Status of barium studies in the present era of oncology: Are they a history?
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2016; 37(04): 223-226
DOI: DOI: 10.4103/0971-5851.195740
Abstract
With the advent of the modern imaging technologies, the present era of oncology is seeing steady decline in requests for barium studies due to the many reasons. It is prudent to mention here, that, barium examinations cannot be made obsolete! Our aim to preserve the age old technique of barium studies not only to keep it going on but also for the betterment and appropriate management of the patient. Our goal is not to “save” barium studies simply to keep this technology alive, per se, but rather to preserve barium radiology for the quality in patient care.
Publication History
Article published online:
12 July 2021
© 2016. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
With the advent of the modern imaging technologies, the present era of oncology is seeing steady decline in requests for barium studies due to the many reasons. It is prudent to mention here, that, barium examinations cannot be made obsolete! Our aim to preserve the age old technique of barium studies not only to keep it going on but also for the betterment and appropriate management of the patient. Our goal is not to “save” barium studies simply to keep this technology alive, per se, but rather to preserve barium radiology for the quality in patient care.
INTRODUCTION
Barium as a positive radiographic contrast medium for evaluation of gastrointestinal disorders has historically been associated with the first application of X-rays in medicine. It formed the mainstay as a primary diagnostic modality to investigate disorders of the gastrointestinal tract.[1] Various improvisations in the composition of barium and its techniques (high density, double contrast) allowed accurate anatomical depiction. Technical innovations in the form of image intensification, automatic exposure, automatic film processor systems, etc., provided ease in performing such tedious procedures. There were, however, concerns regarding the excessive exposure of ionizing radiation to both, the radiologist and the patient.[2,3] The advent of ultrasonography, endoscopy, capsule endoscopy, physiological monitoring, and axial imaging (computed tomography [CT] and magnetic resonance [MR] scanning) relegated the superiority of barium examinations.[2,3]
Over the last 30 years, there has been a steady decline in requests for barium studies due to the above reasons. Now, barium meal evaluation of stomach and small bowel is performed only in teaching institutions and in mofussil areas, where there is dearth of modern imaging facilities. The art of barium examination is seldom seen in any major institution. This art comes with practice and with dwindling number of investigations asked for; there is no time to master the same. Being operator depended, the clinicians would not trust the studies performed by juniors and would thus seek their answers from the gamut of other investigations available. Mastering the art of barium examination is time consuming and in the present economic trends, is not cost-effective.[4,5] Seniors are few, who know the technique well enough to teach. With passage time, there will be nobody who would be able to perform an appropriate and optimal barium examination. Furthermore, the present generation of clinicians and radiologists rely more on endoscopy and axial imaging, and would not like to spend more time in the time-consuming barium examinations.
This decline of barium investigations has had negative repercussions on the residency training programs as they are not aware of the proper techniques, advantages, and limitations of the study. In odd cases where one is forced to perform such an investigation, they would be on tender hooks to go about it and perform a shoddy study.
IT IS PRUDENT TO MENTION HERE, THAT, BARIUM EXAMINATIONS CANNOT BE MADE OBSOLETE!
There are areas where endoscopy, axial imaging, and physiologic monitoring are inadequate; they are invasive, time consuming, expensive, and not without their shortfallings, ambiguity, and complications.[2,3] It is primarily the financially driven initiatives that have propagated the use of other complementary modalities as a primary modality(s) of choice over the conventional barium examination. Barium studies, till date, remains the safest, fastest, and cheapest diagnostic investigation to evaluate vague abdominal symptoms and the art has to be revived.[4,5] Motility disorders of the gastrointestinal tract from pharynx to anus and submucosal lesions are best and quickly evaluated by barium studies. No other modality can be as faster, safer, and more accurate than this age-old barium evaluation.[4,5] The role of barium evaluation of the bowel in patients with malabsorption is irrefutable. It is useful for both, diagnostic as well as for follow-up to evaluate response to therapy.[5,6]
Other specialties such as speech therapy and the ear-nose and throat, also require barium studies for accurate anatomic depiction by barium studies for the detection of vocal cord movements, artificial voice box evaluation, and other benign conditions such as diverticulum. The real-time evaluation of the upper digestive tract by barium is a boon for them as it resolves many ambiguous disorders. However, for staging purposes in esophageal cancers, almost all esophageal disorders can be diagnosed by barium swallow examination. There is no other cheaper modality that can stake this claim.[4,5,6]
Barium study is a quick investigation to evaluate response to treatment and to evaluate the postoperative status and their complications in gastroenterology, being a faster and cheaper investigation.[6] In our institution, we perform a large number of loopogram (distal and proximal) using barium before closure to external bowel diversion.
