Congenital Epulis
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2022; 43(04): 376-377
DOI: DOI: 10.1055/s-0042-1754372
Congenital epulis is a benign tumor that occurs in newborns. It was first described by Neumann in 1871; hence, it came to be known as Neumann's tumor. It is also known as granular cell rhabdomyoma, congenital myoblastoma, or congenital granular cell tumor.[1] The female infant is usually affected but has no familial tendency. It not only arises from alveolar median ridge of the maxilla and mandible but can also originate from tongue, palate, skin, etc. Therefore, the etiology and cell of origin of this tumor are still not clear.[1] [2] It is hypothesized that this tumor arises from several sources: undifferentiated mesenchymal cells, odontogenic epithelial cells, neuroendocrine progenitor cells, pericytes, histiocytes, fibroblasts, or myofibroblast. The steroidal hormones were believed to play a role but this was disproved due to the absence of estrogen and progesterone receptors in the tumor tissue.[3]
A newborn female presented with a large protruding mass in the mouth causing difficulty in breathing and breastfeeding ([Fig. 1)]. A probable diagnosis of congenital epulis was made based on clinical examination. Surgical excision of the mass was performed under general anesthesia ([Fig. 2)]. Postoperative period was uneventful. The specimen was sent for histopathological examination. On gross examination, it consists of single mass covered by gray-brown, firm mucosa with the dimensions of 2.8 × 2 × 1 cm3 ([Fig. 3)]. The outer surface was smooth. The cut section showed whitish and hemorrhagic areas. The nearest resected margin was found to be 0.8 cm.

| Figure 1:Pre operative image.

