Triple Trouble: Disseminated Penicilliosis in a Cancer patient with COVID-19
CC BY 4.0 · Indian J Med Paediatr Oncol 2023; 44(04): 445-448
DOI: DOI: 10.1055/s-0042-1759505
Abstract
Penicilliosis is a fungal infection caused by the fungus Penicillium marneffei or Talaromyces marneffei. Penicillosis is commonly seen in immunocompromised patients such as in HIV(AIDS). Herein, we present a case of penicilliosis in an oral cavity cancer patient who was admitted for the management of SARS-CoV-2 infection at our hospital. A 50-year-old male patient operated on for squamous cell carcinoma of the oral cavity who completed his adjuvant chemoradiation 2 months ago, presented to our hospital with dry cough for more than 3 weeks. His nasopharyngeal swab was positive for the severe acute respiratory distress syndrome (SARS-CoV-2). During his hospital stay for SARS-CoV-2 infection, he was diagnosed with disseminated penicilliosis. The patient was treated with intravenous antifungals caspofungin and voriconazole. However, he succumbed to disseminated fungal sepsis. This case highlights the need to consider penicilliosis as a possible opportunistic pathogen, especially in immunocompromised patients such as cancer.
Declaration of Patient Consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
Publication History
Article published online:
29 March 2023
© 2023. The Author(s). This is an open access article published by Thieme under the terms of the Creative Commons Attribution License, permitting unrestricted use, distribution, and reproduction so long as the original work is properly cited. (https://creativecommons.org/licenses/by/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Penicilliosis is a fungal infection caused by the fungus Penicillium marneffei or Talaromyces marneffei. Penicillosis is commonly seen in immunocompromised patients such as in HIV(AIDS). Herein, we present a case of penicilliosis in an oral cavity cancer patient who was admitted for the management of SARS-CoV-2 infection at our hospital. A 50-year-old male patient operated on for squamous cell carcinoma of the oral cavity who completed his adjuvant chemoradiation 2 months ago, presented to our hospital with dry cough for more than 3 weeks. His nasopharyngeal swab was positive for the severe acute respiratory distress syndrome (SARS-CoV-2). During his hospital stay for SARS-CoV-2 infection, he was diagnosed with disseminated penicilliosis. The patient was treated with intravenous antifungals caspofungin and voriconazole. However, he succumbed to disseminated fungal sepsis. This case highlights the need to consider penicilliosis as a possible opportunistic pathogen, especially in immunocompromised patients such as cancer.
Keywords
penicilliosis - cancer - oral cavity - SARS-CoV-2 - COVID-19
Introduction
Penicilliosis infection is commonly seen in immunocompromised patients such as acquired immunodeficiency syndrome (AIDS), cancer and persons with autoimmune diseases.[1] [2] [3] Disseminated penicilliosis is transmitted in humans from the inhalation of spores from the environment.[4] There are published reports in the literature showing penicilliosis infections in lung cancer patients.[5] In 1959, G. Segretain, a mycologist from the Pastur institute at Paris was the first person to discover penicilliosis. Symptomatology varies as per the system involved. The diagnosis of penicilliosis is suspected or done through examination of either cytology or biopsy samples.[6] Herein, we report the first case of disseminated penicilliosis infection in a cancer patient with concomitant SARS-CoV-2 infection.
