Braving the SARS-CoV-2 Pandemic – Quandary of Health-Care Workers
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2020; 41(04): 454-457
DOI: DOI: 10.4103/ijmpo.ijmpo_245_20
Abstract
Context
Determining how bad health-care providers have been affected by the severe acute respiratory syndrome coronavirus 19 (SARS-CoV-19) pandemic is difficult because governments and organizations have not released this data.
Aims
The aim of the study was to determine the number of health-care workers infected and dead globally due to SARS-CoV-2 infection.
Subjects and Methods
To circumvent these issues, an unconventional approach using Google's programming platform was adopted to aggregate relevant articles reporting the number of confirmed cases and deaths among health-care workers. Locally sourced country-specific data were ensured by individually searching the regional domains of 179 countries.
Results
Reports covering 67 countries showed that 99,847 health-care workers (HCWs) have been reported to be infected with SARS-CoV-2 virus, with a majority reported in Europe. This included confirmed reports of 1732 doctors and 348 nurses. Five hundred and thirty-eight deaths were reported in 32 countries, amounting to a mortality among HCWs globally of 4%.
Conclusions
Although this number might be an underrepresentation of the actual figures out there, it underscores the dire reality of the situation. The information provided is paramount for policymakers to improve services among this vulnerable group.
Keywords
Coronavirus disease 2019 - doctors - health-care workers - nurses - severe acute respiratory syndrome coronavirus 2Publication History
Received: 19 May 2020
Accepted: 25 June 2020
Article published online:
17 May 2021
© 2020. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Context
Determining how bad health-care providers have been affected by the severe acute respiratory syndrome coronavirus 19 (SARS-CoV-19) pandemic is difficult because governments and organizations have not released this data.
Aims
The aim of the study was to determine the number of health-care workers infected and dead globally due to SARS-CoV-2 infection.
Subjects and Methods
To circumvent these issues, an unconventional approach using Google's programming platform was adopted to aggregate relevant articles reporting the number of confirmed cases and deaths among health-care workers. Locally sourced country-specific data were ensured by individually searching the regional domains of 179 countries.
Results
Reports covering 67 countries showed that 99,847 health-care workers (HCWs) have been reported to be infected with SARS-CoV-2 virus, with a majority reported in Europe. This included confirmed reports of 1732 doctors and 348 nurses. Five hundred and thirty-eight deaths were reported in 32 countries, amounting to a mortality among HCWs globally of 4%.
Conclusions
Although this number might be an underrepresentation of the actual figures out there, it underscores the dire reality of the situation. The information provided is paramount for policymakers to improve services among this vulnerable group.
Keywords
Coronavirus disease 2019 - doctors - health-care workers - nurses - severe acute respiratory syndrome coronavirus 2Introduction
Across the globe, millions are coping with restrictions imposed by their governments in an effort to minimize the transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). At the same time, health-care workers (HCWs) are preparing for the opposite, putting themselves at the highest risk of contracting the virus. Doctors and nurses across the spectrum are at the frontlines of the coronavirus disease 2019 (COVID-19) response and are routinely exposed to the hazards including direct contact with the pathogen, long working hours, mental and physical fatigue, stigma, burnout, and psychological violence.
Understanding the impact of this is essential, and yet, structured prospective trials are difficult given the pace of this contagion. Simultaneously, organizations are consistently reporting updated metrics to understand the extent of this pandemic. Most publishers have made resources related to the coronavirus freely available in an effort to further general awareness as well as enable deeper research, while governments are sparingly releasing data about those infected. Worryingly, the potential impact of an unhealthy medical infrastructure has also not been adequately captured by administrations across the globe. This has left people to rely on the media as a key source of real-time information about the coronavirus. In this interesting time for research and reporting, and as an important consideration for the health of our global population, we are aiming to use these critical media sources to estimate the number of health-care workers that have both been infected and succumbed to this rampant virus.