To perform even a simple and easy study such as loopogram, one needs to be aware of basics and basis of the use of barium studies in tubular structures such as mucosal coating, distension, the barium pool, projections, and compression to optimize visualization of abnormalities at single- and double-contrast studies.[6]
TATA MEMORIAL CENTER EXPERIENCE
At Tata Memorial Hospital, we evaluated the audit data over 10 years from January 2006 to December 2015. The data were divided into three groups, namely, barium swallows, barium meals, and enemas and others (enteroclysis, loopogram, and cologram). Being a tertiary cancer center and with the availability of most of the latest imaging technologies, we were seldom performing barium studies for the primary evaluation of the stomach and colon. The trends over the period were reviewed, and analysis was done. There has been a slow but steady decline in the number of barium studies performed in our hospital over the past 10 years. In our institute, we found a trend of overall decrease in the number of barium studies from 2989 to 672 in 10 years with 76% regression. Out of all the barium studies, the major decline was seen in the number of barium swallows which went down from 2801 to 471 in 10 years with an approximately 83% decrease over interval period [Figure 1].
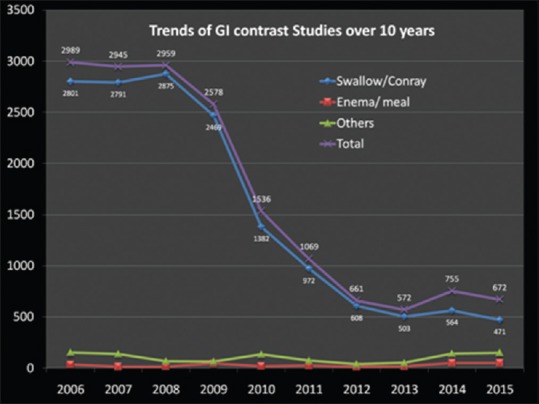
| Fig. 1 Trends of barium studies performed in our hospital over the past 10 years. Overall, 76% regression in the number of barium studies with a major decline seen in the number of barium swallows being performed having 83% decrease
The decline is probably due to the fact that ours is a tertiary cancer center where most of the cases are already worked by basic imaging investigations outside. Similar trends are seen in the United States. In the data published by Medicare, during a 3-year period (1999–2001), there was approximately 33% decrease in the number of double-contrast barium enema (DCBE) for colorectal cancer screening, and in 2008, the U.S. Preventive Services Task Force recommendations for colorectal cancer screening guidelines the use of DCBE is omitted.[7,8] One of the many postulated reasons for the decline of use of DCBE, the most important are (1) wider availability and increasing use of cross-sectional imaging tests, such as abdominal CT and MR imaging (MRI), (2) higher sensitivity and specificity of CT and MRI in detecting polyps, (3) alternatives such as CT- and MRI-based virtual colonoscopy, and (4) very few trained radiologist who can perform and interpret this technique and teach radiology trainee for performing such procedures.[9,10] Not surprisingly, there was a slight increase in the number of loopogram, reflecting the increase in surgical intervention. The decline of barium evaluation of esophagus, stomach, and small bowel is attributed to diverse factors including the ever-increasing accessibility of endoscopy and sophisticated cross-sectional imaging modalities such as CT and MRI.[10]
At our institution, barium studies are now used primarily to evaluate the pharynx, larynx, and cervical anastomosis and to evaluate the external bowel diversion loop before closure. For accurate anatomic delineation of the lesion, our radiotherapy department still uses the lateral barium study for the neck at six feet distance, for the larynx and pharynx. Similarly, many centers across the world still use contrast swallow studies for the assessment of anastomotic leaks, and in a recent study by Price et al. showed that barium swallow is a specific test for detecting anastomotic leaks after esophagectomy.[11,12,13] Rarely, we have had to resort to enteroclysis; for the odd cases, a routine barium follows through examination sufficed.