| Figure 2:Intra operative Image.
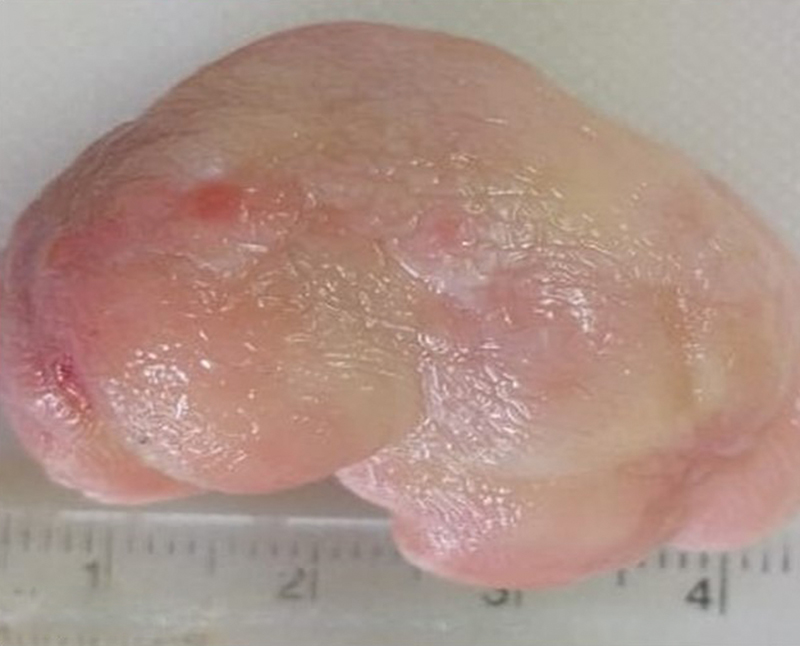
| Figure 3:Gross specimen.
Microscopy revealed large round-to-oval cells with granular eosinophilic cytoplasm and small eccentric, bland nuclei. There was presence of thin fibrovascular network separating the cells. Necrosis and mitosis were not evident. The overlying epithelium was thin and pseudoepitheliomatous hyperplasia was not evident ([Fig. 4)]. All the resected margins were not involved by tumor. On the basis of these findings, the final diagnosis of congenital granular cell tumor was made. Immunohistochemistry (IHC) was not performed as the microscopy findings were characteristic.
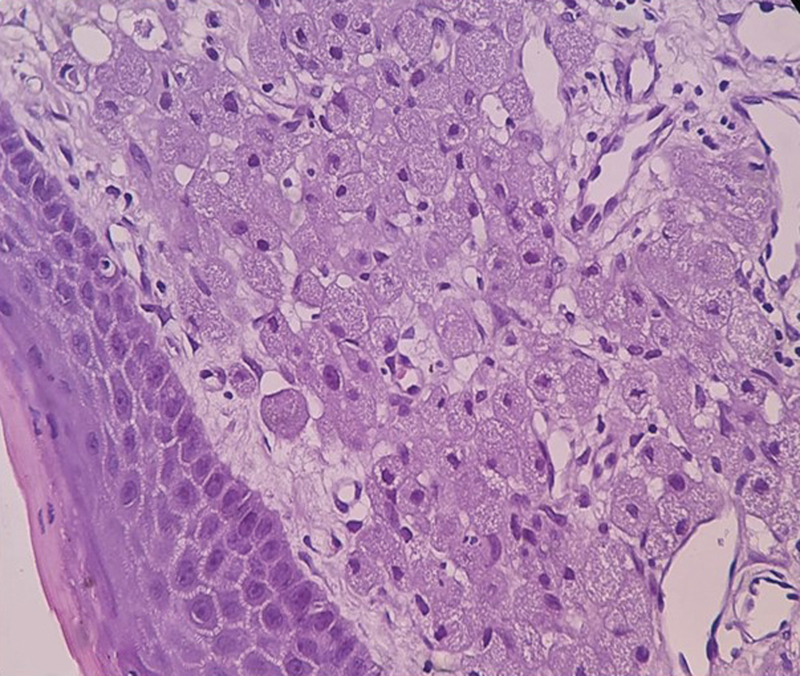
| Figure 4:H&E 40X, showing large round to oval cells with granular eosinophilic cytoplasm and small eccentric bland nuclei.
It is a rare non-neoplastic soft tissue lesion. Prenatal diagnosis can be done by ultrasonography mainly in the last week of pregnancy.[4] This can help in counseling the parents about the possible complications and treatment of the tumor mass. It should be removed postnatally if the size of the mass is big as it can cause difficulty in breathing and feeding.[2] [4]
Surgical excision is the only treatment, though spontaneous regression has also been observed in a few cases. It does not have malignant potential and recurrence rate.4
It presents as single polypoidal protruding mass covered by smooth mucosal surface and firmly attached to the gum by a broad base. The histopathology findings are characteristic. On IHC, the cells are positive for vimentin and negative for S-100 unlike in adults.[1] [5]
It is important to diagnose it both prenatally and postnatally. This will help the oncologist involved in planning the possible intervention and thereby decreasing the morbidity and mortality. The parents can also understand the nature of the mass by consulting the oncologist.
Publication History
Article published online:
01 September 2022
© 2022. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Congenital epulis is a benign tumor that occurs in newborns. It was first described by Neumann in 1871; hence, it came to be known as Neumann's tumor. It is also known as granular cell rhabdomyoma, congenital myoblastoma, or congenital granular cell tumor.[1] The female infant is usually affected but has no familial tendency. It not only arises from alveolar median ridge of the maxilla and mandible but can also originate from tongue, palate, skin, etc. Therefore, the etiology and cell of origin of this tumor are still not clear.[1] [2] It is hypothesized that this tumor arises from several sources: undifferentiated mesenchymal cells, odontogenic epithelial cells, neuroendocrine progenitor cells, pericytes, histiocytes, fibroblasts, or myofibroblast. The steroidal hormones were believed to play a role but this was disproved due to the absence of estrogen and progesterone receptors in the tumor tissue.[3]
A newborn female presented with a large protruding mass in the mouth causing difficulty in breathing and breastfeeding ([Fig. 1)]. A probable diagnosis of congenital epulis was made based on clinical examination. Surgical excision of the mass was performed under general anesthesia ([Fig. 2)]. Postoperative period was uneventful. The specimen was sent for histopathological examination. On gross examination, it consists of single mass covered by gray-brown, firm mucosa with the dimensions of 2.8 × 2 × 1 cm3 ([Fig. 3)]. The outer surface was smooth. The cut section showed whitish and hemorrhagic areas. The nearest resected margin was found to be 0.8 cm.

| Figure 1:Pre operative image.