Subjects and Methods
We initially performed a systematic search of PubMed, Embase, and Google Scholar from inception till May 5, 2020, as per the GATHER guidelines. Our search resulted in one publication reporting the number of “healthcare workers,” “doctors,” or “nurses” being “infected” or “dying” due to “coronavirus,” “SARS-CoV-2” or “COVID-19” at a population level.[1] Our definition of HCWs included doctors, nurses, and any other hospital or paramedical staff working with COVID-19 patients. Hence, using the same search string, we adopted an unconventional approach to circumvent the above issues in these unusual times. Integrating Google's search engine platform to the standard GATHER guidelines, we aggregated the relevant articles that fit our inclusion criteria by individually searching the regional domains of 179 countries. This ensured locally sourced country-specific data. Since the results obtained were mostly from news reports, both authors A. G. S and P. C reviewed each article for the authenticity of the source, i.e., from the government or health ministry, as well as the media owner. Articles were sorted by country and date, followed by excluding the overlapping cases. Since the reports were published on different dates, we obtained the total confirmed cases and the total death count of infected persons from the World Health Organization (WHO) situation reports of that day.[2] Since the incidence and mortality would depend on the overall population tested for the virus and currently countries having different policies for testing, we considered taking an absolute number for representation as well. All the analyses and charts were prepared on Office 365 Personal, ©Microsoft 2020.
Results
As per our search results, 99,847 HCWs have been reported to be infected with SARS-CoV-2 virus across 67 countries up to May 5, 2020, with a majority being reported in Europe [Figure 1]. This included confirmed reports of 1732 doctors and 348 nurses. A little less than a fifth of the transmissions took place in hospitals presumably from infected patients, 8%-were due to travel from endemic regions, 3%-was presumably due to doctors being infected outside of their work environments, while a majority of reports did not include the likely source. Among the ones who did report, the most vulnerable subspecialties getting infected were physicians and anesthetists, followed by urologists and oncologists. Other than a high rate of infection among HCWs at the “coronavirus hospitals,” few reports also suggested that HCWs in oncology hospitals were infected in Egypt, India, Australia, and Italy. The countries with a low population index had a higher rate of HCWs that are being infected.
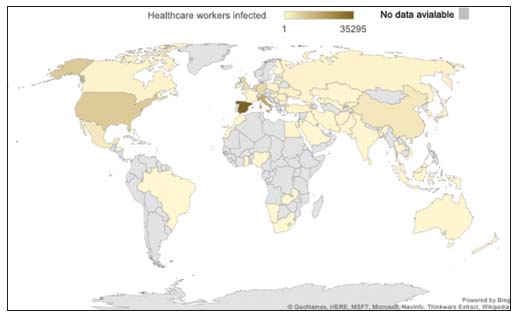
| Figure 1:Health-care workers infected due to severe acute respiratory syndrome coronavirus 2
Eight percent of the globally reported infections were HCWs. Every second person infected in Afghanistan and the Republic of Moldova was an HCW. One in every four to five people infected in Kyrgyzstan, the Netherlands, Ireland, Ukraine, Poland, and Spain were HCWs [Figure 2]. Five hundred and thirty-eight deaths form SARS-CoV-2 infection were reported in 32 countries. The mortality among HCWs globally was 4%-(range – 0%–22%) [Figure 3]. The percentage of HCWs infected and dead in developing countries was higher than the developed countries [Supplementary Table 1] [SUPPORTING:1].
