A cross-sectional observation study regarding patients and their physician willingness to wait for driver mutation report in nonsmall-cell lung cancer
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2016; 37(02): 74-78
DOI: DOI: 10.4103/0971-5851.180138
Abstract
Background: Palliative chemotherapy +/− targeted therapy in accordance with mutation profile is the norm in nonsmall-cell lung cancer (NSCLC). The objective of this audit was to determine the proportion of patients and physicians, who are unwilling to wait for the mutation report and the reasons thereof. Materials and Methods: All newly diagnosed NSCLC patients, post biopsy, seen at our center between November 2014 and January 2015 were included. The relationship between patient and physician decision and objective factors was explored by Fisher's exact test. The factors considered were Eastern Cooperative Oncology Group performance status (ECOG PS), the presence of a cough, hemoptysis, fatigue, and breathlessness. The agreement between patients and physician decision was tested by contingency table. Results: Out of 168 patients, 57 were unwilling to wait for driver mutation report (33.9% confidence interval [CI] 27.2-41.4%). The most common reason provided by patients was symptomatic status (23, 40.1%). No other objective factor except PS (P = 0.00) was associated with patient's decision. In 56 patients (33.4% CI 26.6-40.7%), physicians were unwilling to wait. Among the tested factors ECOG PS (P = 0.000), breathlessness (P = 0.00) and fatigue (P = 0.00) were associated with the decision of not waiting for the report. The percentage corrected value of contingency between patients and physician decision was 78.74%. Conclusion: At present, in our setup, nearly one-third of our NSCLC patients opt for immediate chemotherapy treatment and are unwilling to wait for mutation analysis report. The major reasons for such attitude is poor symptom control and deteriorating general condition.
Keywords
Acceptance - delay - epidermal growth factor receptor mutation analysis - nonsmall-cell lung cancer - willingnessPublication History
Article published online:
12 July 2021
© 2016. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Background:
Palliative chemotherapy +/− targeted therapy in accordance with mutation profile is the norm in nonsmall-cell lung cancer (NSCLC). The objective of this audit was to determine the proportion of patients and physicians, who are unwilling to wait for the mutation report and the reasons thereof.
Materials and Methods:
All newly diagnosed NSCLC patients, post biopsy, seen at our center between November 2014 and January 2015 were included. The relationship between patient and physician decision and objective factors was explored by Fisher's exact test. The factors considered were Eastern Cooperative Oncology Group performance status (ECOG PS), the presence of a cough, hemoptysis, fatigue, and breathlessness. The agreement between patients and physician decision was tested by contingency table.
Results:
Out of 168 patients, 57 were unwilling to wait for driver mutation report (33.9% confidence interval [CI] 27.2-41.4%). The most common reason provided by patients was symptomatic status (23, 40.1%). No other objective factor except PS (P = 0.00) was associated with patient's decision. In 56 patients (33.4% CI 26.6-40.7%), physicians were unwilling to wait. Among the tested factors ECOG PS (P = 0.000), breathlessness (P = 0.00) and fatigue (P = 0.00) were associated with the decision of not waiting for the report. The percentage corrected value of contingency between patients and physician decision was 78.74%.
Conclusion:
At present, in our setup, nearly one-third of our NSCLC patients opt for immediate chemotherapy treatment and are unwilling to wait for mutation analysis report. The major reasons for such attitude is poor symptom control and deteriorating general condition.
INTRODUCTION
Palliative chemotherapy in lung cancer has undergone major changes in the last decade.[1] Initially, palliative chemotherapy in lung cancer was decided on the basis of histology. Whether it was nonsmall-cell lung cancer (NSCLC) or small-cell lung cancer was sufficient to decide treatment. However, currently, not merely histological subclassifications (squamous cell carcinoma or adenocarcinoma) but also the mutation analysis determines the treatment. The discovery of driver mutations and development of small molecules targeting them has changed the way we treat NSCLC today.[1,2,3] Lung cancer treatment guidelines now recommend that at least epidermal growth factor receptor (EGFR) tyrosine kinase domain mutation analysis and ALK rearrangement must be done before starting treatment. Treatment recommendations are based on the results of these analysis.[4,5]
At our center, we follow these international guidelines. However, frequently we encounter a situation where either the patient or the treating physician is unwilling to wait for the mutation analysis report. In an attempt to understand the reasons why either the patient or the physicians are unwilling to wait for the report we did an audit of all consecutive NSCLC patients who came to medical oncology lung cancer outpatient department. The objective of this audit was to determine the proportion of patients refusing to wait for the report and the reasons for the same.
MATERIALS AND METHODS
Patient selection
We maintain a lung cancer chemotherapy database of all newly registered NSCLC patients. All patients with lung referred for palliative chemotherapy are counseled about their diagnosis, stage, prognosis and treatment options. Then they are asked to wait till the availability of mutation analysis report (if applicable) and treatment is then started according to institutional local guidelines.