Tata Memorial Centre (TMC) grant in aid under DAE is one of the largest comprehensive cancer centers in Asian subcontinent. TMC commissioned a model rural cancer control program titled “TMC – Rural Outreach Program” (TMCROP) in Southern Maharashtra districts (approximate population 3 million) in the Western part of India in 2002. From 2008, we introduced barium swallow examination, a faster and cheaper investigation for early esophageal cancer detection, as a primary tool for screening program in our TMCROP.[14]
TO RESURRECT BARIUM STUDIES
Besides, being a primary diagnostic tool for many upper gastrointestinal disorders, these barium fluoroscopic examinations also have an important role in the evaluation of patients after gastrointestinal surgery (including postesophagectomy and anastomosis surgery) and in the diagnosis of a host of postoperative complications (e.g., perforation and obstruction). Hence, in the era of personalised cancer medicine and molecular functional imaging there is a need to revitalize barium studies that have been ignored for a long time.[4,5,6,15,16]
Importantly, there is a need to interact proactively with the clinicians who are our feeders. Joint discussions should be held, and it must be emphasized to them that other imaging modalities are complementary to barium studies and that there are many instances whereby, this cheaper and faster investigation would be beneficial to the patient. They must be coerced, and we should demonstrate a good study to encourage them to look our way.[4,6]
Another problem that needs to be resolved is that of the available literature. Newer books on imaging do not lay sufficient stress on the various techniques of performing barium studies; whatever little they may add, is insufficient. It is not that barium examination can be mastered by reading books or through the internet. It is the older editions on the subject that describe in depth the nuances in the performance of barium studies. The tenets of barium examination can be understood well. Hence, it is the need to preserve older textbooks that describe these procedures in depth. They also contain more illustrations than the newer ones, as other modalities were not in vogue then.
The institution also plays an important role in regard with sanctioning of grants for fluoroscopic equipment. They too must be made aware of the fact that fluoroscopic equipment for barium studies is a must in the armamentarium of the radiodiagnosis department. Money should be spent not only on such equipment but also for the other modern and latest equipment.
Finally, to gather experience, junior doctors need to weed out frank cases to perform barium examination on diagnosed cases for applying and learning the art of barium studies, and importantly, the art of fluoroscopy. Unlike vascular and interventional studies, fluoroscopy is an art in barium examination where one does not try to diagnose lesions on fluoroscopy. Fluoroscopy is performed to see adequacy of contrast coating, its passage, and to record images of lesions (suspicious or obvious) in orthogonal views.
CONCLUSION
Our aim to preserve the age-old technique of barium studies not only to keep it going on but also for the betterment and appropriate management of the patient. Our goal is not to “save” barium studies simply to keep this technology alive, per se, but rather to preserve barium radiology for the quality in patient care.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
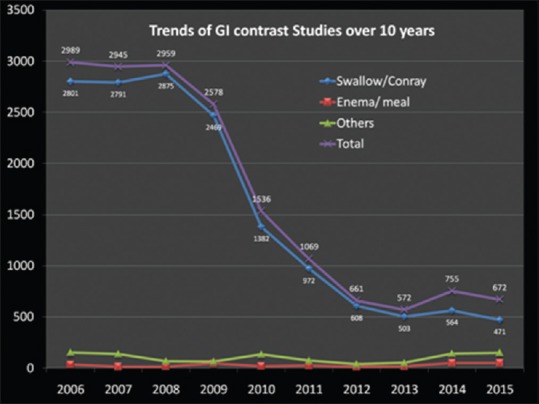
| Fig. 1 Trends of barium studies performed in our hospital over the past 10 years. Overall, 76% regression in the number of barium studies with a major decline seen in the number of barium swallows being performed having 83


 PDF
PDF  Views
Views  Share
Share