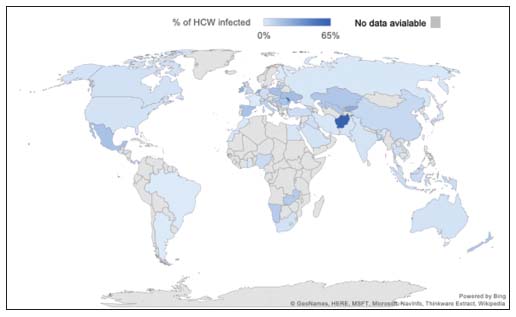
| Figure.2:Health-care workers infected relative to the total cases confirmed of severe acute respiratory syndrome coronavirus 2 infection
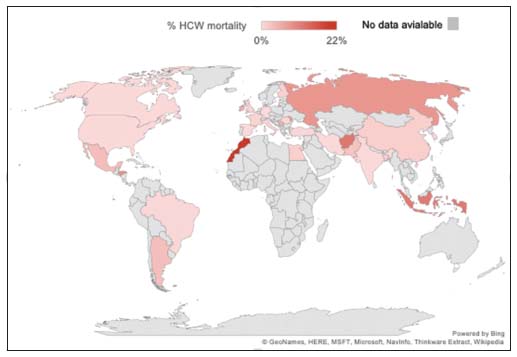
| Figure.3:Deaths of health-care workers relative to the total deaths due to severe acute respiratory syndrome coronavirus 2 infection
Discussion
What do the numbers signify?
Gauging how bad health-care providers have been hit is difficult because governments, medical associations, or workers unions have not released these data. In fact, among the search results, only a few countries had a reasonable freedom of press – the worst being China, Vietnam, Saudi Arabia, Iran, and Egypt.[3] With scant reports underestimating their numbers, no systematic reports exist to address this issue and this number might be an underrepresentation of the actual figures out there. As of April 8, 2020, the WHO situation report suggested that 22,073 HCWs were infected across the 52 countries.[2] This was a fourth of the number we found through the reports from local agencies, although this was about a month before our analysis. We do acknowledge that the data obtained for this summary are not from “conventional” publications, but they underscore the dire reality of the situation. In countries where the disease emerged early on, such as China, the fatality rate is likely much higher as people were not looking for a new disease and would miss the early progressive cases. On the contrary, another reason for these high rates later in the course of the pandemic could be a trait among physicians, known as ascertainment bias. During large-scale outbreaks, health-care providers are more likely to attribute a death with complex causes as being caused by the disease in question. Nonetheless, a study has shown that the overall case-fatality rate for the infected is 1.38%, which is still substantially higher than of the recent outbreaks such as swine flu that had a fatality of 0.1%.[4] Assuming that each infected HCWs would have come in contact with a minimum of ten colleagues before being diagnosed, approximately half the global health-care force should be in quarantine. Further, these figures are made up of a majority of symptomatic cases that have undergone testing early. Since it is estimated that up to 80%-of the tested population may be asymptomatic carriers, the true number of infected HCWs could be ginormous.[5]
What's to come?
Even though studies have shown the virus does not mutate very quickly, these figures are substantially varied across geographic locations.[6] Apart from the disease-related factors, the biggest influence is the way these metrics are being gathered and reported. Countries have varied approaches ranging from widespread testing to a theory of herd immunity where minimal testing is required.[7],[8] With the worst yet to come, health systems in high-income countries are already reporting protective gear shortages, lax protocols, and high levels of stress in hospitals.[9] This makes an already bleak situation worse. An interesting report has shown that the employment of health-care staff per 1000 of the population varies significantly among countries of similar size and wealth. In fact, countries with lower population coverage rates such as the United States (10.6%), Spain (9.1%), and Italy (7.6%) have their health systems strained at a proportionate rate by SARS-CoV-2 compared to countries such as Switzerland (17.4%).[10] With the onset of SARS-CoV-2, this problem will become increasingly acute, with most countries not being able to replace the number of medical workers being infected by SARS-CoV-2.[9]
To make matters worse, in addition to the high risk of infection, HCWs are becoming prey to societal abuse. Reports are emerging of doctors and nurses in India, the United Kingdom, Myanmar, and Mexico being evicted from their residences in the fear that they would transmit the infection.[11] Medical workers are confronted daily with difficult triage decisions and the pain of losing colleagues. With the current scenario escalating, the next global crisis will be a shortage of doctors and nurses. Hospitals might become the main SARS-CoV-19 sources as infected patients are rapidly populating them. This could deliver a detrimental blow to the human toll and deteriorate the capacity of health systems.