In this database from November 2014, we routinely started entering the patients and physicians willingness for waiting for treatment, till the availability of mutation report. In addition, we would also enter the reason for not waiting for the report.
The reasons for not waiting were coded as below:
- Patients reason for not waiting:
- Logistics: Patient does not have social support to stay in Mumbai
- Symptomatic: Patient feels his/her symptoms are not adequately controlled by symptomatic medications and hence wants immediate chemotherapy
- Poor general condition: Patient feels his/her general condition is poor, it may deteriorate further if he/she waits
- Not willing for rebiopsy: Initially, biopsy has inadequate tissue but the patient is not willing for rebiopsy hence does not want to wait.
- Physicians reason for not waiting:
- Eastern Cooperative Oncology Group performance status (ECOG PS) 2-4: Physician feels that patients PS is poor, it may deteriorate further if he/she waits
- Symptomatic: Physician feels that patients symptoms are not adequately controlled by symptomatic medications and hence recommends immediate chemotherapy
- Emergency: Patient has Superior vena cava obstruction (SVCO) or spinal cord compression or other oncologic emergency that warrants immediate treatment
- Others: Patient has already been started on chemotherapy outside our hospital.
All NSCLC cancer patients seen in lung cancer Medical Oncology Outpatient Department between November 2014 and January 2015 were selected for this analysis subjected to following criteria.
Selection criteria
- NSCLC patients referred for palliative chemotherapy
- Biopsy available
- Mutation analysis requested.
From the database, patients meeting these requirements were extracted. In addition, data regarding ECOG PS, stage, pathology, patient's decision regarding willingness to wait for mutation report and the reason for it and physicians willingness to wait for mutation report and the reason for it were extracted. Electronic medical records and case file records were sought when any of the above data were found missing.
Statistical analysis
R Studio version 3.1.2 (R: A Language and Environment for Statistical Computing, R Core Team, Vienna, Austria) was used for analysis. Descriptive statistics was performed. Categorical variables have been reported in the form of frequencies. The relationship between patients willingness to wait and factors was explored by Fisher's exact test for count data. The factors considered were ECOG PS (0-2 vs. 3-4), the presence of cough (yes, no), the presence of hemoptysis (yes, no), the presence of fatigue (yes, no), and the presence of breathlessness (yes, no). Similarly was the relationship between physicians willingness to wait and factors was explored. Binary logistic regression analysis was performed for multivariate analysis to identify independent factors influencing patients and physicians decision.
The agreement analysis between patients decision and physician decision was tested by software package library (VCD). It was kept in mind that the doctor's decision to some extent may be influenced by patient's decision and vice versa. As we were not sure about the assumption of decision independence between doctors and patients, we avoided the application of agreement analysis in this situation. Hence, the percentage correct value was estimated from the contingency table in this study. Decision tree used for contingency analysis is depicted in Figure 1.
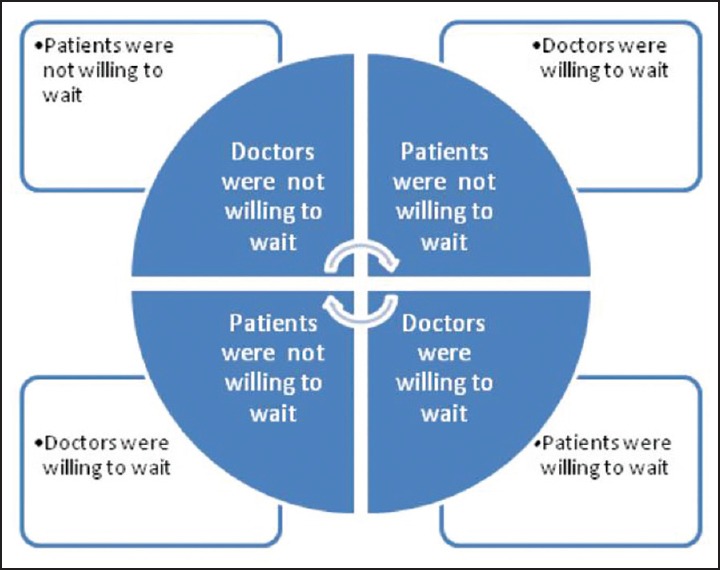
| Fig. 1 Decision tree used for contingency analysis
RESULTS
Patient details
One hundred and sixty-eight patients were selected. One hundred and fifty-six (92.8%) patient had Stage IV disease whereas 11 patients (7.2%) had Stage III disease (not a candidate for radical treatment). The histology was adenocarcinoma in 155 patients (92.2%). The ECOG PS was 0, 1, 2, 3, and 4 in 3 patients (1.8%), 85 patients (50.6%), 42 patients (25.0%), 36 patients (21.4%), and 2 patients (1.2%), respectively. Cough, hemoptysis, pain, breathlessness and fatigue were reported by 124 patients (73.8%), 22 patients (13.9%), 91 patients (54.2%), 106 patients (63.1%), and 88 patients (52.4%), respectively.
