. 10. Lyon: IARC Press; 2004.
- Sankaranarayanan R, Budukh AM, Rajkumar R. Effective screening programmes for cervical cancer in low- and middle-income developing countries. Bull World Health Organ 2001;79:954-62.
- Sankaranarayanan R, Nair MK, Jayaprakash PG, Stanley G, Varghese C, Ramadas V, et al. Cervical cancer in Kerala: A hospital registry-based study on survival and prognostic factors. Br J Cancer 1995;72:1039-42.
- Flores-Luna L, Salazar-Martinez E, Escudero-De los Rios P, Gonzalez-Lira G, Zamora-Muñoz S, Lazcano-Ponce E, et al. Prognostic factors related to cervical cancer survival in Mexican women. Int J Gynaecol Obstet 2001;75:33-42.
- Kaverappa VB, Prakash B, Kulkarni P, Renuka M. Sociodemographic profile of patients with cervical cancer in a tertiary-care cancer hospital in Mysuru, Karnataka. Int J Med Sci Public Health 2015;4:1187-90.
- Nandakumar A, Anantha N, Venugopal TC. Incidence, mortality and survival in cancer of the cervix in Bangalore, India. Br J Cancer 1995;71:1348-52.
- Rajarao P, Hemanth Kumar B. Study of socio demographic profile of cancer cervix patients in tertiary care hospital, Karimnagar (Andhra Pradesh). Int J Biol Med Res 2012;3:2306-10.
- Thulaseedharan JV, Malila N, Hakama M, Esmy PO, Cheriyan M, Swaminathan R, et al. Socio demographic and reproductive risk factors for cervical cancer – A large prospective cohort study from rural India. Asian Pac J Cancer Prev 2012;13:2991-5.
- Ibfelt EH, Kjær SK, Høgdall C, Steding-Jessen M, Kjær TK, Osler M, et al. Socioeconomic position and survival after cervical cancer: Influence of cancer stage, comorbidity and smoking among danish women diagnosed between 2005 and 2010. Br J Cancer 2013;109:2489-95.
- National Cancer Registry Programme (NCRP), Indian Council of Medical Research (ICMR). An Assessment of the Burden and Care of Cancer Patients: Consolidated Report of Hospital Based Cancer Registries, 2001-2003. Bangalore: NCRP, ICMR; 2007. Available from: http://www.icmr.nic.in/ncrp/cancer_reg.htm. [Last accessed on 2015 Feb 21].
- Rajesh N, Sreelakshmi K, Ramesh K. Sociodemographic profile of patients with cancer of cervix attending tertiary care hospital. Int J Sci Res 2014;3:331-2.
- Fotra R, Gupta S, Gupta S. Sociodemographic risk factors for cervical cancer in Jammu region of J and K state of India first ever report from Jammu. Indian J Sci Res 2014;9:105-10.
- Ertem G. Awareness of cervical cancer risk factors and screening behaviour among nurses in a rural region of turkey. Asian Pac J Cancer Prev 2009;10:735-8.
- Thakur A, Gupta B, Gupta A, Chauhan R. Risk factors for cancer cervix among rural women of a hilly state: A case-control study. Indian J Public Health 2015;59:45-8.
- Patil V, Wahab SN, Zodpey S, Vasudeo ND. Development and validation of risk scoring system for prediction of cancer cervix. Indian J Public Health 2006;50:38-42.
- Kaverappa VB, Boralingaiah P, Kulkarni P, Manjunath R. Determinants of survival among patients with cervical cancer: A hospital based study. Natl J Community Med 2015;6:4-9.
- Shrivastava S, Mahantshetty U, Engineer R, Tongaonkar H, Kulkarni J, Dinshaw K. Treatment and outcome in cancer cervix patients treated between 1979 and 1994: A single institutional experience. J Cancer Res Ther 2013;9:672-9.
- Kumar S, Rana ML, Verma K, Singh N, Sharma AK, Maria AK, et al. PrediQt-cx: Post treatment health related quality of life prediction model for cervical cancer patients. PLoS One 2014;9:e89851.


 PDF
PDF  Views
Views  Share
Share

