Transilluminating testicular mass
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2011; 32(01): 46-48
DOI: DOI: 10.4103/0971-5851.81891
Abstract
Testicular tumor in prepubertal age group is uncommon. Most of the testicular tumors are benign in this age group and present as painless, hard testicular mass. We present a case where a 7 year male child presented to us with painless scrotal swelling, which was cystic and transilluminating, clinically mimicking as hydrocele. On ultrasonography, the mass was solid. Orchidectomy was performed and histopathology revealed mature cystic teratoma.
Publication History
Article published online:
16 August 2021
© 2011. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Testicular tumor in prepubertal age group is uncommon. Most of the testicular tumors are benign in this age group and present as painless, hard testicular mass. We present a case where a 7 year male child presented to us with painless scrotal swelling, which was cystic and transilluminating, clinically mimicking as hydrocele. On ultrasonography, the mass was solid. Orchidectomy was performed and histopathology revealed mature cystic teratoma.
INTRODUCTION
Prepubertal testicular tumors are rare accounting for 1–2% of all pediatric tumors with incidence of 0.5–2.0 per 100,000 children.[1] The testicular tumors show a bimodal age distribution, with a large peak in young adults and a much smaller but distinct peak in the first 3 years of life.[2] They differ greatly from adult testicular tumors. While seminoma is most common in adults, teratoma is more common in pediatric age group. Majority of patients present with a testicular mass, which is typically hard and painless. We present a case where testicular teratoma presented as a completely transilluminating scrotal mass clinically mimicking as hydrocele.
CASE REPORT
A 7-year-old male child presented with complaints of painless progressive swelling in the left scrotum noticed by parents for last 1 month. The patient had an unremarkable birth history and no significant past medical history. There was no history of trauma. On physical examination, the child was well nourished with normal developmental milestones. He had a normal uncircumcised phallus and a descended right testis. The left half of scrotum was enlarged, tensely cystic in consistency, and nontender. The scrotal skin of the left side was stretched. The swelling was not compressible but transilluminated brilliantly [Figure 1]. The left testis was not palpable. There was no regional lymphadenopathy. The clinical diagnosis of hydrocele was made initially. On scrotal ultrasound, on the left side, unexpectedly there was no hydrocele; left testis was 13×23×21 mm (6.2 cc) in size and parenchyma was hypochoic as compared to right testis. Multiple tiny specks of parenchymal calcification were also noted. On color Doppler study, there was generalized hypervascularity as compared to the right side. Left epididymis was hypoechoic, hypovascular, and thickened. Right testis was homogenous in appearance and measured 22×11×10 mm (2.4 cc). The ultrasonologist reported it as suspected chronic epididymo-orchitis, and it may be tubercular. Additional investigations like complete blood count, liver function test, renal function test, chest X-ray, β-HCG, serum alfa-fetoprotein (AFP), montoux test, ELISA for tuberculosis were conducted. All investigations were within normal limit.

| Fig. 1 Left side scrotal swelling which transilluminates brilliantly
During surgery, the testis was approached through a left inguinal skin crease incision. Vas and vessel were temporarily occluded after opening the inguinal canal. The testis was delivered, which looked normal in appearance but size was larger. On incising the testis, white gelatinous material with yellowish-white flakes came out and no solid component was found [Figure 2]. Orchidectomy was performed. The histopathological finding revealed benign mature cystic teratoma testis with component of all three germ layers, confined within the left testis [Figure 3]. At 3-month followup, the child is asymptomatic.

