Biallelic Mismatch Repair Deficiency in Children and Adolescents: A Review of Published and Unpublished Data from India—Need for an Indian Consortium
CC BY 4.0 · Indian J Med Paediatr Oncol 2025; 46(03): 288-296
DOI: DOI: 10.1055/s-0044-1790202
Abstract
Introduction Biallelic mismatch repair deficiency or constitutional mismatch repair deficiency (CMMRD) is a rare and aggressive pediatric cancer predisposition syndrome that occurs as a result of homozygous (biallelic) pathogenic variants in mismatch repair genes. The primary malignancies that occur in CMMRD are mainly hematological and brain malignancies. Most published data are from the western populations and the Middle East. Data from India are limited to case reports. We performed an analysis to determine the prevalence of CMMRD in the Indian population.
Materials and Methods All children aged less than 18 years with a diagnosis of CMMRD from various centers in India were included. CMMRD confirmed using genetic, molecular, and clinical criteria by an international consensus was included in the analysis. Literature search and data submitted by individual centers were reviewed.
Results The analysis revealed that 22 children had genetically confirmed CMMRD. The median age of the cohort was 6.5 years, with a male predominance (male:female, 2:1). The classical phenotype of café-au-lait macules was observed in 72.7 % of subjects. The most common pathological variant was found in the PMS2 gene, which accounted for 77.3 % of children. Hematological malignancy (T cell acute lymphoblastic leukemia) was the most common primary malignancy in our study that occurred at a median age of 5 years (interquartile range 4–6 years) followed by brain tumors. The age at initial presentation for CMMRD with mutations in MSH2, MSH6, and PMS2 was 5.4, 4, and 7.5 years, respectively.
Conclusion The diagnosis of CMMRD requires a high index of suspicion for the early diagnosis, management, surveillance, counseling, and testing of family members. The awareness about CMMRD in clinicians is important so that diagnosis is made early, and a second malignancy is detected and treated early. The need for an Indian consortium to determine the actual burden of the disease, genetic characteristics, and course of illness in our country has been emphasized.
Keywords
CMMRD - India - childhood and adolescence - genetic testingPatients' Consent
The written consent of caregivers for publication has been obtained.
Supplementary MaterialPublication History
Article published online:
27 September 2024
© 2024. The Author(s). This is an open access article published by Thieme under the terms of the Creative Commons Attribution License, permitting unrestricted use, distribution, and reproduction so long as the original work is properly cited. (https://creativecommons.org/licenses/by/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
- Vitamin D Deficiency in Children with Psychiatric Illness in a Tertiary Care Hospital in North IndiaNidhi Chauhan, Journal of Neurosciences in Rural Practice, 2019
- Vitamin D Deficiency in Children with Psychiatric Illness in a Tertiary Care Hospital in North IndiaNidhi Chauhan, Journal of Neurosciences in Rural Practice, 2019
- Role of video capsule endoscopy in patients with constitutional mismatch repair deficiency (CMMRD) syndrome: report from the International CMMRD ConsortiumY. Shimamura, EIO, 2018
- Role of video capsule endoscopy in patients with constitutional mismatch repair deficiency (CMMRD) syndrome: report from the International CMMRD ConsortiumY. Shimamura, Zentralblatt für Chirurgie - Zeitschrift für Allgemeine, Viszeral-, Thorax- und Gefäßchirurgie, 2018
- Wilms Tumor in India: A Systematic ReviewShyam Srinivasan, South Asian Journal of Cancer
- Qatar´s Youth Is Putting On Weight: The Increase In Obesity Between 2003 And 2009<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- Preference of Human Biological Samples for Exposure Assessment of Elemental Pollution and Health Implication<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- Adolescents in Arab countries: Health statistics and social context<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- The Citizen Amendment Act of 2019 and its lack of impact on Shvetambara Jains in Mumbai : cautious debates on religious freedom and minority rights in a gated c...<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- Mental health issues among migrant workers in the Gulf Cooperation Council countries: Literature review and case illustrations.<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
Abstract
Introduction Biallelic mismatch repair deficiency or constitutional mismatch repair deficiency (CMMRD) is a rare and aggressive pediatric cancer predisposition syndrome that occurs as a result of homozygous (biallelic) pathogenic variants in mismatch repair genes. The primary malignancies that occur in CMMRD are mainly hematological and brain malignancies. Most published data are from the western populations and the Middle East. Data from India are limited to case reports. We performed an analysis to determine the prevalence of CMMRD in the Indian population.