Case
A 50-year male patient, premorbidly healthy, was diagnosed with carcinoma of buccal mucosa (non-keratinizing squamous cell carcinoma) T4-N3b-M0. He received two cycles of neo-adjuvant chemotherapy (paclitaxel + carboplatin + cetuximab) followed by right buccal mucosa composite resection + left neck dissection followed by pectoralis major myocutaneous flap. Post-surgery, he received concurrent radiation (60Gy/30# of RT over 43 days) along with weekly cisplatin. Two months after completion of concurrent chemoradiation, he presented with a 3-week history of dry cough. Nasopharyngeal swab was positive for SARS-CoV-2 infection using standard real-time polymerase chain reaction (RT-PCR test). He was hospitalized with a diagnosis of severe COVID-19 as per ordinal scale.[7] On admission, the patient was tachypneic, and hypoxic with bilateral crepitations. X-ray chest ([Fig. 1A]) showed bilateral infiltrates. In view of severe COVID-19, and in anticipation of a difficult airway considering a recent history of major facial surgery, an elective tracheostomy was performed on the day of hospital admission. After tracheostomy, he was supported with invasive mechanical ventilation with volume control mode (FiO2 50%). Meanwhile, he was treated with intravenous dexamethasone (6 mg once a day as per the RECOVERY trial) [8] for severe COVID-19, along with broad-spectrum antibiotic (meropenem) and prophylactic enoxaparin. Nondirected broncho-alveolar lavage (ND-BAL) was sent for bacterial culture that showed a sensitive strain of Pseudomonas aeruginosa. Over the next 96 hours, he improved with respect to defervescence, oxygen requirement, and lung infiltrates. On day 10, he was on minimal oxygen support (2 L/min) without any tachypnea. Repeat ND-BAL cultures were negative for any bacterial growth. However, on day 12, we noticed an increase in respiratory rate, with a rise in C-reactive protein (CRP) and radiological evidence of increased lung infiltrates ([Fig. 1B]). In view of normal procalcitonin, high CRP, and repeatedly negative blood and tracheal cultures, we suspected an impending recurrent cytokine storm due to SARS-CoV-2 infection. On account of better lung penetration of methylprednisolone in comparison to dexamethasone[9] and based on evidence for utility of bevacizumab[10] at the time of patient management, he was treated with a single dose of intravenous bevacizumab 400 mg, intravenous methylprednisolone 20 mg 12 hourly, along with broad-spectrum antibiotics (colistin+ ceftazidime-avibactam + aztreonam). However, his lung infiltrates continued to worsen. In view of rising CRP with worsening infiltrates, recent steroid use, and recent use of broad-spectrum antibiotics, the possibility of an opportunistic fungal infection was considered. His blood sugars and neutrophil counts were normal. An ND-BAL fungal culture was repeated. After 24 hours on Sabouraud dextrose agar (SDA) at 25°C; it showed a filamentous grayish–white growth in 24 hours. The growth later became yellowish green in the center surrounded by white periphery and had radial folds. On Lacto phenol Cotton Blue Mount (LPCB), penicillial morphology was seen. Hyaline short hyphae that were septate and branched bearing chains of elliptical or lemon shaped phialoconidia were seen. Dimorphism showing yeast to mycelial phase conversion could not be demonstrated. Hence, it was probably diagnosed as Penicillium non-marneffi spp. Voriconazole plus caspofungin has been shown to work well for patients with penicilliosis non-marneffi infection.[11] Hence, he was started on injection caspofungin pre-emptively pending further identification. Computerized tomogram (CT) of the chest and abdomen showed multiple nodular lesions in bilateral lung fields with cavitations, ground glass opacities, along with well-defined hypodense lesions in segment VII, VIII and multiple satellite foci consistent with a fungal etiology ([Fig. 1C]). An aspiration of liver abscess was not performed in view of poor general condition of the patient. There were no signs of active COVID-19 disease on CT scan. Patient was continued on antibacterials and injection caspofungin. Over the next 96 hours, ND-BAL culture growth was reported as Penicillium species (non-marneffei) ([Fig. 2]). ND-BAL galactomannan levels were positive (Index 3.601), though serum galactomannan levels were negative. The day wise trend of CBC, CRP, and procalcitonin is provided in [Table 1]. After 1 week, voriconazole was added as he continued to worsen with respect to respiratory parameters, rising CRP, worsening infiltrates, and negative bacterial cultures. Subsequently, he had worsening hypoxia necessitating mechanical ventilation. Despite maintaining therapeutic voriconazole levels, he progressed to septic shock. On day 27 of hospital admission, he succumbed to disseminated penicilliosis.

| Figure 1:(A) X-ray chest showing a few nodular opacities in both lung fields, maximum in right lower zone suggestive of infective etiology. (B) X-ray chest showing increase in nodular opacities as compared to a prior X ray, features suggestive of worsening of pulmonary infection. (C) Multinodular lesions in bilateral lung fields with cavitations (red arrow) and surrounding ground glass opacities (green arrow) [in top two panels and left middle panel] suggestive of infective etiology more likely to be fungal. Multiple hypodense (blue arrow) hepatic lesions in segments VII and VIII, suggestive of multiple abscesses. [right middle panel and both lower panels].