| Fig. 2 Gelatinous material with yellowish-white flakes on incising the testis
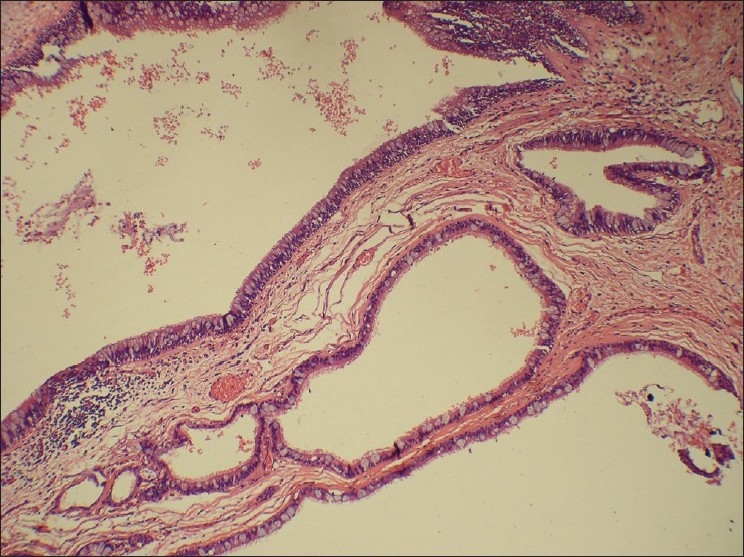
| Fig. 3 Histopathological finding revealed benign mature cystic teratoma testis with component of all three germ layers. Here mature respiratory epithelium is seen
DISCUSSION
Teratoma is a neoplasm of germ cell origin that is composed of multiple cell types derived from one or more of the three germ layers. The exact frequency of testicular tumors in pediatric population needs to be rectified. According to the prepubertal testis tumor registry of urology section of the American Academy of Pediatrics, 62% of primary testicular tumors were yolk sac tumors followed by teratoma, which accounts for 26%.[1] But, recent reviews of single-center or captive population studies have shown that benign tumors of the testis are more common in children and teratoma is the most common pathology.[3–5]
Most testicular tumors present as painless hard mass though rarely they may present with acute scrotum due to hemorrhage or torsion. More rarely, it may present with precocious puberty with gynecomastia. On physical examination, a mass that cannot be separated from the testis is assumed to be a testicular tumor until proved otherwise. Hydrocele is associated in 15–50% of testicular tumor.[2] If a hydrocele is large and firm enough to preclude palpation of the testis, an ultrasound should be obtained.[6] Preoperative evaluation of testicular tumor always includes an ultrasound and an estimation of serum AFP. Ultrasound with Doppler study is helpful in distinguishing testicular from paratesticular lesions in nearly 100% cases. It also determines whether the entire testis is replaced by tumor or if there is some normal testicular tissue that may be salvaged if the tumor is benign. Tumor markers including AFP elevated in malignant germ cell tumors and particularly in yolk sac tumors. Since, AFP may be physiologically elevated in normal infants of less than 6 months, it is less helpful for the diagnosis in this age group.[2] Testicular teratoma can be suspected in a prepubertal child with testicular mass who does not have endocrine manifestation (gonadal stromal tumor) and an elevated AFP level (yolk sac tumor), especially when ultrasound demonstrates well-circumscribed partially cystic, intratesticular lesion. However, the diagnosis of testicular tumor is confirmed at the time of surgery.
Natural history of prepubertal testicular teratoma differs significantly from testicular teratoma of adults. Testicular teratomas are almost always benign in prepubertal children, and they rarely have associated intratubular germ cell neoplasia (or carcinoma in situ) in the remainder of the normal testis compared with nearly 90% of adult cases.[2] For this reason, metastatic evaluation may be deferred until a histopatholgical diagnosis of the primary tumor is obtained. This fact also supports the use of testis-sparing surgery if any salvageable normal testicular tissue is present.[5,6] If AFP level is mildly raised or if there is any doubt in the diagnosis, then initial excision biopsy and frozen section should be done. If biopsy reveals malignant tumor or potentially malignant tumor, then radical orchidectomy is performed. Otherwise in case of benign histopathology, the testis should be preserved. If teratoma is diagnosed and child is near pubertal age, surrounding parenchyma should be examined for intratubular germ cell neoplasia, presence of which warrants radical orchidectomy; enuclation or partial orchidectomy for teratoma in pubertal boys is not recommended.[2]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.

| Fig. 1 Left side scrotal swelling which transilluminates brilliantly

| Fig. 2 Gelatinous material with yellowish-white flakes on incising the testis
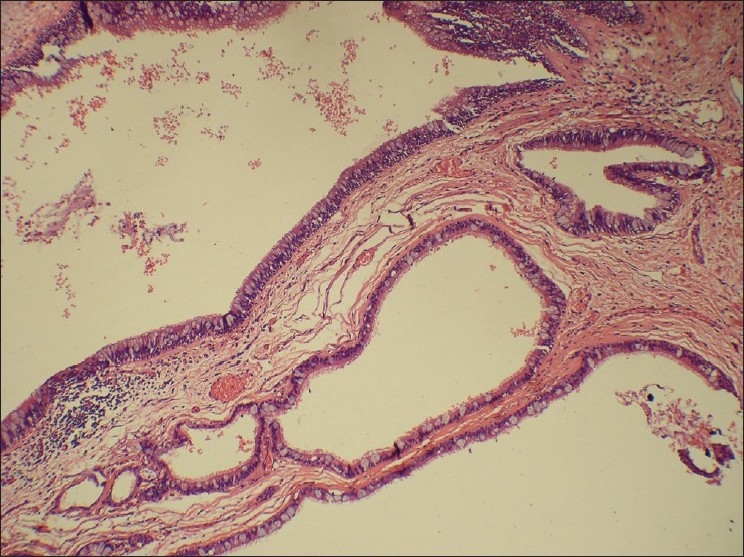
| Fig. 3 Histopathological finding revealed benign mature cystic teratoma testis with component of all three germ layers. Here mature respiratory epithelium is seen


 PDF
PDF  Views
Views  Share
Share