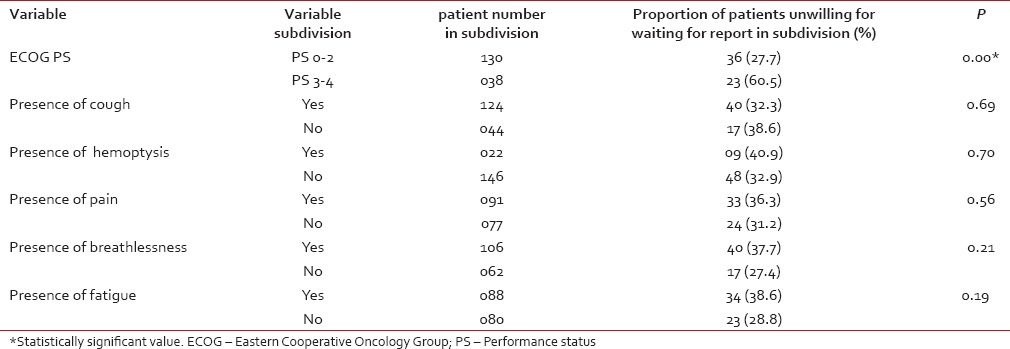
Patients decision and reasons
Out of 168 patients, 111 patients (66.1%) were willing to wait for biopsy report while 57 (33.9%) were not. The reasons provided by patients for not waiting were symptomatic status in 23 patients (40.1%), a poor general condition in 19 patients (33.3%), the logistic issue in 14 (24.6%) and others in 01 (2.0%). Factors affecting patients decision are shown in Table 1. Only ECOG PS was associated with patients unwillingness to wait.
Table 1
Different factors affecting patients decision making
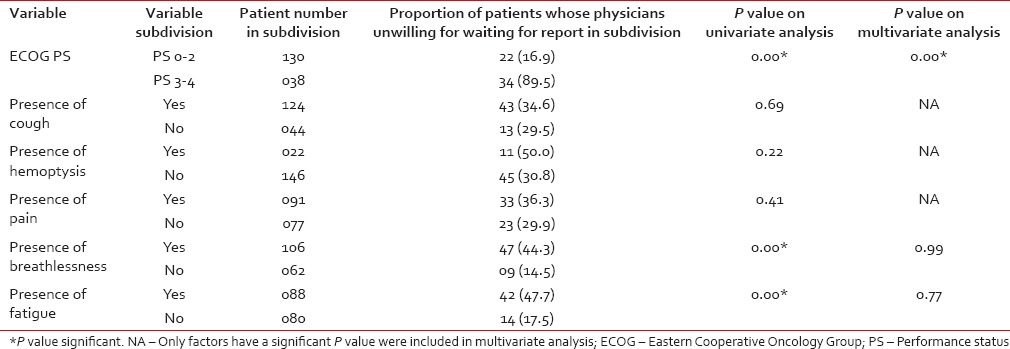
 Physicians decisions and reasons
Physicians decisions and reasonsOut of 168 patients, in 112 patients (66.6%) physicians were willing to wait for biopsy report while in 56 patients (33.4%) they were not. The reasons for not waiting were symptomatic status in 28 patients (50.0%), poor PS in 22 patients (39.4%), emergency in 03 patients (SVCO-2, spinal cord compression-1), and others in 3 patients (05.3%). The reasons provided in others were old age in 2 patients and in 1 patient the chemotherapy had already been started. Factors affecting physicians decision are shown in Table 2. Though ECOG PS (P = 0.00), breathlessness (P = 0.00) and fatigue (P = 0.00) were associated with physicians decision of not waiting for the report on univariate analysis only poor PS (0.00) was an independent factor influencing the decision identified on multivariate analysis.
Table 2
Different factors affecting physicians decision making
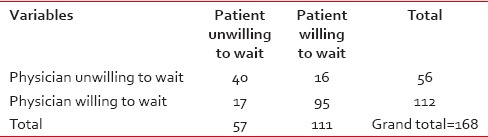
 Concordance between physician and patient's decision
Concordance between physician and patient's decisionThe 2 × 2 table of the decision of patients and physician is shown in Table 3. The estimated percentage corrected value of contingency between patients and physician decision was 78.74%.
