Epidemiological review of gastric cancer in India
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2011; 32(01): 3-11
DOI: DOI: 10.4103/0971-5851.81883
Abstract
Stomach cancer is the one of the leading cause of cancer in southern region of India. Its incidence is decreasing worldwide yet on global scale stomach cancer remains one of the most common causes of cancer death. Etiology of gastric cancer includes Helicobacter pylori infection, diet and lifestyle, tobacco, alcohol and genetic susceptibility. In this review, we tried to find the contribution of Indian scientist in understanding the descriptive and observational epidemiology of stomach cancer. PubMed was used as a search platform using key words such as "stomach cancer, treatment, clinical characteristics, stomach cancer outcome, epidemiology, etiological factor and their corresponding Mesh terms were used in combination with Boolean operators OR, AND". Most of the reported studies on gastric cancer from India are case report or case series and few are case-control studies. Indian studies on this topic are limited and have observed H. pylori infection, salted tea, pickled food, rice intake, spicy food, soda (additive of food), tobacco and alcohol as risk factors for gastric cancer. More research is required to understand the etiology, develop suitable screening test, to demarcate high-risk population and to develop and evaluate the effect of primary prevention programs.
Publication History
Article published online:
16 August 2021
© 2011. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Stomach cancer is the one of the leading cause of cancer in southern region of India. Its incidence is decreasing worldwide yet on global scale stomach cancer remains one of the most common causes of cancer death. Etiology of gastric cancer includes Helicobacter pylori infection, diet and lifestyle, tobacco, alcohol and genetic susceptibility. In this review, we tried to find the contribution of Indian scientist in understanding the descriptive and observational epidemiology of stomach cancer. PubMed was used as a search platform using key words such as “stomach cancer, treatment, clinical characteristics, stomach cancer outcome, epidemiology, etiological factor and their corresponding Mesh terms were used in combination with Boolean operators OR, AND”. Most of the reported studies on gastric cancer from India are case report or case series and few are case-control studies. Indian studies on this topic are limited and have observed H. pylori infection, salted tea, pickled food, rice intake, spicy food, soda (additive of food), tobacco and alcohol as risk factors for gastric cancer. More research is required to understand the etiology, develop suitable screening test, to demarcate high-risk population and to develop and evaluate the effect of primary prevention programs.
INTRODUCTION
Stomach cancer is the second-most common cancer among men and third-most among females in Asia and worldwide.[1] The symptoms and sign of the stomach cancer are often reported late when the disease is already in advanced stages and 5-year survival is less than 30% in developed countries and around 20% in developing countries.[2]
About 8.6% of all cancers that occurred in 2002 were gastric cancer. The gastric cancer rates shows marked geographical variation, with high-risk areas in Japan, China, Eastern Europe and certain countries in Latin America. Low-risk population is seen among whites in North America, India, Philippines, most countries in Africa, some Western European countries and Australia.[2] In India, the number of new stomach cancer cases in 2001 was estimated to be approximately 35,675 (n=23,785 in men; 11,890 in women).[3] These differences in incidence rates can be attributed to many factors but refer particularly to differences in dietary habits, and infection to Helicobacter pylori.
This review includes an update of distribution of gastric cancer in India, as well as systematic review of published findings on association between various risk factors related to gastric cancer.
MATERIALS AND METHODS
A search was undertaken in MEDLINE (www.pubmed.com) using Pubmed database, using key words such as “stomach cancer, treatment, clinical characteristics, stomach cancer outcome, epidemiology, etiological factor and their corresponding Mesh terms were used in combination like OR, AND.” The search was limited to only English literature including those studies which were published from 2000 to 2009 by Indian institutes only. This search yielded a total of 256 articles of which the following studies were excluded: Animal model (48), studies which were not conducted in India (13), studies other than gastric cancer (25), case reports (42) and other studies unrelated to the topic concerned (80) as these studies did not satisfy the review purpose. Total 48 studies fulfilled the inclusion criterion. The descriptive health statistical data for gastric cancer was mainly obtained from publications of National Cancer Registry, UICC, IARC and WHO (GLOBOCON-2008). In most of the case-control studies definition of gastric cancer used was not specified.