| Figure 2:Intra operative Image.
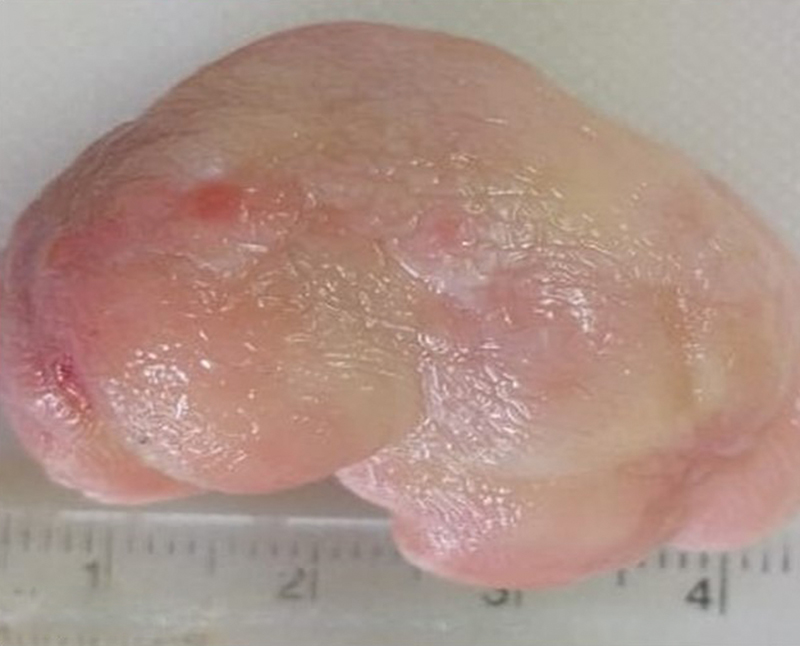
| Figure 3:Gross specimen.
Microscopy revealed large round-to-oval cells with granular eosinophilic cytoplasm and small eccentric, bland nuclei. There was presence of thin fibrovascular network separating the cells. Necrosis and mitosis were not evident. The overlying epithelium was thin and pseudoepitheliomatous hyperplasia was not evident ([Fig. 4)]. All the resected margins were not involved by tumor. On the basis of these findings, the final diagnosis of congenital granular cell tumor was made. Immunohistochemistry (IHC) was not performed as the microscopy findings were characteristic.
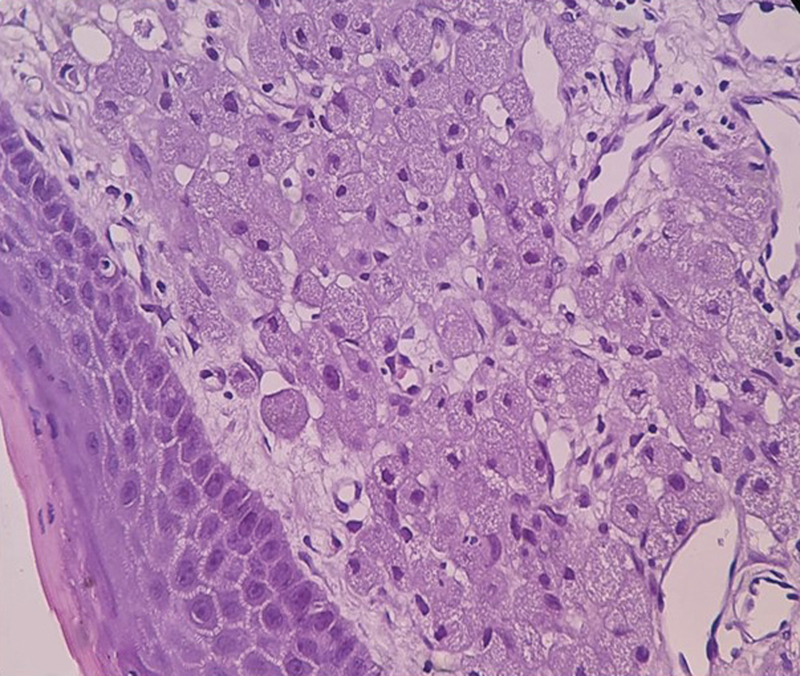
| Figure 4:H&E 40X, showing large round to oval cells with granular eosinophilic cytoplasm and small eccentric bland nuclei.
It is a rare non-neoplastic soft tissue lesion. Prenatal diagnosis can be done by ultrasonography mainly in the last week of pregnancy.[4] This can help in counseling the parents about the possible complications and treatment of the tumor mass. It should be removed postnatally if the size of the mass is big as it can cause difficulty in breathing and feeding.[2] [4]
Surgical excision is the only treatment, though spontaneous regression has also been observed in a few cases. It does not have malignant potential and recurrence rate.4
It presents as single polypoidal protruding mass covered by smooth mucosal surface and firmly attached to the gum by a broad base. The histopathology findings are characteristic. On IHC, the cells are positive for vimentin and negative for S-100 unlike in adults.[1] [5]
It is important to diagnose it both prenatally and postnatally. This will help the oncologist involved in planning the possible intervention and thereby decreasing the morbidity and mortality. The parents can also understand the nature of the mass by consulting the oncologist.
Conflict of Interest
None declared.
References
- Lapid O, Shaco-Levy R, Krieger Y, Kachko L, Sagi A. Congenital epulis. Pediatrics 2001; 107 (02) E22
- Chattopadhyay A, Patra R, kumar Vijay. Oral tumors in newborn. Indian J Pediatr 2003; 70 (07) 587-588
- Conrad R, Perez MC. Congenital granular cell epulis. Arch Pathol Lab Med 2014; 138 (01) 128-131
- Williams RW, Grave B, Stewart M, Heggie AA. Prenatal and postnatal management of congenital granular cell tumours: a case report. Br J Oral Maxillofac Surg 2009; 47 (01) 56-58
- Kumar RM, Bavle RM, Umashankar DN, Sharma R. Congenital epulis of the newborn. J Oral Maxillofac Pathol 2015; 19 (03) 407
Address for correspondence
Publication History
Article published online:
01 September 2022
© 2022. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India

| Figure 1:Pre operative image.

