The Role of Chronic Mucosal Trauma in Oral Cancer: A Review of Literature
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2017; 38(01): 44-50
DOI: DOI: 10.4103/0971-5851.203510
Abstract
Chronic mucosal trauma resulting from sharp teeth, dentures, faulty restoration, or implants has frequently been associated with the development of oral cancer. The definitive evidence for the same is lacking. We undertook a search using the terms – dental trauma, mucosal trauma, oral cancer, squamous cell carcinoma, risk factor, potentially malignant lesion, dental factor, mechanical irritation, dental irritation, and cancer in the following electronic databases: MEDLINE, PubMed, ScienceDirect, Cochrane Database of Systematic Reviews, and Wiley InterScience. The search yielded 788 articles. Of these articles, only 22 articles described chronic mucosal trauma as risk factors for oral cancers and were considered in this review. The review shows that chronic mucosal irritation resulting from ill-fitting dentures may be considered a risk factor for the development of oral cancer, such cancers occur commonly over the lateral border of the tongue. However, no association has been proven between the duration of denture use and cancer formation. In patients without any addiction, such cancers occur more frequently in females. These cancers may present with an early nodal disease but their prognosis and outcomes have not been studied separately till now.
Keywords
Dental trauma - etiology - mucosal trauma - oral cancer - risk factor - squamous cell carcinomaPublication History
Article published online:
06 July 2021
© 2017. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Chronic mucosal trauma resulting from sharp teeth, dentures, faulty restoration, or implants has frequently been associated with the development of oral cancer. The definitive evidence for the same is lacking. We undertook a search using the terms – dental trauma, mucosal trauma, oral cancer, squamous cell carcinoma, risk factor, potentially malignant lesion, dental factor, mechanical irritation, dental irritation, and cancer in the following electronic databases: MEDLINE, PubMed, ScienceDirect, Cochrane Database of Systematic Reviews, and Wiley InterScience. The search yielded 788 articles. Of these articles, only 22 articles described chronic mucosal trauma as risk factors for oral cancers and were considered in this review. The review shows that chronic mucosal irritation resulting from ill-fitting dentures may be considered a risk factor for the development of oral cancer, such cancers occur commonly over the lateral border of the tongue. However, no association has been proven between the duration of denture use and cancer formation. In patients without any addiction, such cancers occur more frequently in females. These cancers may present with an early nodal disease but their prognosis and outcomes have not been studied separately till now.
ntroduction
Oral cancer is among the commonly seen cancers in the world. Each year, about 300,000 new cases of oral cancer are detected worldwide. It also leads to about 145,000 deaths annually.[1] Five-year survival of patients with early oral cancer is between 55% and 60% and it decreases to 30% and 40% in cases of advanced oral cancer. These cancers are associated with the use of tobacco, betel quid, areca nut, smoking, and alcohol consumption.[2,3,4] In addition to these, long-standing irritation has been postulated as a risk factor. Chronic irritation may result from poor oral hygiene,[5] poor dentition,[6] missing teeth,[7] and ill-fitting dentures.[8] However, the role of these conditions in developing oral cancer has been debatable. We, therefore, decided to conduct a review of literature to evaluate the role of chronic irritation resulting from these conditions in causing oral cancer.
Methodology
A systematic search of the databases MEDLINE (from 1950), PubMed (from 1946), Cochrane Database of Systematic Reviews (from 2005), Web of Science, and PubMed (from 1950) through September 2016 was done. Relevant articles were identified. The search terms used were “dental trauma,” “mucosal trauma,” “oral cancer,” “squamous cell carcinoma,” “risk factor,” “potentially malignant lesion,” “dental factor,” “mechanical irritation,” “dental irritation,” and “cancer.” These were searched as text word and as subject headings individually as well as in different combination. The reference lists of relevant articles were also searched for appropriate studies. No language restrictions were used in either the search or study selection. This search yielded 788 articles. Articles were excluded from the review if they failed to describe the factors of interest for the study. Among these articles, only 22 articles described chronic mucosal trauma as risk factors for oral cancers and were considered in this review.
Literature Review
Chronic irritation has been proposed to be an etiological factor for oral cancer, but we could not find any Level 1 evidence to support this hypothesis. During review of literature, we found retrospective case–control and descriptive studies and a few case series exploring its association with carcinogenesis. Mucosal trauma in oral cavity may be due to ill-fitting denture, broken teeth, sharp teeth, overhanging restoration, and rarely due to implants.
Mechanism of Carcinogenesis Following Mucosal Trauma
Many studies have been done to evaluate the role of chronic trauma in carcinogenesis. Experimental animal studies have suggested that chronic trauma may result in cancer formation by two mechanisms. It has been proposed that persistent mechanical irritation causes DNA damage and may eventually result in cancer formation. This has been proven by increased activity of poly-ADP-ribose polymerase[9] in cases with chronic trauma.