Table 3
The concordance between patient and physician on willingness to wait for report
DISCUSSION
The era of personalized medicine comes with a challenge. A major challenge faced by physicians is to convince patients to perform investigations which make it possible to plan personalized treatment and in addition to patiently wait for such a report is available. Literature from the Western world clearly shows that patients are willing to do this. A study from North America by Cuffe et al. highlighted that 99% of patients in adjuvant setting and 97.4% in palliative setting respectively, are willing to undergo pharmacogenomic testing that would identify the cohort of patients who would benefit from therapy.[6] Though the majority of patients wanted to be a part of the decision-making process, 20% of patients lack the basic knowledge to do so.[6] A similar attitude toward pharmacogenetic testing was noted in the UK public by Finegold et al.[7] However, in our study, surprisingly one-third of patients even after being counseled regarding the benefit of EGFR mutation testing were not willing to wait for the report. EGFR and ALK testing is a part of routine protocol and hence, we recommend tissue biopsy in all NSCLC patients. Hence, the sample for mutation testing is acquired at the time of diagnostic confirmation itself. The report at our center is provided within 2 weeks which is at par with the international standards. Inspite of this, we face opposition from many patients to wait for the report and hence we wanted to identify the factors responsible. Even the large studies done in Western countries have identified a small proportion of patients who are resistant to such testing but they fail to identify the reason behind this resistance.[7]
Our analysis determines that poor symptom control (40.1%) was the major reason for patient resistance to wait. Poor symptom control is associated with high distress and deterioration in performance status. The reason behind this may be that a dedicated palliative care clinic for lung cancer is not available for these patients. The other common reason which was provided by patients was a poor general condition. This seems to corroborate with poor performance status. The important question here is the reason for poor PS. If the reason were uncontrolled comorbidity or disease related immediately correctable (pleural effusion) cause then may be a repeat interview after corrective treatment may help the patient to change their decision. However, in case of poor PS because of other causes, waiting for report is unjustifiable. This is reflected in the fact that poor PS patients and those with breathlessness were recommended the immediate start of therapy without awaiting the molecular report. The third common reason given by patients was logistics which was mainly because of lack of social support for staying in the city. This is a problem peculiar to our tertiary care referral center that draws patients from all parts of the country.
We have planned corrective steps toward improving patients compliance with the recommendation to wait for EGFR report. First is repeated counselling of patients who are unwilling to wait for the report. We are conducting group discussion meetings between patients, relatives, doctors and social workers so that in a more elaborate way, with the aid of audio-visual presentations the importance of mutation testing can be stressed. We thought that this step is necessary, as the Western population is nearly 100% literate but nearly 20% of Indian population is illiterate and hence the basic knowledge of decisions need to be explained in more simplified manner with visual aids.[8] Further efforts will be made for getting a dedicated palliative care expert for better management of symptoms preferably located near the medical oncology lung clinic. Facility would be provided for patients to access their reports online itself with a telephonic alert so that these patients staying far away can revisit our center or a center nearby for starting appropriate treatment. Finally, we are planning to expedite our lab efforts so that reports can be available within 1 week and develop liquid biopsy based molecular tests. We plan to repeat our analysis after 1 year of implementation of these measures to quantify the effect of our measures.
CONCLUSION
At present, in our setup, nearly one-third of our NSCLC patients opt for immediate chemotherapy treatment and are unwilling to wait for mutation analysis report. The major reasons for such attitude are poor symptom control and deteriorating general condition.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
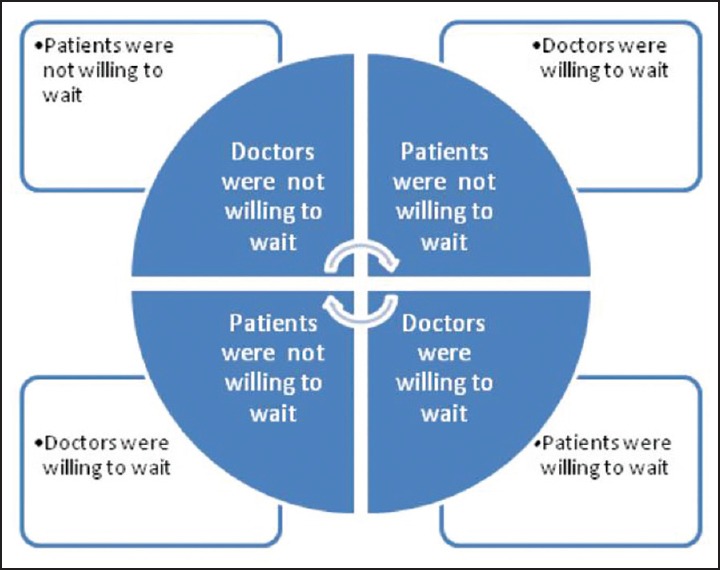
| Fig. 1 Decision tree used for contingency analysis


 PDF
PDF  Views
Views  Share
Share