Materials and Methods All children aged less than 18 years with a diagnosis of CMMRD from various centers in India were included. CMMRD confirmed using genetic, molecular, and clinical criteria by an international consensus was included in the analysis. Literature search and data submitted by individual centers were reviewed.
Results The analysis revealed that 22 children had genetically confirmed CMMRD. The median age of the cohort was 6.5 years, with a male predominance (male:female, 2:1). The classical phenotype of café-au-lait macules was observed in 72.7 %-of subjects. The most common pathological variant was found in the PMS2 gene, which accounted for 77.3 %-of children. Hematological malignancy (T cell acute lymphoblastic leukemia) was the most common primary malignancy in our study that occurred at a median age of 5 years (interquartile range 4–6 years) followed by brain tumors. The age at initial presentation for CMMRD with mutations in MSH2, MSH6, and PMS2 was 5.4, 4, and 7.5 years, respectively.
Conclusion The diagnosis of CMMRD requires a high index of suspicion for the early diagnosis, management, surveillance, counseling, and testing of family members. The awareness about CMMRD in clinicians is important so that diagnosis is made early, and a second malignancy is detected and treated early. The need for an Indian consortium to determine the actual burden of the disease, genetic characteristics, and course of illness in our country has been emphasized.
Keywords
CMMRD - India - childhood and adolescence - genetic testingIntroduction
Biallelic mismatch repair deficiency (BMMRD) or constitutional mismatch repair deficiency (CMMRD) is a rare childhood cancer predisposition syndrome with an autosomal recessive inheritance.[1] While Lynch syndrome (LS) is associated with heterozygous (monoallelic) germline pathogenic variant in one of the mismatch repair (MMR) genes, CMMRD occurs because of homozygous (biallelic) pathogenic variant in these genes.[2] Primary malignancies that occur in LS are usually of colorectal and endometrial origin. In addition to hematological and central nervous system (CNS) malignancies, colorectal malignancies are well-known and frequent in CMMRD.[3]
Most of the published data are from the western population, as well as from the Middle East. In 2024, the findings of the study with a large cohort of more than 200 patients with CMMRD, led by the International Replication Repair Deficiency Consortium (IRRDC), was published by Ercan et al.[1] Data from India were limited to case reports. We performed a literature search to determine the prevalence of CMMRD in the Indian population.
Materials and Methods
An online literature search was done to obtain published data on pediatric CMMRD cases from India. Various centers across India were contacted for data on unpublished and confirmed CMMRD cases. Only pathogenic variant-proven CMMRD cases in children from India were included in this study.
Study Design
Retrospective study: Sample size – 22 children with CMMRD.
Primary and Secondary Outcome
The primary objective was to find the clinical presentation, type of cancer, and age of onset of primary and secondary malignancy and progression of the disease. The most common malignancy was hematological malignancy with a median age of 6.5 years (interquartile range [IQR] 4–9years) at presentation and the second most common malignancy was brain tumors at a median age of 11.5 years (IQR 8–15 years) with parental consanguinity a vital pointer toward diagnosis.
The secondary objective was to find the severity of illness and survival associated with each MMR gene and its pathological variant. Children with pathogenic variants in MSH2 and MSH6 tend to have an earlier onset of malignancy. PMS2 pathogenic variants were the most common and children with MSH2 or MLH1 had severe disease. The incidence of pathogenic variants in MLH1 and MSH2 were much less than the incidence of pathogenic variants of PMS2 and MSH6.