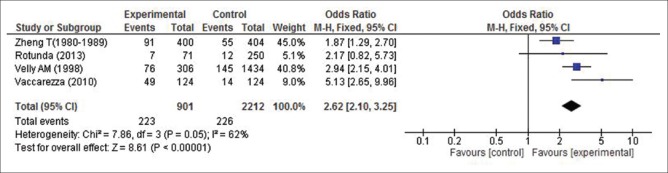
According to second proposed mechanism, chronic mucosal trauma results in inflammation, thereby releasing chemical mediators such as cytokine, prostaglandins, and tumor necrosis factor. Such an inflammation leads to oxidative stress.[10] This could induce genetic and epigenetic changes damaging DNA, inhibiting its repair, altering transcription factors, preventing apoptosis, and stimulating angiogenesis, thus resulting in carcinogenesis. In a nutshell, inflammation may act at different steps and result in cancer formation.[11,12] [Figure 1]
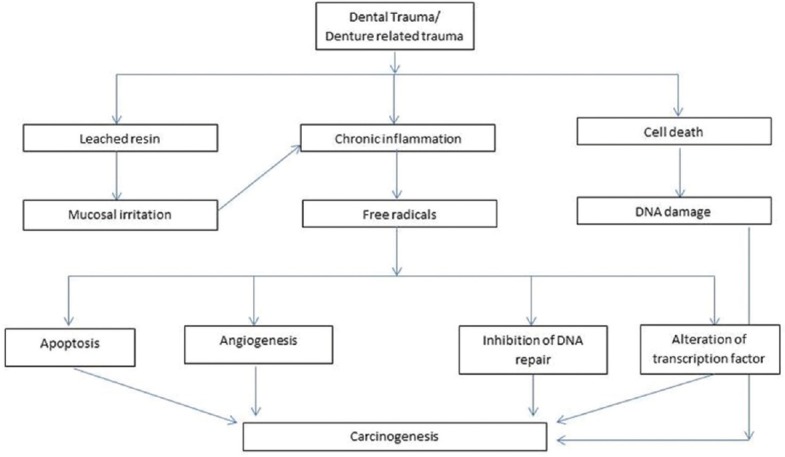
| Figure 1:Proposed hypothesis of mechanism of carcinogenesis following chronic mucosal trauma
Site of Oral Cancer Associated With Dental Trauma
In a retrospective study from Australia,[13] it was found that the lateral border of tongue was the most common site of tumor occurrence in both smokers and nonsmokers. The incidence of tumor occurrence in lateral border of tongue was twice as common in nonsmokers as compared to smokers. This suggests that lateral border of tongue could be a site for chronic dental trauma. In a Brazilian-Canadian[14] study, association of chronic mucosal trauma with oral cancer was primarily linked to tongue neoplasm to the odds ratio (OR) = 9.1 (confidence interval [CI] = 1.9–43.4).
In an another study,[15] which examined a series of 28 oral malignant neoplasms, it was found that all these neoplasms occurred in areas of contact with teeth and/or dental appliances. This very strong association observed between trauma and cancer formation in this study could be because it was conducted mainly in a dental setup, so probably that is why that all the patients had dental trauma related cancers. One-third of these cancers occurred at the lateral border of tongue. On the contrary, another study[16] examining 67 oral cancer patients without any addiction found that the majority of oral cancers were on the alveolar arch. Thus, from available literature, it may be considered that lateral border of the tongue is the most frequent site of chronic trauma associated oral cancer.
Ill-Fitting Denture and Oral Cancer
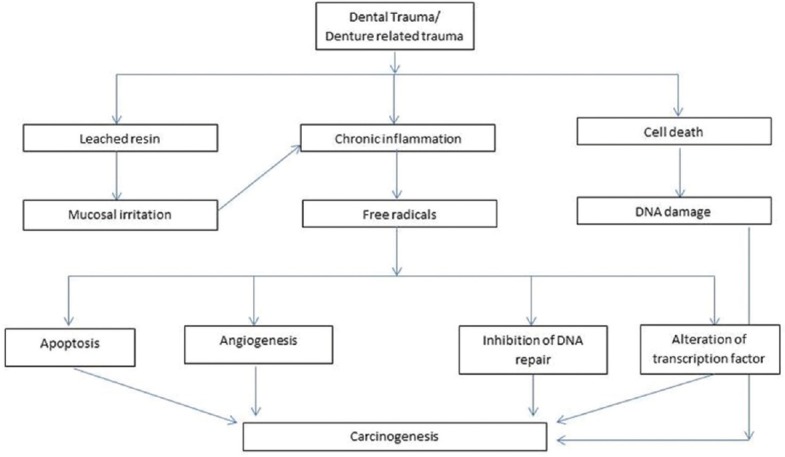
Denture use has often been considered as a cause of chronic mucosal insult and subsequent cancer formation. Several studies have proven such an association. In a population-based case–control study conducted in Sweden,[17] a multivariate analysis showed that defective or malfunctioning complete dentures were significant risk factors (OR = 3.8; 95% CI = 1.3–11.4) for the development of oral squamous cell carcinoma. However, in this study, poor oral hygiene was found to be more strongly associated with oral cancer with the OR = 5.3 (95% CI = 2.5–11.3). In a hospital-based case–control study in São Paulo, Brazil,[18] association between ill-fitting dentures and oral cancer was statistically significant in the multivariate model: OR = 3.98; (95% CI = 1.06–14.96). They went a step further and found a specific assessment of association between tumors in the lower jaw and mucosal trauma by mandibular dentures with OR = 6.39; (95% CI = 1.49–29.5). Specific assessment of maxillary denture associated mucosal injury was not done in this study. In another multivariate analysis[19] conducted in Brazil, it was found that ill-fitting denture-associated sores were associated with oral cancer with adjusted OR = 4.58; CI = 1.52–13.76 (P = 0.007). They concluded that chronic physical irritation of oral mucosa contributes to the topical carcinogenic effect of tobacco. In a meta-analysis,[8] the use of dentures by itself was associated with an increased risk of developing cancer (OR = 1.42, 95% CI = 1.01–1.99) while ill-fitting dentures appeared to substantially increase the risk of developing cancer by almost four times (pooled OR = 3.90, 95% CI = 2.48–6.13) [Figure 2].