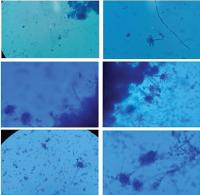
| Figure 2:Lactophenol cotton blue stain mount from the growth of the Penicillium spp showing conidiophores having secondary branches called metulae. On metulae are arranged flask-shaped phialides bearing conidia. The entire structure is forming the characteristic "penicillus "or "brush" appearance.
|
Day of COVID-19 positivity |
Hb g/dL |
TLC * 109 (per L) |
ANC * 109 (per L) |
ALC * 109 (per L) |
Platelets * 109 (per L) |
CRP(mg%) |
Procalcitonin (ng/mL) |
|---|---|---|---|---|---|---|---|
|
1 |
– |
– |
– |
– |
– |
– |
– |
|
2 |
7.3 |
9.59 |
8.29 |
0.44 |
175 |
10.31 |
– |
|
4 |
8.5 |
10.26 |
9.62 |
0.33 |
172 |
11.5 |
0.08 |
|
5 |
7.7 |
13.33 |
12.56 |
0.28 |
211 |
4.4 |
– |
|
6 |
7.4 |
11.99 |
11.02 |
0.34 |
178 |
5.8 |
0.13 |
|
11 |
13.6 |
5.84 |
3.92 |
1.08 |
181 |
5.4 |
0.17 |
|
14 |
12.9 |
12.46 |
10.93 |
0.66 |
257 |
1.0 |
0.14 |
|
18 |
13.0 |
7.61 |
4.63 |
2.03 |
348 |
0.3 |
0.05 |
|
19 |
8.6 |
8.13 |
7.22 |
0.39 |
139 |
– |
0.06 |
|
20 |
– |
– |
– |
– |
– |
4.6 |
– |
|
21 |
8.1 |
6.71 |
5.86 |
0.261 |
144 |
8.99 |
0.13 |
|
22 |
8.2 |
5.68 |
4.97 |
0.255 |
161 |
11.8 |
0.17 |
|
25 |
8.4 |
4.86 |
4.41 |
0.184 |
194 |
13.98 |
0.17 |
|
26 |
8.4 |
8.82 |
7.81 |
0.308 |
206 |
16.68 |
0.58 |
|
27 |
7.4 |
6.82 |
6.04 |
0.293 |
178 |
23.4 |
0.33 |
|
28 |
6.9 |
6.27 |
5.83 |
0.206 |
140 |
24.7 |
0.66 |
|
29 |
8.5 |
15.96 |
12.51 |
2.82 |
265 |
29.32 |
13.55 |
References
- Talaromycosis (formerly Penicilliosis) Fungal Diseases CDC. Accessed October 30, 2021, at: www.cdc.gov
- Sun J, Sun W, Tang Y. et al. Clinical characteristics and risk factors for poor prognosis among HIV patients with Talaromyces marneffei bloodstream infection. BMC Infect Dis 2021; 21 (01) 514
- Zheng J, Gui X, Cao Q. et al. A clinical study of acquired immunodeficiency syndrome associated Penicillium marneffei infection from a non-endemic area in China. PLoS One 2015; 10 (06) e0130376
- Stone A, Park BJ. Penicillium marneffei Infection: Knowledge, Gaps, and Future Directions. Curr Fungal Infect Rep 2011; 5 (04) 193
- Ching-López R, Rodríguez Pavón S. Talaromycosis in a lung cancer patient: a rare case. Cureus 2020; 12 (09) e10615
- Gorai S, Saha M, Madhab V, Mitra S. Talaromycosis (penicilliosis): a rare, opportunistic systemic fungal infection. Indian J Dermatol 2019; 64 (04) 331-333
- Goldman JD, Lye DCB, Hui DS. et al; GS-US-540-5773 Investigators. Remdesivir for 5 or 10 days in patients with severe covid-19. N Engl J Med 2020; 383 (19) 1827-1837 DOI: 10.1056/NEJMoa2015301.