DESCRIPTIVE EPIDEMIOLOGY
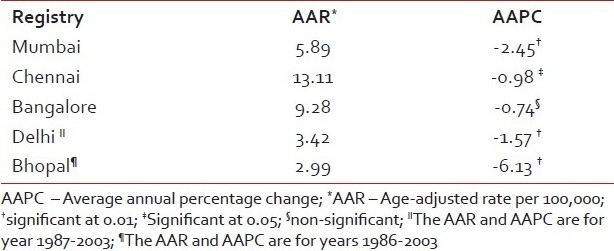
The data obtained from the National Cancer Registries indicates that gastric cancer is a leading problem in North-eastern and Southern states of Indian subcontinent [Tables [Tables11 and and2].2]. The rates for gastric cancer in North-eastern registries are higher than rest of the countries. However, this should be interpreted with caution as these registries are in initial years of registry operation, and it has been demonstrated that registries might include prevalent cases in their initial years. The age-adjusted incidence rate of stomach cancer in males varies widely among registries, highest being 11.1 per 100,000 in Chennai compared to 1.6 per 100,000 in Bhopal.[4] Similar to trends of stomach cancer globally, Indian registries have also observed statistically significant decreasing trend over the last 20-year period [Table 3].
Table 1
Age-adjusted (world) incidence and mortality rates of gastric cancer* and its relative proportion in Indian population-based cancer registries. Years: 2001-2003
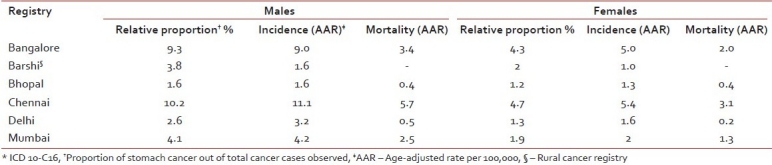
Table 2
Age-adjusted (world) incidence and mortality rates of gastric cancer and its relative proportion in population-based cancer registries from North-Eastern region of India. Years: 2003-2004
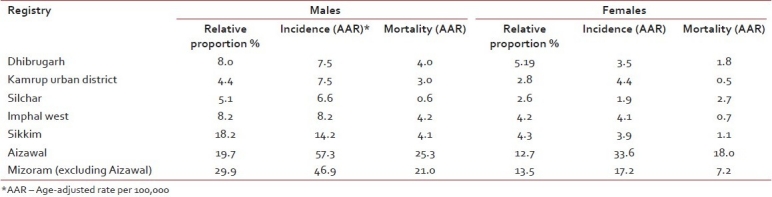
Table 3
The age-adjusted (world) incidence rates and AAPC for gastric cancer in males in Indian population-based cancer registry during the years 1982-2003
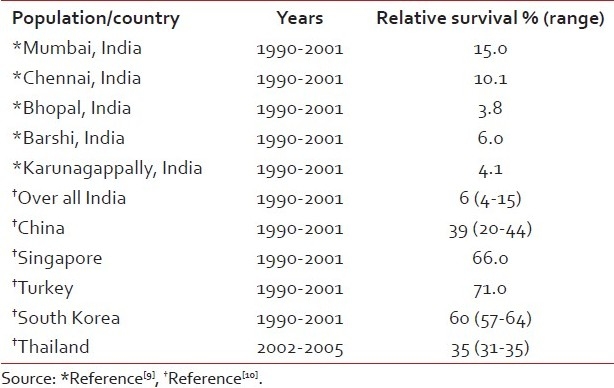
The mortality figures from Indian registries suffer with problem of under-reporting because of problems in registration of death and in reporting of cause of death. The Mumbai registry with comparative reliable mortality (owing to stringent implication of Coroners Act) data reports decline in mortality rate from 2.7 for females and 4.8 for males in 1994[5] to 1.7 for females and 1.8 for males in 2005.[6] The population-based survival studies, another indicator of health infrastructure and success of treatment, indicate that despite improvement in treatment modalities, prognosis from stomach cancer remains to be poor. The 5-year survival rate for stomach cancer is approximately 20%. Survival rates are higher in countries which have screening programs that lead to early detection and where distal cancer (which has a better prognosis) predominates.[7] The 5-year relative survival for stomach cancer in India from 1992 to 1994 was observed to be 6%.[8] The 5-year age standardized relative survival in the age group of 0-74 years for different Indian registries and its comparison with other Asian registries is shown in Table 4.