| Figure 2:Intra operative Image.
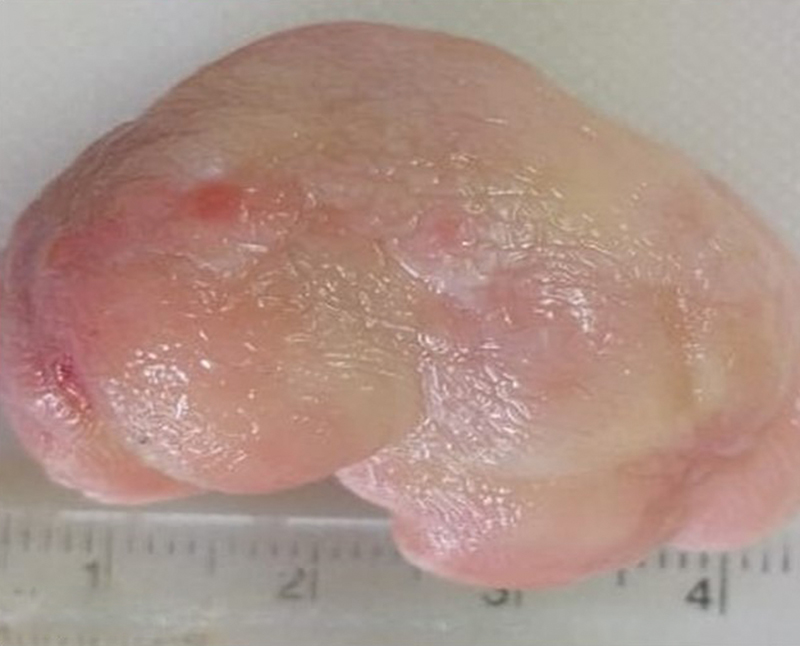
| Figure 3:Gross specimen.
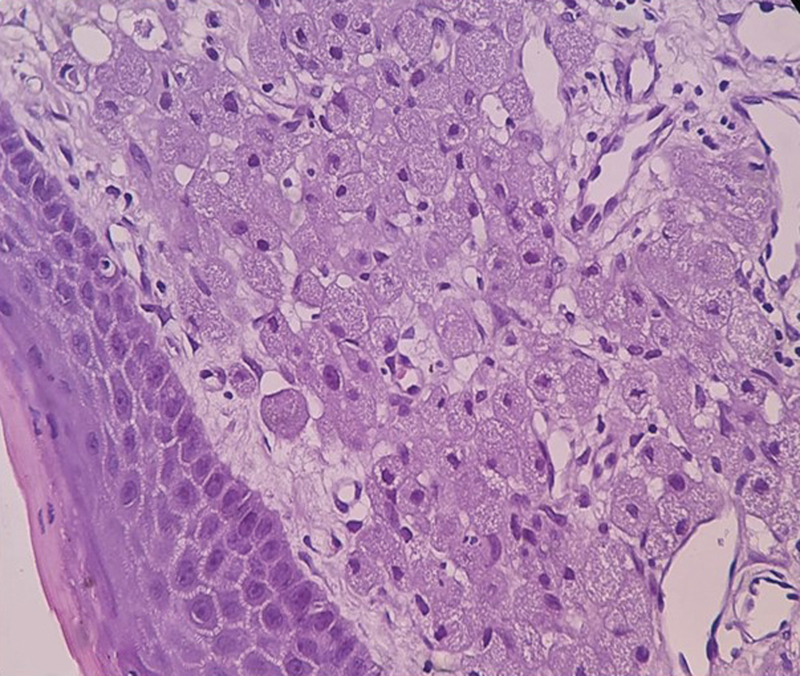
| Figure 4:H&E 40X, showing large round to oval cells with granular eosinophilic cytoplasm and small eccentric bland nuclei.
References
- Lapid O, Shaco-Levy R, Krieger Y, Kachko L, Sagi A. Congenital epulis. Pediatrics 2001; 107 (02) E22
- Chattopadhyay A, Patra R, kumar Vijay. Oral tumors in newborn. Indian J Pediatr 2003; 70 (07) 587-588
- Conrad R, Perez MC. Congenital granular cell epulis. Arch Pathol Lab Med 2014; 138 (01) 128-131
- Williams RW, Grave B, Stewart M, Heggie AA. Prenatal and postnatal management of congenital granular cell tumours: a case report. Br J Oral Maxillofac Surg 2009; 47 (01) 56-58
- Kumar RM, Bavle RM, Umashankar DN, Sharma R. Congenital epulis of the newborn. J Oral Maxillofac Pathol 2015; 19 (03) 407


 PDF
PDF  Views
Views  Share
Share