Inclusion Criteria
All children less than 18 years with a diagnosis of CMMRD from various centers in India were included. CMMRD confirmed using clinical, genetic, and molecular criteria by an international consensus was included in the analysis. Data collected from published as well as unpublished data provided by centers treating children with malignancies were considered the full study cohort. The initial literature search was executed by searching the PubMed, Cochrane Library, and Web of Science databases for studies in the English language. The search words were “CMMRD, BMMRD” restricted to “India” and then limited to “childhood” and “adolescence.”
Exclusion Criteria
Duplicate publications and cases with no confirmatory genetic study were excluded.
Data Abstraction
Two investigators reviewed all the studies that were obtained and confirmed that they fulfill the inclusion criteria. Duplicate publications were excluded from analysis. Patients who had no confirmatory diagnosis of CMMRD based on molecular studies were excluded. The studies selected for data collection are included in [Annexure 1] (available in the online version).
All subject data submitted by individual centers were also reviewed for eligibility for entry into the analysis. An overview of this study is given in [Fig. 1].
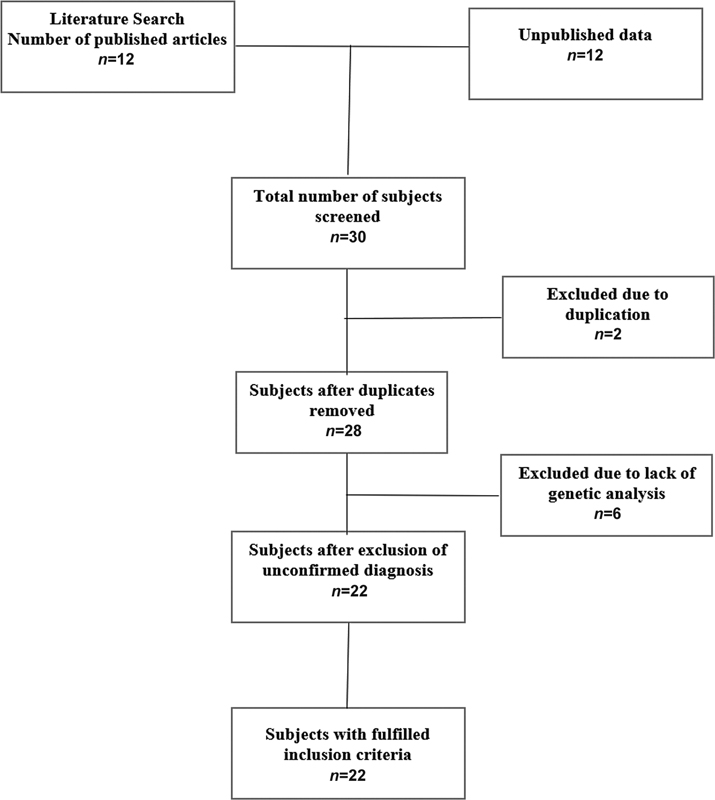
| Fig 1 : Study overview of constitutional mismatch repair deficiency subjects included in the analysis.
Analysis
The median values, IQR, and percentages were calculated from the data.
Various clinical parameters such as age at diagnosis, gender, types of first and second malignancies, consanguinity and other affected family members, and their molecular profiles were analyzed. All patients were also given a score as per the scoring system to determine germline testing eligibility for CMMRD ([Supp. Table S1], available in the online version).
Ethical Approval
The Institutional Ethics Committee had granted approval for this retrospective study (Institutional Ethics Committee, MVR Cancer Centre & Research Institute, Kerala, India).
