Undifferentiated Carcinoma of the Uterine Cervix with Evidence of Its Origin from Small-Cell Neuroendocrine Carcinoma
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2018; 39(04): 536-538
DOI: DOI: 10.4103/ijmpo.ijmpo_23_17
Abstract
Neuroendocrine carcinoma (NEC) of the uterine cervix is an uncommon aggressive tumor, comprises <5>Keywords
Human papillomavirus - neuroendocrine carcinoma - undifferentiated carcinoma - uterine cervixPublication History
Article published online:
17 June 2021
© 2018. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/).
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Neuroendocrine carcinoma (NEC) of the uterine cervix is an uncommon aggressive tumor, comprises <5>
Keywords
Human papillomavirus - neuroendocrine carcinoma - undifferentiated carcinoma - uterine cervixIntroduction
Neuroendocrine carcinoma (NEC) of the uterine cervix is an uncommon tumor, accounting -<5>1] [2] Undifferentiated carcinoma of the uterine cervix is extremely rare with no obvious histologic evidence of differentiation. It can be typed as undifferentiated squamous cell carcinoma or NEC by immunohistochemistry using p63 and panel of neuroendocrine markers. We report an extremely rare case of undifferentiated carcinoma of the uterine cervix, originating from SCNEC, proven by immunohistochemistry and the presence of differentiated NEC component in the proximity.
Case Report
A premenopausal, P2 L2 female, presented with complaints of bleeding per vagina for 3 months and cervix biopsy report of moderately differentiated squamous cell carcinoma. She underwent right hemithyroidectomy for benign thyroid nodule 4 years back. There was no other past medical history. Contrast-enhanced computerized tomography outside showed a large mass lesion involving the entire length of the cervix with the right parametrial extension. The exophytic mass measured 5.7 cm × 5.5 cm. There was no pelvic or para-aortic lymphadenopathy. She was staged cT2bcN0 and was given concurrent radiotherapy and platinum-based chemotherapy for 5 weeks. Posttherapy speculum examination revealed gross residual tumor in the cervix.
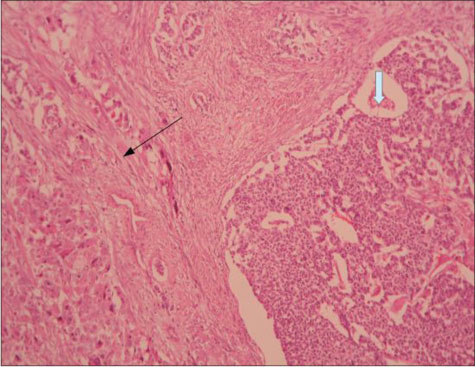
Posttherapy CT scan revealed a large residual proliferative mass in the anterior lip of the cervix, which was hyperintense on T2 and showed minimal enhancement postcontrast [Figure 1]. The mass measured 4 cm × 3.5 cm × 2.5 cm seen projecting into the vaginal cavity. There was no free fluid in the pelvis. Wertheim’s hysterectomy was performed with nodal sampling. The specimen showed an exophytic firm tumor of 3.8 cm × 3.2 cm × 3.2 cm in the anterior lip of the cervix. Rest of the uterus and ovaries were grossly normal.

| Figure 1:Posttherapy computed tomography images showing large residual tumor in the anterior lip of cervix
Histology showed a tumor with two different looking areas, merging with each other [Figure 2]. The tumor cells were small, arranged in nests and cords, with round nuclei and granular chromatin. Apoptotic bodies and increased mitosis were present [Figure 3a]. Merging with these tumor cells were large cells in islands and sheets, with moderate cytoplasm, enlarged nuclei, and prominent eosinophilic nucleoli [Figure 3b]. Bizarre nuclei, multinucleation, intranuclear cytoplasmic pseudoinclusions, lymphovascular invasion, and perineural invasion were seen. The smaller and larger tumor cells were immunoreactive to synaptophysin [Figure 4a] and CD56 [Figure 4b] with proliferation index of 14%. Chromogranin, neuron-specific enolase (NSE), p16, and p63 were negative. With the above histomorphology and immunohistochemistry findings, a diagnosis of undifferentiated carcinoma of the uterine cervix with transition from high-grade SCNEC was made. There were no ascertainable therapy associated changes. She was on adjuvant chemotherapy with cisplatin.