- Horby P, Lim WS, Emberson JR. et al; RECOVERY Collaborative Group. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med 2021; 384 (08) 693-704 DOI: 10.1056/NEJMoa2021436.
- Ranjbar K, Moghadami M, Mirahmadizadeh A. et al. Methylprednisolone or dexamethasone, which one is superior corticosteroid in the treatment of hospitalized COVID-19 patients: a triple-blinded randomized controlled trial. BMC Infect Dis 2021; 21 (01) 337 DOI: 10.1186/s12879-021-06045-3.
- Pang J, Xu F, Aondio G. et al. Efficacy and tolerability of bevacizumab in patients with severe Covid-19. Nat Commun 2021; 12 (01) 814
- Ramírez I, Hidrón A, Cardona R. Successful treatment of pulmonary invasive fungal infection by Penicillium non -marneffei in lymphoblastic lymphoma: case report and literature review. Clin Case Rep 2018; 6 (06) 1153-1157
- Vanittanakom N, Cooper Jr CR, Fisher MC, Sirisanthana T. Penicillium marneffei infection and recent advances in the epidemiology and molecular biology aspects. Clin Microbiol Rev 2006; 19 (01) 95-110
- Yadav S, Gupta R, Anuradha S, Makkar AM. A rare case of disseminated penicilliosis – first of its kind from North India. Indian J Pathol Microbiol 2019; Jan-Mar; 62 (01) 156-158
- Huang YT, Hung CC, Liao CH, Sun HY, Chang SC, Chen YC. Detection of circulating galactomannan in serum samples for diagnosis of Penicillium marneffei infection and cryptococcosis among patients infected with human immunodeficiency virus. J Clin Microbiol 2007; 45 (09) 2858-2862
- Li CS, Pan SF. Analysis and causation discussion of 185 severe acute respiratory syndrome dead cases [article in Chinese]. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue 2003; 15 (10) 582-584
- Peng J, Wang Q, Mei H. et al. Fungal co-infection in COVID-19 patients: evidence from a systematic review and meta-analysis. Aging (Albany NY) 2021; 13 (06) 7745-7757
- Singh RB, Devi KR. A comparative study on antifungal susceptibility of Penicillium marneffei ( Talaromyces marneffei) and nonmarneffei Penicillium species. J Med Soc 2018; 32: 22-26
- Supparatpinyo K, Schlamm HT. Voriconazole as therapy for systemic Penicillium marneffei infections in AIDS patients. Am J Trop Med Hyg 2007; 77 (02) 350-353
- Lin F, Qiu Y, Zeng W, Liang Y, Zhang J. Talaromyces marneffei infection in a lung cancer patient: a rare case report. BMC Infect Dis 2019; 19 (01) 336
- Yang Z, Zeng W, Qiu Y, Liu G, Zhang J. Nodular sclerosing Hodgkin lymphoma combined with disseminated Talaromyces marneffei infection: a case report. Infect Drug Resist 2021; 14: 5671-5678
- Fedorková L, Vojtech I, He LP, Ondruš D. Multiresistent opportunistic talaromycosis in a patient with ovarian cancer. Klin Onkol 2020; 33 (06) 464-466
- Narayanasamy S, Dat VQ, Thanh NT. et al. A global call for talaromycosis to be recognised as a neglected tropical disease. Lancet Glob Health 2021; 9 (11) e1618-e1622
Address for correspondence
Publication History
Article published online:
29 March 2023
© 2023. The Author(s). This is an open access article published by Thieme under the terms of the Creative Commons Attribution License, permitting unrestricted use, distribution, and reproduction so long as the original work is properly cited. (https://creativecommons.org/licenses/by/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
References
- Talaromycosis (formerly Penicilliosis) Fungal Diseases CDC. Accessed October 30, 2021, at: www.cdc.gov
- Sun J, Sun W, Tang Y. et al. Clinical characteristics and risk factors for poor prognosis among HIV patients with Talaromyces marneffei bloodstream infection. BMC Infect Dis 2021; 21 (01) 514
- Zheng J, Gui X, Cao Q. et al. A clinical study of acquired immunodeficiency syndrome associated Penicillium marneffei infection from a non-endemic area in China. PLoS One 2015; 10 (06) e0130376
- Stone A, Park BJ. Penicillium marneffei Infection: Knowledge, Gaps, and Future Directions. Curr Fungal Infect Rep 2011; 5 (04) 193
- Ching-López R, Rodríguez Pavón S. Talaromycosis in a lung cancer patient: a rare case. Cureus 2020; 12 (09) e10615
- Gorai S, Saha M, Madhab V, Mitra S. Talaromycosis (penicilliosis): a rare, opportunistic systemic fungal infection. Indian J Dermatol 2019; 64 (04) 331-333
- Goldman JD, Lye DCB, Hui DS. et al; GS-US-540-5773 Investigators. Remdesivir for 5 or 10 days in patients with severe covid-19. N Engl J Med 2020; 383 (19) 1827-1837 DOI: 10.1056/NEJMoa2015301.