Table 4
Age-standardized relative survival in the 0-74 years age group in selected Indian populations
RISK FACTORS
H. pylori – The most important risk factor for stomach cancer is observed to be the infection with H. pylori. IARC monograph classifies H. pylori as a carcinogenic to humans based on epidemiological evidence.[11] A large number of case-control and cohort studies conducted in various parts of the world observed 2-3-fold increase in gastric cancer among individuals exposed compared to non-exposed to H. pylori infection after adjusting for important covariants.[12–14] The Cag A gene is the main virulence factor of H. pylori which is responsible for the development of gastric adenocarcinoma through derangement of cellular architecture and signaling pathway.[2] The prevalence of H. pylori is high in India as observed by many case series. The prevalence varies from 56 to 89% among gastric cancer cases. A study from North India reported the prevalence of H. pylori infection to be 56.5% in gastric cancer patients.[15] The frequency of Cag A IgG was found to be more common in the healthy controls (89%) compared to gastric neoplasm patients (76%).[16] A study by Mishra et al.,[17] showed slightly higher prevalence of H. pylori (80%) in the control group as compared to the cases (78%). It was also reported that H. pylori was more common in diffuse type of cancer than intestinal type (86% vs. 68%).
Another study from Northern India reported the prevalence of H. pylori as high as 74% in controls as compared to 68% in gastric cancer cases.[18]
A study from Mizoram reported higher rate of infection by H. pylori in stomach cancer patients. The study failed to show any significant association of IgG (OR-0.66; CI-0.29-1.32), IgM (OR-0.41; CI-0.17-1.50) and IgA (OR-1.15; CI-0.12-2.0) antibody levels against the H. pylori in development of gastric cancer after adjusting for important confounding factors. The significant interaction between H. pylori infection and smoked, salted meat (OR 1.9) and Sa-um which is a locally made dish (OR-2.1) was observed.[19] The techniques used by these studies to detect H. pylori infection included RUT (rapid urease test), culture, histopathology, PCR and ELISA which are endoscopy and serology based.
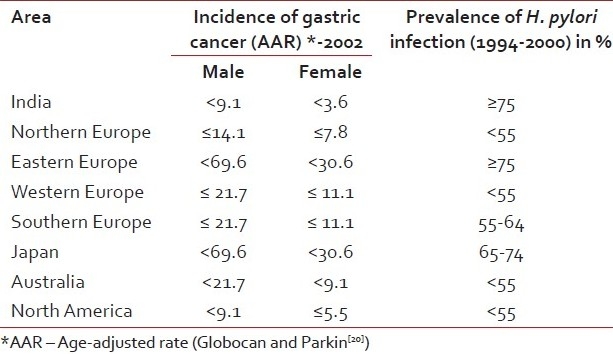
The studies conducted in India over the last 10 years fails to confirm the association between H. pylori infection and gastric cancer. This is mainly because of high prevalence of H. pylori infection in Indian population and small sample size of most of the studies. Further it is important to be able to adjust for other confounding variables. The studies with adequate power and addressing the issue of interaction between H. pylori and other lifestyle-related factors and dietary variables will be important to understand the etiology of gastric cancer in India in relation to H. pylori infection [Table 5].
Table 5
Mean prevalence of infection by Helicobacter pylori in adults by world area and incidence of stomach cancer
DIET AND LIFESTYLE
Diet plays a major role in gastric carcinogenesis. Globally, literature suggests that none or low-starch vegetable including green yellow vegetables, cruciferous and allium vegetables (garlic and onion) and fruits are considered to be probable protective factors. Limited evidence suggests that pulses (including soy) and selenium are also protective in nature.[21,22] Recent decline in the incident of stomach cancer in many countries may be in part explained not only by higher consumption of fruit but also due to highly reduced intake of salt, preserved foods as well as the availability of refrigeration.
Five case-control studies and no cohort studies have been published from India in the last 10 years to establish specific dietary and lifestyle habits in relation to gastric cancer. The limited number of studies may be due to the difficulties in measuring the exposure by developing food frequency questionnaire and in preparing nutritional data base.
Pickled food,[23] high rice intake, spicy food, excess chilly consumption, consumption of high-temperature foods[24] smoked dried salted meat, use of soda[25] and consumption of dried salted fish[25] have emerged as significant dietary risk factors in various parts of India. These practices are prevalent in southern and eastern states of India where a higher frequency of gastric cases are also observed.