| Figure.2:Undifferentiated carcinoma showing islands of large cells (black arrow) merging with small-cell neuroendocrine carcinoma in nests (block arrow) (H and E, ×40)
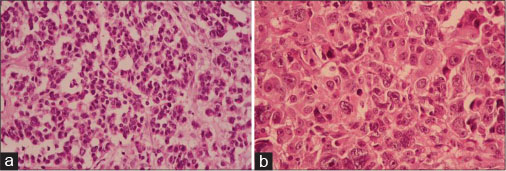
| Figure.3:(a) Neuroendocrine carcinoma component showing small cells in nests and cords with granular chromatin. (b) Undifferentiated carcinoma areas with large nuclei and prominent nucleoli (H and E, ×100)
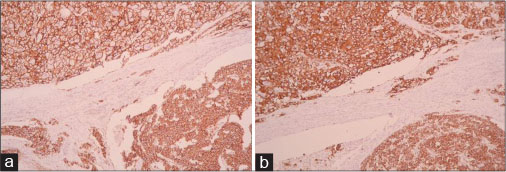
| Figure.4:Undifferentiated carcinoma component in the upper left and neuroendocrine carcinoma component in the lower right showing positivity to synaptophysin (a) and CD56 (b) (×40)
Discussion
Neuroendocrine tumors of the cervix is defined by a consensus workshop in 1997 as carcinoid, atypical carcinoid, SCNEC, and large-cell NEC.[1] NECs are uncommon, aggressive tumors of the cervix, with no defined precursor lesions and may coexist with glandular or squamous carcinoma. They constitute <5 href="https://www.thieme-connect.com/products/ejournals/html/10.4103/ijmpo.ijmpo_23_17#JR_2" xss=removed>2] NEC is associated with high-risk human papillomavirus (HPV-18).[3] High-grade NEC is highly aggressive, regardless of the morphological subtype or stage of the disease, with poorer survival in higher stage disease.[4]
Undifferentiated carcinoma of the uterine cervix is extremely rare, composed of sheets of cells with no histologic evidence of squamous or glandular differentiation.[5] Immunohistochemistry with p63 or neuroendocrine markers helps in delineating the tumor type as squamous cell carcinoma or NEC. p16 and detection of HPV by in situ hybridization help in differentiating metastatic from primary tumors.[5]
Clinically, the tumor presents as like other cervical carcinomas as vaginal bleeding (as seen in the patient) and/or mass.[4] [5] The patient rarely may present with carcinoid symptoms due to metastatic disease. Histology of SCNEC is characterized by sheets of small cells with hyperchromatic nuclei, high nucleus-to-cytoplasmic ratio, and scant cytoplasm. Necrosis, abundant mitosis, apoptotic activity, and nuclear molding are characteristics. NEC of large cell type (LCNEC) has organoid or trabecular growth pattern with cells showing abundant cytoplasm and large nuclei with prominent nucleoli.[2] [4]
Diagnosis of NEC is supported by staining of the tumor cells for neuroendocrine markers such as synaptophysin, chromogranin, NSE, and CD56. Synaptophysin and CD56 seem to be sensitive than chromogranin.[2] [4] The tumor cells mostly show thyroid transcription factor-1 positivity, hence does not help in differentiating from SCNEC of the lung. They are variably negative to p63, useful in differentiating from small-cell nonkeratinizing squamous cell carcinoma.[4]
As SCNEC metastasize in the early stages of the disease, pelvic control by radical hysterectomy alone does not appear to be beneficial and needs adjuvant chemotherapy to control hematogenous spread, and thereby to improve the survival.[6] The role of radiotherapy in control of local recurrence is debated.[6] [7] Previous studies have reported dismal prognosis despite various treatment modalities. Lee et al. have found that patients who received neoadjuvant chemotherapy (NACT) showed poorer prognosis than those who did not receive NACT.[6] This case did not have any therapy-associated changes in histology, though there was a slight reduction in size by 2 cm in imaging. Federation of Gynecology and Obstetrics stage is an independent prognostic factor for NEC.[6] The other probable prognostic factors discussed by previous studies include tumor size, presence and number of lymph node metastasis, stage, pure small-cell histology, parametrial involvement, deep stromal invasion, and smoking.[8] [9] [10]
To conclude, NECs are highly aggressive uncommon tumors, usually presenting at advanced stage of the disease and poorer survival even with multimodal therapy. Undifferentiated carcinoma of the cervix is extremely rare, with evidence of origin from SCNEC (with positivity for neuroendocrine markers as seen in our case), or from squamous or adenocarcinoma. Undifferentiated carcinoma is expected to behave aggressively as it gets dedifferentiated from a differentiated malignancy. Considering the extreme rarity of undifferentiated carcinoma and NEC of the uterine cervix, further case studies and follow-up of these might help in ascertaining the behavior of this tumor and to plan appropriate therapy.