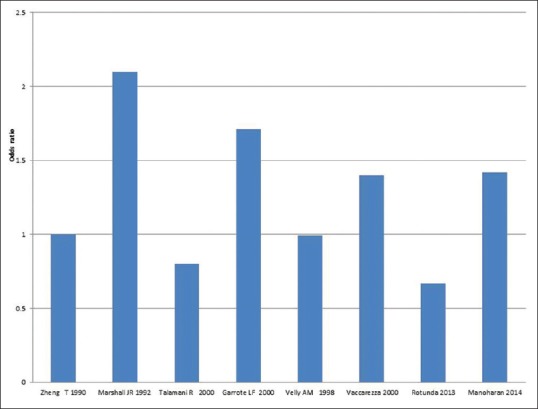
| Figure 2:Studies showing odds ratio of denture as a risk factor for oral cancer (adjusted for confounders)
Another study suggested that 44% of the patients showed a correlation between the site of cancer development and the site of some form of chronic dental irritation. However, it did not separate the smoking population from the nonsmoking population.[20] Another case–control study studying the role of dental prosthesis in alveolar cancer found that denture use was associated with cancer with OR = 2.28. When adjusted for confounding factors, OR was found to be 1.3 though the association was not found to be statistically significant. They also observed that denture use was not an independent risk factor for alveolar ridge carcinomas.[21] In a Swedish epidemiological study,[22] the authors found that relative risk for oral cancer was 5.97 for painful denture and 3.15 for ill-fitting denture in males while it was 1.60 and 2.15 for females, respectively. This study did not separate addicts from nonaddicts.
Another study[14] reported that patients with prolonged use of dentures (>8 years) experienced a lower risk of tongue cancer. It may be because well-fitted denture may not cause mucosal trauma and such patients are more likely to be on regular follow-up by a health-care personnel.
On the contrary, a Chinese retrospective study[9] looked at the role of oral hygiene, dental condition, diet, and nutrition in 404 oral cancer patients. They found that actually it was oral hygiene (i.e., number of brushings/day) which was strongly associated with risk of oral cancer. They also found that there was no association of oral cancer with denture use, broken, filled, or decayed teeth. However, they suggested that patient wearing metal denture were associated with oral cancer with OR = 5.5 in males. However, the numbers of metal denture users were too less (12/808), so this OR is not actually representative of the cohort. A study[14] conducted at Canada and Brazil showed that when matched analysis without adjustment for confounding factors as done, the denture use with associated mucosal trauma had OR = 2.3 (95% CI = 1.2–4.6) for developing into cancer. When adjusted for factors such as tobacco, alcohol, and dental-related factors (broken tooth, decayed teeth, filled teeth), this association was not found to be significant. Several studies have linked teeth status with oral cancer risk.[23,24,25] In these studies, tooth loss was the most important dental factor in relation with oral cancer risk. However, they did not find denture use as a significant risk factor in causation of oral cancer [Figure 3]. The forest plots of the OR for the available studies on the dentures and the ill-fitting dentures in causing oral cancer are depicted in Figures Figures44 and and5.5. It can be concluded from the available studies that trauma associated with ill-fitting dentures has a higher OR of resulting in oral cancer however same cannot be said for well fitted denture.
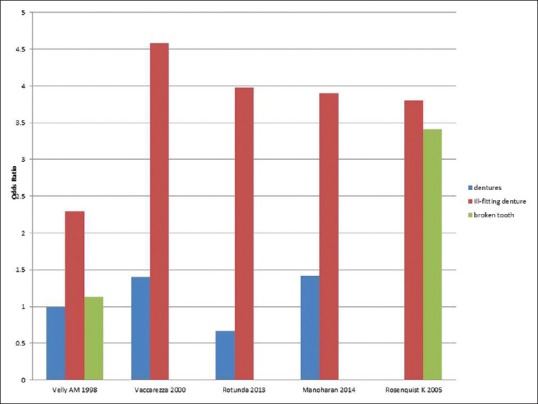
| Figure 3:Studies comparing odds ratio of denture, ill-fitting denture and broken tooth as risk factors for oral cancer
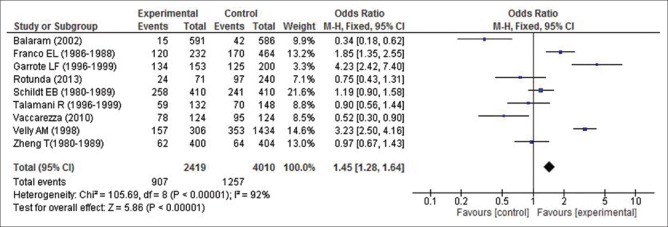
| Figure 4Forest plot for the use of denture as risk factor for oral cancer
| Figure 5Forest plot for the use of ill-fitting denture as risk factor for oral cancer
Broken/sharp Teeth and Oral Cancer
Chronic mucosal insult may also result from sharp or broken teeth. Many a times, during examination of oral cancer patient, we come across a sharp tooth at corresponding location on the alveolar arch. However, over review of literature, we could not find any study which has separately looked at association between sharp tooth and oral cancer. There have been studies establishing relationship between defective teeth and oral cancer. A Swedish[17] study has established an association between defective teeth (more than five defective teeth) and oral cancer risk with OR = 3.1; (95% CI = 1.2–8.2) even though it mentions the number of defective teeth, it does not specify the criteria to determine defective teeth. While few other studies[7,22] suggested that broken teeth was not associated with oral cancer. However, in these studies, addicts were not separated from nonaddicts. In another study,[14] broken teeth were associated with oral cancer to the OR = 1.43 but when adjusted for confounders its OR dropped to 1.13. Very few studies have specifically studied sharp teeth or broken teeth in association with oral cancer, they are generally considered as one of the dental factors. Available evidence does not appear to be significant enough to support broken/sharp teeth to be a risk factor in causing oral cancer.