Understanding the impact of the altruistic behavior of HCWs is essential and yet impossible given the pace of this contagion. The health system in India needs to improve the safety of HCWs. A greater number of protective equipment need to be deployed to the frontline workers. Justified working schedules need to be considered to take into account the mental and physical fatigue HCWs face. The government policies should include providing provisions to the HCWs in the event of being infected. In terms of absolute figures reported, the health-care burden of high-income countries could provide a frightening preview of the numbers that are to come in other countries that are already overwhelmed by SARS-CoV-2 and medical personnel put at risk. The information provided though our analysis could prove vital for policymakers to improve protection among this vulnerable group. We urge the governments to take appropriate action incorporating the collective suggestions from the apex centers of infectious diseases in their countries.
Conclusion
Although the incidence might be an underrepresentation of the actual figures out there, these results underscore the dire reality of the situation. Making the epidemiological data available is paramount to strengthen our understanding of the virus.
Conflict of Interest
There are no conflicts of interest.
Supplementary Material
References
- Stevens GA, Alkema L, Black RE, Boerma JT, Collins GS, Ezzati M. et al. Guidelines for accurate and transparent health estimates reporting: The GATHER statement. Lancet 2016; 388: e19-23
- Novel Coronavirus (2019-nCoV) Situation Reports. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports Available from: [Last accessed on 2020 May 10]
- Tracker_19. RSF. 2020 https://rsf.org/en/tracker19-Coronavirus-Covid19 Available from: [Last accessed on 2020 Apr 10]
- Verity R, Okell LC, Dorigatti I, Winskill P, Whittaker C, Imai N. et al. Estimates of the severity of coronavirus disease 2019: A model-based analysis. [published correction appears in Lancet Infect Dis. 2020 Apr 15] [published correction appears in Lancet Infect Dis. 2020 May 4]. Lancet Infect Dis 2020; 20: 669-77
- COVID-19: What Proportion are Asymptomatic? CEBM. https://www.cebm.net/covid-19/covid-19-what-proportion-are-asymptomatic/. Available from: [Last accessed on 2020 Apr 10]
- Tang X, Wu C, Li X, Song Y, Yao X, Wu X. On the origin and continuing evolution of SARS-CoV-2. Natl Sci Rev 2020; nwaa036 et al. Published 2020 Mar 3
- Kwok KO, Lai F, Wei WI, Wong SYS, Tang JWT. Herd immunity-estimating the level required to halt the COVID-19 epidemics in affected countries. J Infect 2020; 80: e32-3
- Jin YH, Cai L, Cheng ZS, Cheng H, Deng T, Fan YP. Rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version). Mil Med Res 2020; 7: 4 et al. Published 2020 Feb 6
- Wang X, Zhang X, He J. Challenges to the system of reserve medical supplies for public health emergencies: Reflections on the outbreak of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) epidemic in China. Biosci Trends 2020; 14: 3-8