Conflict of Interest
There are no conflicts of interest.
References
- Gardner GJ, Reidy-Lagunes D, Gehrig PA. Neuroendocrine tumors of the gynecologic tract: A Society of Gynecologic Oncology (SGO) clinical document. Gynecol Oncol 2011; 122: 190-8
- Nucci MR, Lee KR, Crum CP. Tumors of the female genital tract, part E cervix. In: Fletcher CD. editor Diagnostic Histopathology of Tumors. 4th ed. 1. Philadelphia: Elsevier Saunders; 2013: 829-30
- Stoler MH, Mills SE, Gersell DJ, Walker AN. Small-cell neuroendocrine carcinoma of the cervix. A human papillomavirus type 18-associated cancer. Am J Surg Pathol 1991; 15: 28-32
- Colgan TJ, Kim I, Hirschowitz L, McCluggage WG. Neuroendocrine tumours. In: Kurman RJ, Carcangiu ML, Herrington CS, Young RH. editors WHO Classification of Tumours of Female Reproductive Organs. 4th ed. Lyon: IARC; 2014: 196-8
- Colgan TJ, Kim KR, Hirschowitz L, McCluggage WG. Other epithelial tumours. In: Kurman RJ, Carcangiu ML, Herrington CS, Young RH. editors WHO Classification of Tumours of Female Reproductive Organs. 4th ed. Lyon: IARC; 2014: 194-6
- Lee JM, Lee KB, Nam JH, Ryu SY, Bae DS, Park JT. et al. Prognostic factors in FIGO stage IB-IIA small cell neuroendocrine carcinoma of the uterine cervix treated surgically: Results of a multi-center retrospective Korean study. Ann Oncol 2008; 19: 321-6
- Bifulco G, Mandato VD, Giampaolino P, Piccoli R, Insabato L, De Rosa N. et al. Small cell neuroendocrine cervical carcinoma with 1-year follow-up: Case report and review. Anticancer Res 2009; 29: 477-84
- Wang KL, Yang YC, Wang TY, Chen JR, Chen TC, Chen HS. et al. Neuroendocrine carcinoma of the uterine cervix: A clinicopathologic retrospective study of 31 cases with prognostic implications. J Chemother 2006; 18: 209-16
- Viswanathan AN, Deavers MT, Jhingran A, Ramirez PT, Levenback C, Eifel PJ. et al. Small cell neuroendocrine carcinoma of the cervix: Outcome and patterns of recurrence. Gynecol Oncol 2004; 93: 27-33
- Chan JK, Loizzi V, Burger RA, Rutgers J, Monk BJ. Prognostic factors in neuroendocrine small cell cervical carcinoma: A multivariate analysis. Cancer 2003; 97: 568-74
Address for correspondence
Publication History
Article published online:
17 June 2021
© 2018. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/).