Association of Duration of Denture Use and Oral Cancer
Carcinogens such as tobacco and alcohol have been shown to have a relationship between their dose, duration of use and probability of developing cancer. Similarly, a few studies have reported whether duration of denture use can be a crucial factor in carcinogenesis. A retrospective[14] Canadian study classified duration of denture use into long-term use (>8 years) and short-term use (<8 xss=removed xss=removed href="https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5398106/#ref25" rid="ref25" class=" bibr popnode tag_hotlink tag_tooltip" id="__tag_603278346" role="button" aria-expanded="false" aria-haspopup="true" xss=removed>25] in which they classified long denture wearer as >10 years, did not find any increased risk with long duration of denture wear. A meta-analysis[8] showed that there was no link between the duration of denture use and cancer development in which duration was classified as long-term (>5 years) and short-term (<5 xss=removed xss=removed xss=removed xss=removed>
Importance of Gender in Nonaddicts
In an Australian retrospective[13] study, it has been shown that in oral cancer patients among nonsmokers and nontobacco chewers around 61% were females and approximately 30% of nonsmokers and nontobacco chewers had some kind of dental abnormality in proximity to the tumor. They have not mentioned how many of those having dental abnormalities were female. In a Portuguese[26] study evaluating oral cancer patients, they classified patients depending upon addiction to alcohol, tobacco, and denture use. Of the entire cohort, 26% were females who were nonaddicts (to both tobacco and alcohol) and used dentures compared to only 11% males who were nonaddicts and denture users. Another explanation for this finding could be that more number of male patients may be addicted to tobacco and alcohol. Several studies[16,27,28] have shown that patients not addicted to tobacco and alcohol were more likely to be females. However, whether the cancer was associated with dental or denture related irritation has not been mentioned in these studies. Thus, from the above studies, it may be considered that among nonaddicts denture-associated cancers are seen more often in females.
Factors Contributing to Denture Related Carcinogenesis
Denture-related sores may be colonized by candida.[29] Colonization of denture-based materials by candida may induce inflammation of the mucosa. This may be associated with epithelial dysplasia[30] and leukoplakia formation. These are recognized oral premalignant lesions with higher potential for developing into cancer as compared to other leukoplakia.[31] A Japanese retrospective study[32] reported that human papillomavirus (HPV) may be present in the oral cavity, especially in those of denture wearers. They suggested that dentures may be a reservoir of HPV from where HPV-associated diseases, such as oral cancer and other oral lesions, may develop. Thus, the use of dentures may be associated with co-existing candida and HPV infection and these may contribute to developing oral cancer.
Dentures and Oral Potentially Malignant Disorder
There are several studies establishing association of chronic trauma with oral cancer but its association with oral potentially malignant disorder (OPMD) has been scarcely evaluated. We believe that ideally chronic trauma should result in potentially malignant lesion before evolving into carcinoma. Such an association has not been adequately studied in the literature. A retrospective study showed that though a significant association between oral cancer and chronic mucosal trauma (P = 0.000) exists, no such association was present between OPMD and mucosal trauma.[33]
Nodal Staging and Cancer Associated With Dental Trauma
A retrospective study[14] on oral carcinoma patients found a lower mean nodal staging in patients with primaries adjacent to teeth and dental appliances. Due to these appliances, patients may develop associated symptoms such as pain, bleeding, or functional problems and may present to the physician earlier. Such patients may also tend to observe their oral cavity more often. However, no other studies have discussed about the nodal status of the oral cancer associated with chronic trauma.