- OECD Health Statistics 2019 OECD. http://www.oecd.org/els/health-systems/health-data.htm Available from: [Last accessed on 2020 Apr 10]
- Yeung J, Gupta S. Doctors in India Evicted from their Homes as Coronavirus Fear Spreads. CNN. https://www.cnn.com/2020/03/25/asia/india-coronavirus-doctors-discrimination-intl-hnk/index.html. Available from: [Last accessed on 2020 Apr 10]
Address for correspondence
Publication History
Received: 19 May 2020
Accepted: 25 June 2020
Article published online:
17 May
2021
© 2020. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301
UP, India
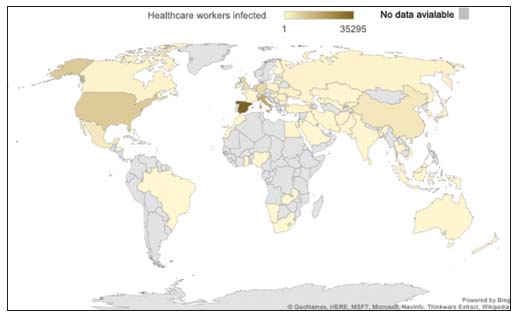
| Figure 1:Health-care workers infected due to severe acute respiratory syndrome coronavirus 2
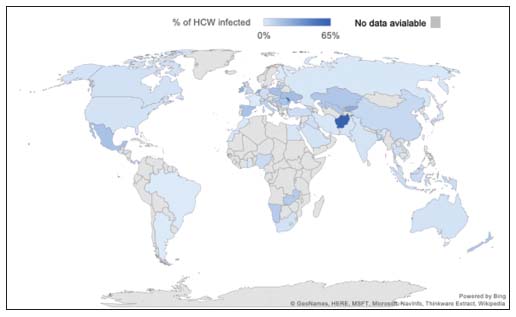
| Figure.2:Health-care workers infected relative to the total cases confirmed of severe acute respiratory syndrome coronavirus 2 infection
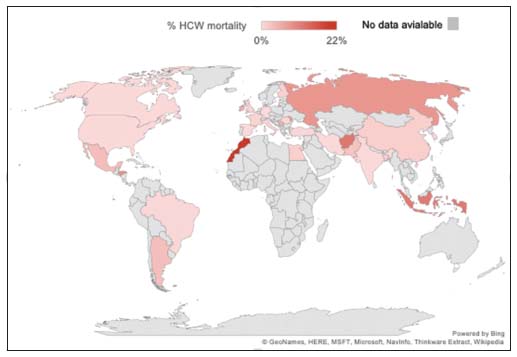
| Figure.3:Deaths of health-care workers relative to the total deaths due to severe acute respiratory syndrome coronavirus 2 infection
References
- Stevens GA, Alkema L, Black RE, Boerma JT, Collins GS, Ezzati M. et al. Guidelines for accurate and transparent health estimates reporting: The GATHER statement. Lancet 2016; 388: e19-23
- Novel Coronavirus (2019-nCoV) Situation Reports. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports Available from: [Last accessed on 2020 May 10]
- Tracker_19. RSF. 2020 https://rsf.org/en/tracker19-Coronavirus-Covid19 Available from: [Last accessed on 2020 Apr 10]
- Verity R, Okell LC, Dorigatti I, Winskill P, Whittaker C, Imai N. et al. Estimates of the severity of coronavirus disease 2019: A model-based analysis. [published correction appears in Lancet Infect Dis. 2020 Apr 15] [published correction appears in Lancet Infect Dis. 2020 May 4]. Lancet Infect Dis 2020; 20: 669-77
- COVID-19: What Proportion are Asymptomatic? CEBM. https://www.cebm.net/covid-19/covid-19-what-proportion-are-asymptomatic/. Available from: [Last accessed on 2020 Apr 10]
- Tang X, Wu C, Li X, Song Y, Yao X, Wu X. On the origin and continuing evolution of SARS-CoV-2. Natl Sci Rev 2020; nwaa036 et al. Published 2020 Mar 3
- Kwok KO, Lai F, Wei WI, Wong SYS, Tang JWT. Herd immunity-estimating the level required to halt the COVID-19 epidemics in affected countries. J Infect 2020; 80: e32-3
- Jin YH, Cai L, Cheng ZS, Cheng H, Deng T, Fan YP. Rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version). Mil Med Res 2020; 7: 4 et al. Published 2020 Feb 6
- Wang X, Zhang X, He J. Challenges to the system of reserve medical supplies for public health emergencies: Reflections on the outbreak of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) epidemic in China. Biosci Trends 2020; 14: 3-8
- OECD Health Statistics 2019 OECD. http://www.oecd.org/els/health-systems/health-data.htm Available from: [Last accessed on 2020 Apr 10]
- Yeung J, Gupta S. Doctors in India Evicted from their Homes as Coronavirus Fear Spreads. CNN. https://www.cnn.com/2020/03/25/asia/india-coronavirus-doctors-discrimination-intl-hnk/index.html. Available from: [Last accessed on 2020 Apr 10]


 PDF
PDF  Views
Views  Share
Share