- Horby P, Lim WS, Emberson JR. et al; RECOVERY Collaborative Group. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med 2021; 384 (08) 693-704 DOI: 10.1056/NEJMoa2021436.
- Ranjbar K, Moghadami M, Mirahmadizadeh A. et al. Methylprednisolone or dexamethasone, which one is superior corticosteroid in the treatment of hospitalized COVID-19 patients: a triple-blinded randomized controlled trial. BMC Infect Dis 2021; 21 (01) 337 DOI: 10.1186/s12879-021-06045-3.
- Pang J, Xu F, Aondio G. et al. Efficacy and tolerability of bevacizumab in patients with severe Covid-19. Nat Commun 2021; 12 (01) 814
- Ramírez I, Hidrón A, Cardona R. Successful treatment of pulmonary invasive fungal infection by Penicillium non -marneffei in lymphoblastic lymphoma: case report and literature review. Clin Case Rep 2018; 6 (06) 1153-1157
- Vanittanakom N, Cooper Jr CR, Fisher MC, Sirisanthana T. Penicillium marneffei infection and recent advances in the epidemiology and molecular biology aspects. Clin Microbiol Rev 2006; 19 (01) 95-110
- Yadav S, Gupta R, Anuradha S, Makkar AM. A rare case of disseminated penicilliosis – first of its kind from North India. Indian J Pathol Microbiol 2019; Jan-Mar; 62 (01) 156-158
- Huang YT, Hung CC, Liao CH, Sun HY, Chang SC, Chen YC. Detection of circulating galactomannan in serum samples for diagnosis of Penicillium marneffei infection and cryptococcosis among patients infected with human immunodeficiency virus. J Clin Microbiol 2007; 45 (09) 2858-2862
- Li CS, Pan SF. Analysis and causation discussion of 185 severe acute respiratory syndrome dead cases [article in Chinese]. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue 2003; 15 (10) 582-584
- Peng J, Wang Q, Mei H. et al. Fungal co-infection in COVID-19 patients: evidence from a systematic review and meta-analysis. Aging (Albany NY) 2021; 13 (06) 7745-7757
- Singh RB, Devi KR. A comparative study on antifungal susceptibility of Penicillium marneffei ( Talaromyces marneffei) and nonmarneffei Penicillium species. J Med Soc 2018; 32: 22-26
- Supparatpinyo K, Schlamm HT. Voriconazole as therapy for systemic Penicillium marneffei infections in AIDS patients. Am J Trop Med Hyg 2007; 77 (02) 350-353
- Lin F, Qiu Y, Zeng W, Liang Y, Zhang J. Talaromyces marneffei infection in a lung cancer patient: a rare case report. BMC Infect Dis 2019; 19 (01) 336
- Yang Z, Zeng W, Qiu Y, Liu G, Zhang J. Nodular sclerosing Hodgkin lymphoma combined with disseminated Talaromyces marneffei infection: a case report. Infect Drug Resist 2021; 14: 5671-5678
- Fedorková L, Vojtech I, He LP, Ondruš D. Multiresistent opportunistic talaromycosis in a patient with ovarian cancer. Klin Onkol 2020; 33 (06) 464-466
- Narayanasamy S, Dat VQ, Thanh NT. et al. A global call for talaromycosis to be recognised as a neglected tropical disease. Lancet Glob Health 2021; 9 (11) e1618-e1622


 PDF
PDF  Views
Views  Share
Share