One study analyzed its dietary data based on food groups like total pulses, total meat, total fruits, total vegetables and total cereals. The results were found to be insignificant.[24] Increased association between consumption of milk and beverages containing milk showed higher risk as compared to reduced consumption but results were not statistically significant [Table 6].
Table 6
Role of dietary factors in the development of gastric cancer in India
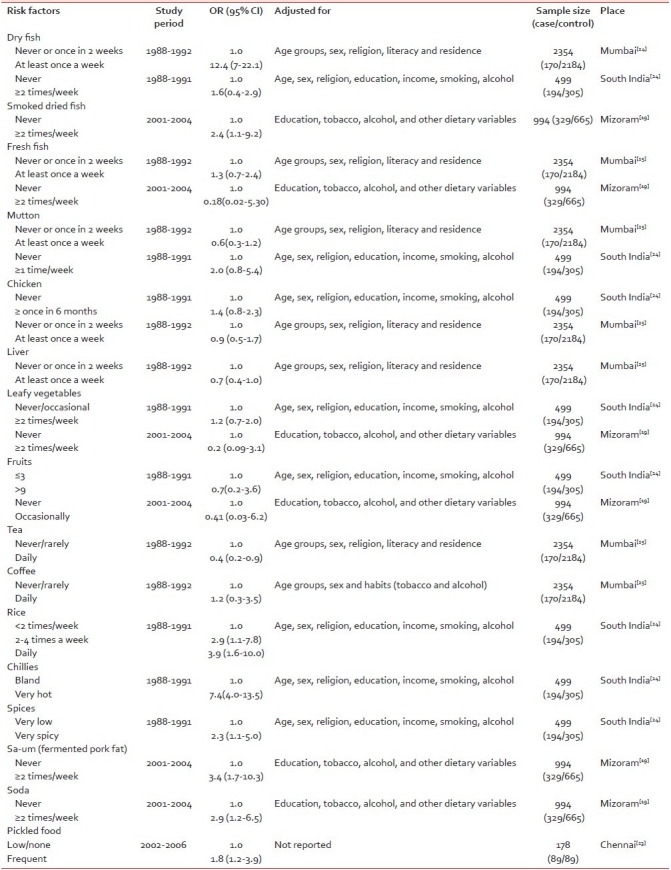
Salt intake is a risk factor for gastric carcinoma as it damages the gastric mucosa, which results in gastritis and increased cell proliferation.[26] Salted tea, a peculiar beverage, is commonly consumed by a majority of population in Kashmir valley was observed to be a risk factor.[27] Indian studies have not observed salt intake as a separate factor but salted and processed products were taken into consideration. Soda, which is an additive commonly added in the foods, was found to be associated with increased risk (OR=2.9). A protective effect of leafy vegetables and fruits was observed in these studies. Tea consumption was shown to have protective effects in one study. Reheated foods, reheated oils and refrigeration were not observed to be associated with risk of gastric cancer.[24]
The studies on diet and stomach cancer could provide breakthrough in understanding role of diet because of heterogeneous food consumption throughout India. Although the inter-individual variation might be high, the intra-individual variation is usually low. Unlike western countries where animal foods are the major part of diet and being a vegetarian is voluntary, in India the effect of lifelong vegetarianism on risk of gastric cancer could be explored.
TOBACCO AND ALCOHOL
Globally tobacco smoking has been indicated as the risk factor for gastric cancer in case-control and cohort studies.[28,29] The association between gastric cancer and tobacco smoking has been observed in various epidemiological studies [Table 7]. In India, not only tobacco smoking but also tobacco chewing is highly prevalent. Tobacco is used in various forms like, hukka, snuff, bidis, cigarettes, taibur, Meiziol, etc. About 229,392,725 adult males and 11,908,517 adult females are estimated to use tobacco in India.[28]
Table 7
Role of lifestyle-related factors in the development of gastric cancer in India
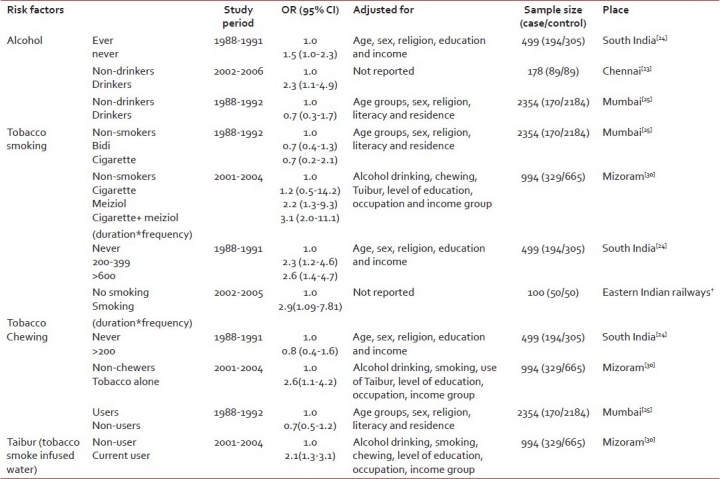
Smoking tobacco has been found to be an independent risk factor for stomach cancer.[29] Current smokers were found to be at a higher risk as compared to non-smokers and ex-smokers.[30] A significantly increased risk was observed with increased smoking in South Indian study.[24]
Increased risk was also observed among the tobacco chewers.[30] The risk showed an increasing trend with the increase in frequency and amount of tobacco use and decreasing trend with the number of years since the practice of consuming tobacco was discontinued.