Dental Implants and Its Relation to Oral Cancer
Nowadays, osteocutaneous grafts and flaps are being used for reconstruction after ablative surgeries for oral cancer. Along with these, osseointegrated implants are being used for dental replacement. Although dental implants have been used, a lot over the past few decades, the recent literature[34,35,36] has had some reports of squamous cell carcinoma occurring in close association with dental implants. Although the direct carcinogenic role of dental implants has never been established, several carcinogenicity theories have been proposed. These include release of corrosion products, metallic ion release, and migration of malignant cells through the sulcus around the implant.[34,35] In a systematic review,[36] 75% of dental implant associated oral cancer had a history of previous cancer. It is often recommended that when patients at risk for oral cancer (due to addiction to tobacco or previous oral cancer) present with failure/loosening of dental implants, then they should be thoroughly evaluated to rule out the presence of malignancy associated with dental implants. It may be postulated that fixed dentures unlike removable denture over implants are in continuous contact with oral mucosa. Hence, any ill-fitting fixed denture in contact with altered mucosa (which has undergone field cancerization due to previous habits) may increase the risk of developing cancer manifold due to repeated trauma. At present, there is no definitive evidence that dental implants could be a direct etiologic or contributory agent for oral cancer formation.
Association With Denture Material
There were very few studies discussing specifically about material of denture used and its role in causing irritation of mucosa and subsequent cancer formation. There have been many reports[37,38,39,40] suggesting that residual monomer in the denture base causes mucosal irritation and sensitization of tissues. Many studies have found that chemicals leached out from acrylic resin can cause irritation of oral tissue, inflammation, or even an allergic reaction. However, there is no evidence of such resins having inherent carcinogenic potential.
Association With Tumor Morphology, Outcome, and Prognosis
We could not find any study describing the morphology of tumors associated with chronic trauma. Recurrence rate, outcome, and prognosis of such tumors have also not been studied separately.
As mentioned earlier, most of the available literature includes only retrospective case–control and descriptive studies. Such studies have limitations such as recall bias, selection bias, nonblinding, and over or under matching. In spite of all these limitations, case–control studies have given us a clue in demonstrating the role played by various factors associated with chronic mucosal trauma in the etiology of oral cancer.
Conclusion
Thus, from this review, we can conclude that chronic mucosal irritation resulting from ill-fitting dentures may be considered a risk factor for subsequent development of oral cancer. Such trauma related cancers may be seen more often over the lateral border of tongue and also over the alveolus. In patients without any addictions, such cancers occur more often in females. No association has been proven between the duration of denture use and cancer formation. These cancers may present with an early nodal disease, but their prognosis and outcomes have not been studied separately till now. No definitive relation has been seen between broken/sharp tooth, dental implants, nature of denture material and oral cancer formation. No relationship has been shown between OPMD and chronic mucosal trauma.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray, F.GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11 [Internet]. Lyon, France: International Agency for Research on Cancer; 2013. Available from: http://globocan.iarc.fr. [Last accessed on 2016 Nov 20].
- Pednekar MS, Gupta PC, Yeole BB, Hébert JR. Association of tobacco habits, including bidi smoking, with overall and site-specific cancer incidence: Results from the Mumbai cohort study. Cancer Causes Control 2011;22:859-68.
- Radoï L, Luce D. A review of risk factors for oral cavity cancer: The importance of a standardized case definition. Community Dent Oral Epidemiol 2013;41:97-109, e78-91.
- Guha N, Warnakulasuriya S, Vlaanderen J, Straif K. Betel quid chewing and the risk of oral and oropharyngeal cancers: A meta-analysis with implications for cancer control. Int J Cancer 2014;135:1433-43.
- Franco EL, Kowalski LP, Oliveira BV, Curado MP, Pereira RN, Silva ME, et al. Risk factors for oral cancer in Brazil: A case-control study. Int J Cancer 1989;43:992-1000.
- Zheng TZ, Boyle P, Hu HF, Duan J, Jian PJ, Ma DQ, et al. Dentition, oral hygiene, and risk of oral cancer: A case-control study in Beijing, people's republic of China. Cancer Causes Control 1990;1:235-41.
- Marshall JR, Graham S, Haughey BP, Shedd D, O'Shea R, Brasure J, et al. Smoking, alcohol, dentition and diet in the epidemiology of oral cancer. Eur J Cancer B Oral Oncol 1992;28B: 9-15.
- Manoharan S, Nagaraja V, Eslick GD. Ill-fitting dentures and oral cancer: A meta-analysis. Oral Oncol 2014;50:1058-61.
- Sato T. A study on effect of mechanical irritation in development and progression of tongue cancer. Kokubyo Gakkai Zasshi 1995;62:532-50.
- Kawanishi S, Hiraku Y, Pinlaor S, Ma N. Oxidative and nitrative DNA damage in animals and patients with inflammatory diseases in relation to inflammation-related carcinogenesis. Biol Chem 2006;387:365-72.
- Kundu JK, Surh YJ. Inflammation: Gearing the journey to cancer. Mutat Res 2008;659:15-30.
- Keibel A, Singh V, Sharma MC. Inflammation, microenvironment, and the immune system in cancer progression. Curr Pharm Des 2009;15:1949-55.
- Perry BJ, Zammit AP, Lewandowski AW, Bashford JJ, Dragovic AS, Perry EJ, et al. Sites of origin of oral cavity cancer in nonsmokers vs. smokers: Possible evidence of dental trauma carcinogenesis and its importance compared with human papillomavirus. JAMA Otolaryngol Head Neck Surg 2015;141:5-11.
- Velly AM, Franco EL, Schlecht N, Pintos J, Kowalski LP, Oliveira BV, et al. Relationship between dental factors and risk of upper aerodigestive tract cancer. Oral Oncol 1998;34:284-91.