Approval No.: EC Ref No.: IEC2023/III/02, dated: 08/12/2023.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Results
We analyzed the data of 22 children with genetically confirmed CMMRD from different centers across India. Of the 22 subjects analyzed, 15 were males and 7 were females. The male:female ratio was 2:1. The median age at diagnosis of the first malignancy was 6.5 years (IQR 4–9 years). The median age at diagnosis was 7 years (IQR 4–11 years) and 6 years (IQR 4.4–9 years) for males and females, respectively. In this study, a high incidence of consanguinity was observed. Fourteen of 22 (63.6%) children were born out of a third-degree consanguineous marriage which is a high rate of consanguinity. The parents were unaffected and did not have features of LS.
Sixteen (72.7%) participants had siblings with malignancies. Upon analyzing the clinical parameters, all children had normal development and intelligence (95%), except for one child who had delayed speech development. Skin involvement in the form of café-au-lait macules (CALM) was observed in 16 children (72.7%). One child each had a hypopigmented macule, pilomatricoma, and nevus spilus, in addition to CALMs. All children had strong evidence of CMMRD according to the CMMRD diagnostic criteria as per updated international diagnostic criteria for CMMRD published by Aronson et al in 2022.
All patients were given a score according to the scoring system to determine germline testing eligibility for CMMRD, and the median score in our study was 5.5. A score of ≥ 3 requires testing for MMR gene pathogenic variant. The indications for CMMRD testing are listed in [Supp. Table S1] (available in the online version).
Of all the pathogenic variants analyzed, the most common was in PMS2, accounting for 77.3%. MSH2 and MSH6 constituted 18.2 and 4.5%-of the total, respectively. There were no children with MLH1 pathogenic variant in our study. Additional pathogenic variants were detected in PMS2 (additional second pathogenic variant), POLE, and TP53 genes ([Table 1]).
|
Parameter |
Number (percentage) |
|---|---|
|
Median age at first malignancy (range) |
6.5 y (IQR 4–9 y) |
|
Median age in males |
7 y (IQR 4–11 y) |
|
Median age in females |
6 y (IQR 4.4–9 y) |
|
Sex |
|
|
Male |
15 (68.2) |
|
Female |
7 (21.8) |
|
Consanguineous marriage |
14 (63.6) |
|
Family history |
16 (72.7) |
|
Skin findings |
16 (72.7) |
|
Normal development and intelligence |
21 (95 |
|
Median age at second malignancy, N = 8 |
12 y (IQR 10–15 y |
|
CMMRD score, mean |
6 |
|
Relapse |
5 (24) |
|
Pathologic variants, genes affected |
|
|
PMS2 |
17 (77.2) |
|
MSH2 |
4 (18.1) |
|
MSH6 |
1 (4.5) |
|
MLH1 |
0 (0) |
|
Additional pathologic variants |
PMS2 |
|
POLE |
|
|
TP53 |
|
Genes affected |