Tobacco use in any form (chewing, smoking and drinking) was observed to increase the risk of stomach cancer in Mizoram, a North-eastern state of India.[30]
Literature suggest that alcohol may be carcinogenic to the esophagus and cardia cancers but not to distal gastric cancer. In a study conducted in Mumbai, alcohol intake did not emerge as a risk factor[25] for gastric cancer. In Indian context, due to social stigma attached, it is difficult to measure the alcohol intake of an individual.
Other risk factors observed by studies conducted in India are education and occupation. Case-control study conducted in Mumbai, observed that male agricultural workers had 50% excess risk (OR-1.5; 95%CI-1.1-2.6) as compared to unskilled laborers or mill workers.[25]
GENETIC SUSCEPTIBILITY
Globally literature suggest that polymorphism in genes involved in inflammation viz interleukin,[31] toll-like receptor 4,[32] hyuman leukocyte antigen,[33] metabolic phase I enzyme viz CYP1A1,[34] metabolic phase II enzyme viz GSTM1, GSTT1 (Glutathione-S-transferase)[35] and NAT1, NAT2 (N-acetyltransferase), DNA repair Viz XRCC1,[36] are involved in development of gastric cancer. Indian studies on this topic are limited because of inadequate sample size, improper study designs and inability to controls for confounders. Only small numbers of polymorphism were investigated in all these studies. Most of the Indian studies have used RFLP method for genotyping while studies conducted outside India have used Taqman and Illumina assays for genotyping.
Only six studies are reported from India on genetic polymorphism and development of gastric cancer [Table 8]. Malik et al. have found GSTM1null and CYP2E1c1c2 genotypes imparted risk for gastric cancer [OR=1.98 (95% CI=1.22-3.21) and OR=2.26 (95% CI=1.25-5.25)] in population from Kashmir valley.[37] Another study has stated that GSTT1 null genotype increases the risk of gastric cancer.[38] Prasad et al. have stated that combination of G carrier and H. pylori infection increased the risk of gastric adenocarcinoma [OR=3.504, (95% CI=1.195-7.0807)].[39] Another study from Northern India has indicated the risk of gastric adenocarcinoma was significantly higher in patients having C carrier and H. pylori infection [OR=7.06, (95% CI=2.61-19.09)].[40]
Table 8
Role of genetic susceptibility in development of gastric cancer
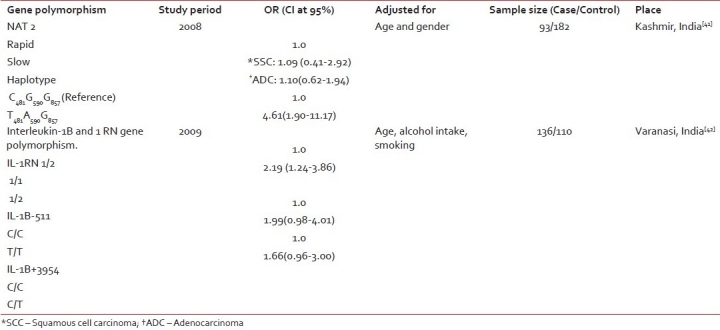
Single nucleotide polymorphism (SNP) in genes NAT2 (N-acetyltransferase),[41] interlukin-1B,[42] GSTM1 and GSTT1 (Glutathione S-transferase),[37,38] Pro12Ala peroxisome proliferator-activated receptor γ,[39] COX (cyclooxygenase)[40] have reported significant association in the development of gastric cancer.