- Lockhart PB, Norris CM Jr., Pulliam C. Dental factors in the genesis of squamous cell carcinoma of the oral cavity. Oral Oncol 1998;34:133-9.
- ;Kruse AL, Bredell M, Grätz KW. Oral squamous cell carcinoma in non-smoking and non-drinking patients. Head Neck Oncol 2010;2:24.
- Rosenquist K. Risk factors in oral and oropharyngeal squamous cell carcinoma: A population-based case-control study in Southern Sweden. Swed Dent J Suppl 2005;179:1-66.
- Rotundo LD, Toporcov TN, Biazevic GH, de Carvalho MB, Kowalski LP, Antunes JL. Are recurrent denture-related sores associated with the risk of oral cancer? A case control study. Rev Bras Epidemiol 2013;16:705-15.
- Vaccarezza GF, Antunes JL, Michaluart-Júnior P. Recurrent sores by ill-fitting dentures and intra-oral squamous cell carcinoma in smokers. J Public Health Dent 2010;70:52-7.
- Thumfart W, Weidenbecher M, Waller G, Pesch HG. Chronic mechanical trauma in the aetiology of oro-pharyngeal carcinoma. J Maxillofac Surg 1978;6:217-21.
- Campbell BH, Mark DH, Soneson EA, Freije JE, Schultz CJ. The role of dental prostheses in alveolar ridge squamous carcinomas. Arch Otolaryngol Head Neck Surg 1997;123:1112-5.
- Young TB, Ford CN, Brandenburg JH. An epidemiologic study of oral cancer in a statewide network. Am J Otolaryngol 1986;7:200-8.
- Bundgaard T, Wildt J, Frydenberg M, Elbrønd O, Nielsen JE. Case-control study of squamous cell cancer of the oral cavity in Denmark. Cancer Causes Control 1995;6:57-67.
- Schildt EB, Eriksson M, Hardell L, Magnuson A. Oral infections and dental factors in relation to oral cancer: A Swedish case – Control study. Eur J Cancer Prev 1998;7:201-6.
- Talamini R, Vaccarella S, Barbone F, Tavani A, La Vecchia C, Herrero R, et al. Oral hygiene, dentition, sexual habits and risk of oral cancer. Br J Cancer 2000;83:1238-42.
- Alburqueque R, Lépez-Lépez J, Marí-Roig A, Jané-Salas E, Chimenos-Küstner E, Santos JR. Relationship between squamous cell carcinoma of the anterior two thirds of the tongue and removable denture use: A pioneer study in a Portuguese population. Braz Dent J 2011;22:410-4.
- Wiseman SM, Swede H, Stoler DL, Anderson GR, Rigual NR, Hicks WL Jr., et al. Squamous cell carcinoma of the head and neck in nonsmokers and nondrinkers: An analysis of clinicopathologic characteristics and treatment outcomes. Ann Surg Oncol 2003;10:551-7.
- Dahlstrom KR, Little JA, Zafereo ME, Lung M, Wei Q, Sturgis EM. Squamous cell carcinoma of the head and neck in never smoker-never drinkers: A descriptive epidemiologic study. Head Neck 2008;30:75-84.
- Jainkittivong A, Aneksuk V, Langlais RP. Oral mucosal conditions in elderly dental patients. Oral Dis 2002;8:218-23.
- Zomorodian K, Haghighi NN, Rajaee N, Pakshir K, Tarazooie B, Vojdani M, et al. Assessment of Candida species colonization and denture-related stomatitis in complete denture wearers. Med Mycol 2011;49:208-11.
- Hooper SJ, Wilson MJ, Crean SJ. Exploring the link between microorganisms and oral cancer: A systematic review of the literature. Head Neck 2009;31:1228-39.
- Nishimura Y, Maeda H, Hattori M, Azumaya F, Muramatsu I, Kameyama Y, et al. Human papillomavirus infection in the oral cavity of denture wearers. Nihon Hotetsu Shika Gakkai Zasshi 2004;48:713-22.
- Piemonte ED, Lazos JP, Brunotto M. Relationship between chronic trauma of the oral mucosa, oral potentially malignant disorders and oral cancer. J Oral Pathol Med 2010;39:513-7.
- Schache A, Thavaraj S, Kalavrezos N. Osseointegrated implants: A potential route of entry for squamous cell carcinoma of the mandible. Br J Oral Maxillofac Surg 2008;46:397-9.
- Abu El-Naaj I, Trost O, Tagger-Green N, Trouilloud P, Robe N, Malka G, et al. Peri-implantitis or squamous cell carcinoma? Rev Stomatol Chir Maxillofac 2007;108:458-60.
- Bhatavadekar NB. Squamous cell carcinoma in association with dental implants: An assessment of previously hypothesized carcinogenic mechanisms and a case report. J Oral Implantol 2012;38:792-8.
- Basker RM, Sturdee DW, Davenport JC. Patients with burning mouths. A clinical investigation of causative factors, including the climacteric and diabetes. Br Dent J 1978;145:9-16.
- Kallus T. Evaluation of the toxicity of denture base polymers after subcutaneous implantation in guinea pigs. J Prosthet Dent 1984;52:126-34.
- Ali A, Bates JF, Reynolds AJ, Walker DM. The burning mouth sensation related to the wearing of acrylic dentures: An investigation. Br Dent J 1986;161:444-7.