Number of patients N (%) |
Median age in years at first malignancy (IQR) |
Median age at second malignancy in years (IQR) |
Skin findings |
Siblings affected |
|---|---|---|---|---|---|
|
PMS2 |
17 (77.2) |
8 (4–5) |
(N = 8) 12 (10–15) |
11 (64%) |
8 |
|
MSH2 |
4 (18.1) |
10 (1–11) |
4 (100%) |
4 |
|
|
MSH6 |
1 (4.5) |
4 |
1 (100%) |
1 |
|
|
MLH1 |
0 |
0 |
|||
|
Total |
22 (100) |
15 |
12 |
|
Type of malignancy |
First malignancy N (%) |
Median age at first malignancy in years (IQR) |
Second malignancy N (%) |
Median age at second malignancy (y) |
|---|---|---|---|---|
|
Hematological |
||||
|
T-ALL |
6 (27.4) |
6 (4–8) |
||
|
B-ALL |
3 (13.6) |
4 (3.5–4.4) |
||
|
NHL |
2 (9) |
4 |
2 (25) |
13 |
|
Brain tumors |
||||
|
GBM/Astrocytoma |
4 (18.2) |
9 (5–11) |
2 (25) |
10.5 |
|
Medulloblastoma |
3 (13,6) |
11 |
||
|
High-grade glioma |
1 (4.6) |
15 |
||
|
Lynch syndrome associated |
||||
|
Colorectal cancer |
2 (9) |
9.5 |
2 (25) |
16 |
|
Other cancers |
||||
|
ASPS |
1 (12.5) |
8 |
||
|
Osteosarcoma |
1 (12.5) |
12 |
||
|
No malignancy |
1 (4.6) |
|||
|
Total |
22 (100) |
8 (100) |
|
Sl. no. |
PMS2 |
Exon |
MSH2 |
Exon |
MSH6 |
Exon |
Homozygous |
First and second malignancies (age at diagnosis in years) |
|---|---|---|---|---|---|---|---|---|
|
1 |
delC |
11 |
Yes |
T-ALL (8); GBM (12) |
||||
|
2 |
delC |
11 |
Yes |
T-ALL (6); ASPS (8) |
||||
|
3 |
double heterozygous (p. Ser815Leu and p.Gln275Gln) |
Yes |
CRC (9); GBM (9) |
|||||
|
4 |
c.1500delC at codon 501 |
11 |
Yes |
GBM (11); CRC (15) |
||||
|
5 |
c.1500delC at codon 501 |
11 |
Yes |
Medulloblastoma (9); NHL (11) |
||||
|
6 |
c.2402C > T |
14 |
Yes |
GBM (9) |
||||
|
7 |
c.2402C > T |
14 |
Yes |
CRC (10) |
||||
|
8 |
c.325dupG |
4 |
Yes |
T-ALL (4); Relapse (8) |
||||
|
9 |
c.325dupG |
4 |
Yes |
T-ALL (4); NHL (15) |
||||
|
10 |
c.325dupG |
4 |
Yes |
NHL (7) |
||||
|
11 |
c.478C > T |
5 |
Yes |
GBM (4) |
||||
|
12 |
(c.221_231del) |
2 |
Yes |
GBM (5) |
||||
|
13 |
(c.221_231del) |
2 |
Yes |
High-grade glioma (15) |
||||
|
14 |
(c.2404C > T) |
14 |
Yes |
|||||
|
15 |
(c.2404C > T) |
14 |
Yes |
B-ALL (4) |
||||
|
16 |
c.1670G > A |
4 |
Yes |
B-ALL (4) Relapse |
||||
|
17 |
c.128_130del |
2 |
Yes |
T-ALL (6); Osteosarcoma (12) |
||||
|
18 |
c.525_534del |
5 |
Yes |
B-ALL (3); Relapse (4) |
||||
|
19 |
c.778del |
7 |
Yes |
Medulloblastoma (12); CRC (17) |
||||
|
20 |
c.778del |
7 |
Yes |
Medulloblastoma (12) |
||||
|
21 |
c.1165C > T |
7 |
Yes |
T-ALL (11 mo) |
||||
|
22 |
c.1165C > T |
7 |
Yes |
NHL (1 y) |
|
Examination |
Start age |
Frequency |
Tumors |
Comment |
|---|---|---|---|---|
|
MRI brain |
At diagnosis |
Q 6 months |
Brain tumors |
Should not be replaced with WBMRI |
|
WBMRI |
6 years |
Once a year |
All tumors |
Should not replace dedicated CNS imaging |