Multiplicative interaction was observed between H. pylori infection and COX-2 polymorphism.[40] However, other studies failed to observe interaction between SNPs studied and infection with H. pylori and/or with other lifestyle factors.
PRIMARY PREVENTION
Diet and lifestyle
According to the report released by WCRF and AICR in 2007,[21] non-starchy vegetables including specific allium (particularly garlic) vegetables as well as fruits (rich sources of antioxidants) probably protect against stomach cancer. Seventeen percent decreased risk per 50 g fruits per day was observed in meta-analysis of case-control data. There is limited evidence suggesting that pulses including soya and soya products and also fruits-containing selenium protect against stomach cancer. There is limited evidence suggesting that chilly is associated with an increased risk of stomach cancer. Chilly is used to disguise “off” flavors, and thus data may be confounded by socioeconomic status, availability of refrigeration and H. pylori infection.
Salt has been shown to directly damage the stomach lining in animal trials and substantial amount of evidence from various international studies suggests that salt as well as salted foods are a probable cause of stomach cancer.
Population attributable risk for smoking among men varied between 21.5 and 28.6% and among women between 11 and 14% from the US and Europe. Thus, a reduction in tobacco consumption would bring a marked change in mortality and survival in gastric cancer.
No intervention study for dietary prevention has been reported from India in span of 1998-2008.
Primary prevention of gastric cancer by eradiating H. pylori infection is one of the alternatives proposed by some studies. The infection by H. pylori can be prevented by interrupt transmission of the infection by promoting sanitary habits,[43] good waste disposal, clean water supply and planned housing to minimize overcrowding. However, large-scale intervention trials are required to demonstrate efficiency of eradication of H. pylori infection in gastric cancer reduction in Indian perspective.
SECONDARY PREVENTION
No screening trials to observe reduction in gastric cancer mortality have been conducted in India to date. In Japan endoscopy has been tested as a screening test for gastric cancer (77.4-84% sensitivity).[44] Owing to the complications involved with endoscopy procedure and lack of large number of trained and experienced personnel who can conduct the test in field endoscopy is not considered to be an ideal tool for a population-based screening program. There is evidence from Japan about early detection and treatment of gastric cancer and finally the reduction of mortality due to the use of double contrast barium X-ray photoflurography.[45]
Serum pepsinogen is a non-invasive serological test which is being advocated for gastric cancer screening.[46] Although it makes the detection of gastric cancer easier, it can, however, detect the presence of only intestinal type of gastric cancers.
Occult Blood bead test has a specificity of 55% and a sensitivity of 65%.[47] This might also be explored for screening as it is easier to administer than endoscopy.
Mass eradication of H. pylori has been proposed as an alternative to mass screening in reducing incidence of gastric cancer. Screening young adults for H. pylori followed by treatment in those who test positive has a potential to prevent one in every 4–6 GC cases in China.[48] However, the timing of H. pylori eradication may be critical i.e., H. pylori eradication after initiation of cancer may prove unsuccessful, so medication should be administered prior to carcinogenesis (APOCP, Cancer report 2010). The data indicating the prevention of GC by H. pylori eradication needs to be critically evaluated as many conflicting results have been reported.[43] No appropriately designed RCT regarding screening has been reported in the past 10 years in India.
CONCLUSION
India has a high prevalence of H. pylori infection and comparatively low gastric cancer incidence rates. Stomach cancer is decreasing but its burden is high in India. There are limited studies from India to explain the etiology of gastric cancer. Given the high prevalence of H. pylori, trials are required to judge the potential benefit for its eradication to reduce gastric cancer. Providing medication for H. pylori eradication has to be further evaluated. More research is required not only to develop suitable screening test, but also to demarcate high-risk population and the effect of primary prevention programs. There is a need to clearly understand the risk associated with diet for any kind of prevention. Properly designed genetic susceptibility studies considering interaction with H. pylori, diet and tobacco use are required to understand etiology of gastric cancer.
As stomach cancer is one of the common cancers in India, studies are required to understand the etiology and prevention of gastric cancer.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.


 PDF
PDF  Views
Views  Share
Share