- Giunta JL, Grauer I, Zablotsky N. Allergic contact stomatitis caused by acrylic resin. J Prosthet Dent 1979;42:188-90.
| Figure 1:Proposed hypothesis of mechanism of carcinogenesis following chronic mucosal trauma
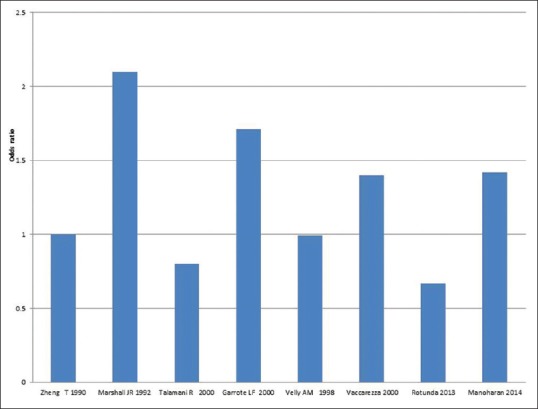
| Figure 2:Studies showing odds ratio of denture as a risk factor for oral cancer (adjusted for confounders)
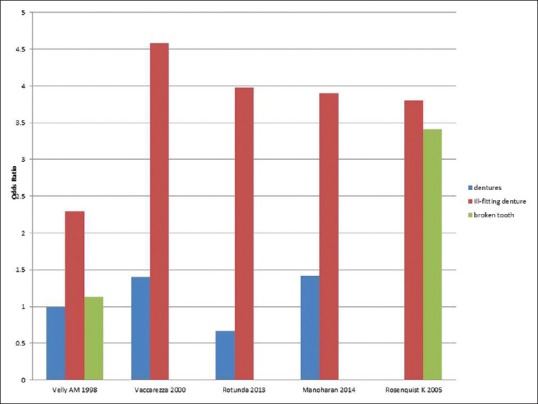
| Figure 3:Studies comparing odds ratio of denture, ill-fitting denture and broken tooth as risk factors for oral cancer
References
- Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray, F.GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11 [Internet]. Lyon, France: International Agency for Research on Cancer; 2013. Available from: http://globocan.iarc.fr. [Last accessed on 2016 Nov 20].
- Pednekar MS, Gupta PC, Yeole BB, Hébert JR. Association of tobacco habits, including bidi smoking, with overall and site-specific cancer incidence: Results from the Mumbai cohort study. Cancer Causes Control 2011;22:859-68.
- Radoï L, Luce D. A review of risk factors for oral cavity cancer: The importance of a standardized case definition. Community Dent Oral Epidemiol 2013;41:97-109, e78-91.
- Guha N, Warnakulasuriya S, Vlaanderen J, Straif K. Betel quid chewing and the risk of oral and oropharyngeal cancers: A meta-analysis with implications for cancer control. Int J Cancer 2014;135:1433-43.
- Franco EL, Kowalski LP, Oliveira BV, Curado MP, Pereira RN, Silva ME, et al. Risk factors for oral cancer in Brazil: A case-control study. Int J Cancer 1989;43:992-1000.
- Zheng TZ, Boyle P, Hu HF, Duan J, Jian PJ, Ma DQ, et al. Dentition, oral hygiene, and risk of oral cancer: A case-control study in Beijing, people's republic of China. Cancer Causes Control 1990;1:235-41.
- Marshall JR, Graham S, Haughey BP, Shedd D, O'Shea R, Brasure J, et al. Smoking, alcohol, dentition and diet in the epidemiology of oral cancer. Eur J Cancer B Oral Oncol 1992;28B: 9-15.
- Manoharan S, Nagaraja V, Eslick GD. Ill-fitting dentures and oral cancer: A meta-analysis. Oral Oncol 2014;50:1058-61.
- Sato T. A study on effect of mechanical irritation in development and progression of tongue cancer. Kokubyo Gakkai Zasshi 1995;62:532-50.
- Kawanishi S, Hiraku Y, Pinlaor S, Ma N. Oxidative and nitrative DNA damage in animals and patients with inflammatory diseases in relation to inflammation-related carcinogenesis. Biol Chem 2006;387:365-72.
- Kundu JK, Surh YJ. Inflammation: Gearing the journey to cancer. Mutat Res 2008;659:15-30.
- Keibel A, Singh V, Sharma MC. Inflammation, microenvironment, and the immune system in cancer progression. Curr Pharm Des 2009;15:1949-55.
- Perry BJ, Zammit AP, Lewandowski AW, Bashford JJ, Dragovic AS, Perry EJ, et al. Sites of origin of oral cavity cancer in nonsmokers vs. smokers: Possible evidence of dental trauma carcinogenesis and its importance compared with human papillomavirus. JAMA Otolaryngol Head Neck Surg 2015;141:5-11.
- Velly AM, Franco EL, Schlecht N, Pintos J, Kowalski LP, Oliveira BV, et al. Relationship between dental factors and risk of upper aerodigestive tract cancer. Oral Oncol 1998;34:284-91.
- Lockhart PB, Norris CM Jr., Pulliam C. Dental factors in the genesis of squamous cell carcinoma of the oral cavity. Oral Oncol 1998;34:133-9.
- ;Kruse AL, Bredell M, Grätz KW. Oral squamous cell carcinoma in non-smoking and non-drinking patients. Head Neck Oncol 2010;2:24.