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2,
Noida-201301 UP, India

| Figure 1:Posttherapy computed tomography images showing large residual tumor in the anterior lip of cervix
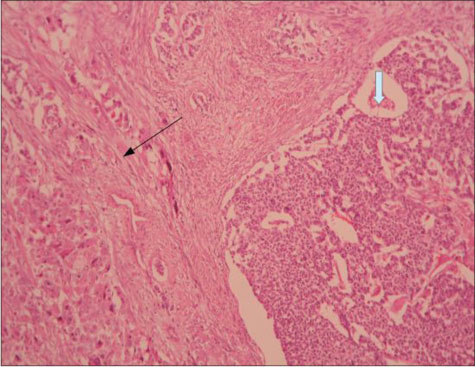
| Figure.2:Undifferentiated carcinoma showing islands of large cells (black arrow) merging with small-cell neuroendocrine carcinoma in nests (block arrow) (H and E, ×40)
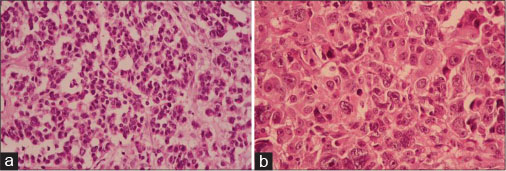
| Figure.3:(a) Neuroendocrine carcinoma component showing small cells in nests and cords with granular chromatin. (b) Undifferentiated carcinoma areas with large nuclei and prominent nucleoli (H and E, ×100)
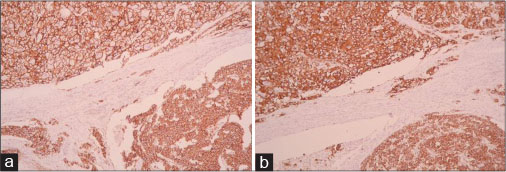
| Figure.4:Undifferentiated carcinoma component in the upper left and neuroendocrine carcinoma component in the lower right showing positivity to synaptophysin (a) and CD56 (b) (×40)
References
- Gardner GJ, Reidy-Lagunes D, Gehrig PA. Neuroendocrine tumors of the gynecologic tract: A Society of Gynecologic Oncology (SGO) clinical document. Gynecol Oncol 2011; 122: 190-8
- Nucci MR, Lee KR, Crum CP. Tumors of the female genital tract, part E cervix. In: Fletcher CD. editor Diagnostic Histopathology of Tumors. 4th ed. 1. Philadelphia: Elsevier Saunders; 2013: 829-30
- Stoler MH, Mills SE, Gersell DJ, Walker AN. Small-cell neuroendocrine carcinoma of the cervix. A human papillomavirus type 18-associated cancer. Am J Surg Pathol 1991; 15: 28-32
- Colgan TJ, Kim I, Hirschowitz L, McCluggage WG. Neuroendocrine tumours. In: Kurman RJ, Carcangiu ML, Herrington CS, Young RH. editors WHO Classification of Tumours of Female Reproductive Organs. 4th ed. Lyon: IARC; 2014: 196-8
- Colgan TJ, Kim KR, Hirschowitz L, McCluggage WG. Other epithelial tumours. In: Kurman RJ, Carcangiu ML, Herrington CS, Young RH. editors WHO Classification of Tumours of Female Reproductive Organs. 4th ed. Lyon: IARC; 2014: 194-6
- Lee JM, Lee KB, Nam JH, Ryu SY, Bae DS, Park JT. et al. Prognostic factors in FIGO stage IB-IIA small cell neuroendocrine carcinoma of the uterine cervix treated surgically: Results of a multi-center retrospective Korean study. Ann Oncol 2008; 19: 321-6
- Bifulco G, Mandato VD, Giampaolino P, Piccoli R, Insabato L, De Rosa N. et al. Small cell neuroendocrine cervical carcinoma with 1-year follow-up: Case report and review. Anticancer Res 2009; 29: 477-84
- Wang KL, Yang YC, Wang TY, Chen JR, Chen TC, Chen HS. et al. Neuroendocrine carcinoma of the uterine cervix: A clinicopathologic retrospective study of 31 cases with prognostic implications. J Chemother 2006; 18: 209-16
- Viswanathan AN, Deavers MT, Jhingran A, Ramirez PT, Levenback C, Eifel PJ. et al. Small cell neuroendocrine carcinoma of the cervix: Outcome and patterns of recurrence. Gynecol Oncol 2004; 93: 27-33
- Chan JK, Loizzi V, Burger RA, Rutgers J, Monk BJ. Prognostic factors in neuroendocrine small cell cervical carcinoma: A multivariate analysis. Cancer 2003; 97: 568-74


 PDF
PDF  Views
Views  Share
Share