|
CBC |
1 year |
Q 6 months |
Leukemia |
May be considered |
|
Abdominal ultrasound |
1 year |
Q 6 months |
Lymphoma |
May be considered |
|
Upper gastrointestinal endoscopy; video capsule endoscopy, ileocolonoscopy |
4 to 6 years |
Once a year |
Gastrointestinal tumors |
Upper and lower endoscopy, to increase once polyps are found |
|
Gynecological exam, transvaginal ultrasound, pipelle curettage, urine cytology, dipstick |
20 years |
Once a year |
Genitourinary cancers |
As per Lynch syndrome guidelines |
References
Address for correspondence
Publication History
Article published online:
27 September 2024
© 2024. The Author(s). This is an open access article published by Thieme under the terms of the Creative Commons Attribution License, permitting unrestricted use, distribution, and reproduction so long as the original work is properly cited. (https://creativecommons.org/licenses/by/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
- Vitamin D Deficiency in Children with Psychiatric Illness in a Tertiary Care Hospital in North IndiaNidhi Chauhan, Journal of Neurosciences in Rural Practice, 2019
- Role of video capsule endoscopy in patients with constitutional mismatch repair deficiency (CMMRD) syndrome: report from the International CMMRD ConsortiumY. Shimamura, Zentralblatt für Chirurgie - Zeitschrift für Allgemeine, Viszeral-, Thorax- und Gefäßchirurgie, 2018
- Vitamin D Deficiency in Children with Psychiatric Illness in a Tertiary Care Hospital in North IndiaNidhi Chauhan, Journal of Neurosciences in Rural Practice, 2019
- Role of video capsule endoscopy in patients with constitutional mismatch repair deficiency (CMMRD) syndrome: report from the International CMMRD ConsortiumY. Shimamura, EIO, 2018
- Wilms Tumor in India: A Systematic ReviewShyam Srinivasan, South Asian Journal of Cancer
- A review of laser scanning for geological and geotechnical applications in underground mining<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- Experts consensus on management of tooth luxation and avulsion<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- Low prevalence of primary sclerosing cholangitis in patients with inflammatory bowel disease in India<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- From Rimbaud to Verne : a conversation with Ari Sitas : interview<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- Type 2 Diabetes Mellitus Exacerbates Pathological Processes of Parkinson's Disease: Insights from Signaling Pathways Mediated by Insulin Receptors<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
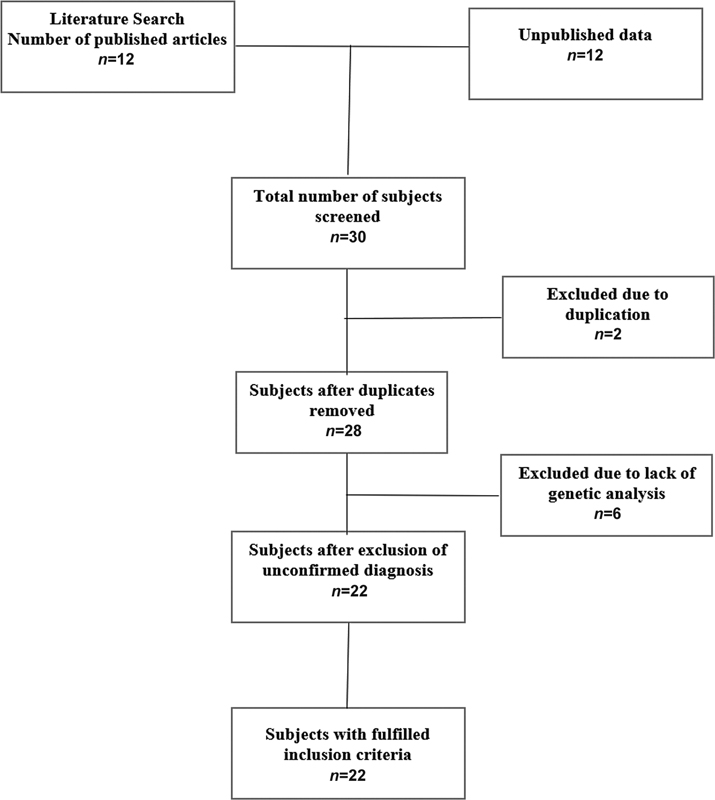
| Fig 1 : Study overview of constitutional mismatch repair deficiency subjects included in the analysis.


 PDF
PDF  Views
Views  Share
Share