- Rosenquist K. Risk factors in oral and oropharyngeal squamous cell carcinoma: A population-based case-control study in Southern Sweden. Swed Dent J Suppl 2005;179:1-66.
- Rotundo LD, Toporcov TN, Biazevic GH, de Carvalho MB, Kowalski LP, Antunes JL. Are recurrent denture-related sores associated with the risk of oral cancer? A case control study. Rev Bras Epidemiol 2013;16:705-15.
- Vaccarezza GF, Antunes JL, Michaluart-Júnior P. Recurrent sores by ill-fitting dentures and intra-oral squamous cell carcinoma in smokers. J Public Health Dent 2010;70:52-7.
- Thumfart W, Weidenbecher M, Waller G, Pesch HG. Chronic mechanical trauma in the aetiology of oro-pharyngeal carcinoma. J Maxillofac Surg 1978;6:217-21.
- Campbell BH, Mark DH, Soneson EA, Freije JE, Schultz CJ. The role of dental prostheses in alveolar ridge squamous carcinomas. Arch Otolaryngol Head Neck Surg 1997;123:1112-5.
- Young TB, Ford CN, Brandenburg JH. An epidemiologic study of oral cancer in a statewide network. Am J Otolaryngol 1986;7:200-8.
- Bundgaard T, Wildt J, Frydenberg M, Elbrønd O, Nielsen JE. Case-control study of squamous cell cancer of the oral cavity in Denmark. Cancer Causes Control 1995;6:57-67.
- Schildt EB, Eriksson M, Hardell L, Magnuson A. Oral infections and dental factors in relation to oral cancer: A Swedish case – Control study. Eur J Cancer Prev 1998;7:201-6.
- Talamini R, Vaccarella S, Barbone F, Tavani A, La Vecchia C, Herrero R, et al. Oral hygiene, dentition, sexual habits and risk of oral cancer. Br J Cancer 2000;83:1238-42.
- Alburqueque R, Lépez-Lépez J, Marí-Roig A, Jané-Salas E, Chimenos-Küstner E, Santos JR. Relationship between squamous cell carcinoma of the anterior two thirds of the tongue and removable denture use: A pioneer study in a Portuguese population. Braz Dent J 2011;22:410-4.
- Wiseman SM, Swede H, Stoler DL, Anderson GR, Rigual NR, Hicks WL Jr., et al. Squamous cell carcinoma of the head and neck in nonsmokers and nondrinkers: An analysis of clinicopathologic characteristics and treatment outcomes. Ann Surg Oncol 2003;10:551-7.
- Dahlstrom KR, Little JA, Zafereo ME, Lung M, Wei Q, Sturgis EM. Squamous cell carcinoma of the head and neck in never smoker-never drinkers: A descriptive epidemiologic study. Head Neck 2008;30:75-84.
- Jainkittivong A, Aneksuk V, Langlais RP. Oral mucosal conditions in elderly dental patients. Oral Dis 2002;8:218-23.
- Zomorodian K, Haghighi NN, Rajaee N, Pakshir K, Tarazooie B, Vojdani M, et al. Assessment of Candida species colonization and denture-related stomatitis in complete denture wearers. Med Mycol 2011;49:208-11.
- Hooper SJ, Wilson MJ, Crean SJ. Exploring the link between microorganisms and oral cancer: A systematic review of the literature. Head Neck 2009;31:1228-39.
- Nishimura Y, Maeda H, Hattori M, Azumaya F, Muramatsu I, Kameyama Y, et al. Human papillomavirus infection in the oral cavity of denture wearers. Nihon Hotetsu Shika Gakkai Zasshi 2004;48:713-22.
- Piemonte ED, Lazos JP, Brunotto M. Relationship between chronic trauma of the oral mucosa, oral potentially malignant disorders and oral cancer. J Oral Pathol Med 2010;39:513-7.
- Schache A, Thavaraj S, Kalavrezos N. Osseointegrated implants: A potential route of entry for squamous cell carcinoma of the mandible. Br J Oral Maxillofac Surg 2008;46:397-9.
- Abu El-Naaj I, Trost O, Tagger-Green N, Trouilloud P, Robe N, Malka G, et al. Peri-implantitis or squamous cell carcinoma? Rev Stomatol Chir Maxillofac 2007;108:458-60.
- Bhatavadekar NB. Squamous cell carcinoma in association with dental implants: An assessment of previously hypothesized carcinogenic mechanisms and a case report. J Oral Implantol 2012;38:792-8.
- Basker RM, Sturdee DW, Davenport JC. Patients with burning mouths. A clinical investigation of causative factors, including the climacteric and diabetes. Br Dent J 1978;145:9-16.
- Kallus T. Evaluation of the toxicity of denture base polymers after subcutaneous implantation in guinea pigs. J Prosthet Dent 1984;52:126-34.
- Ali A, Bates JF, Reynolds AJ, Walker DM. The burning mouth sensation related to the wearing of acrylic dentures: An investigation. Br Dent J 1986;161:444-7.
- Giunta JL, Grauer I, Zablotsky N. Allergic contact stomatitis caused by acrylic resin. J Prosthet Dent 1979;42:188-90.


 PDF
PDF  Views
Views  Share
Share

