Etiologic and epidemiologic study of hepatocellular carcinoma in West Azarbaijan of Iran (2006-2011)
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2012; 33(04): 221-223
DOI: DOI: 10.4103/0971-5851.107086
Abstract
Background: Hepatocellular carcinoma (HCC) is one of the most common cancers worldwide. Epidemiologic and etiologic studies help in the prevention of disease and improve surveillance of affected patients. The aim of this study was to study the etiology and epidemiology of HCC in West Azarbaijan of Iran. Materials and Methods: In this cross-sectional, retrospective study, medical records of 60 patients with HCC who were diagnosed between 2006 and 2011 in West Azarbaijan of Iran were analyzed for age, sex, location, presence of liver cirrhosis and/or well-known risk factors of HCC. Data were analyzed by SPSS 17 software. Results: From 60 patients with HCC, 75% were male and 25% were female. Mean age of the patients was 63.47 years. 51.66% were from rural areas and 48.33% were from urban areas. 43.33% of HCC patients were cirrhotic while 56.66% patients were non-cirrhotic. Of the 26 cirrhotic patients, 57.69% were seropositive for hepatitis B surface antigen (HBsAg), 15.38% not only had history of excess alcohol intake but were also HBsAg positive, 3.84% had history of alcoholism, 3.84% had history of Wilson disease and the rest (19.24%) had cryptogenic cirrhosis. Of the 34 non-cirrhotic patients, 35.29% were positive for HBsAg. None of the 60 patients with HCC had positive serology for hepatitis C virus (HCV) or history of hepatitis C infection. Conclusion: In our study, most of the patients (>50%) with HCC did not have underlying liver cirrhosis. In the cirrhotic patients, hepatitis B infection was the most common predisposing factor, followed by hepatitis B infection concomitant with alcoholism, alcoholism alone and Wilson disease. In the remaining cirrhotic patients, we could not find any predisposing factor for cirrhosis. Infection with HCV was not found in our studied group. We concluded that etiology of HCC in our province is different from that in the western countries.
Publication History
Article published online:
20 July 2021
© 2012. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Background:
Hepatocellular carcinoma (HCC) is one of the most common cancers worldwide. Epidemiologic and etiologic studies help in the prevention of disease and improve surveillance of affected patients. The aim of this study was to study the etiology and epidemiology of HCC in West Azarbaijan of Iran.
Materials and Methods:
In this cross-sectional, retrospective study, medical records of 60 patients with HCC who were diagnosed between 2006 and 2011 in West Azarbaijan of Iran were analyzed for age, sex, location, presence of liver cirrhosis and/or well-known risk factors of HCC. Data were analyzed by SPSS 17 software.
Results:
From 60 patients with HCC, 75% were male and 25% were female. Mean age of the patients was 63.47 years. 51.66% were from rural areas and 48.33% were from urban areas. 43.33% of HCC patients were cirrhotic while 56.66% patients were non-cirrhotic. Of the 26 cirrhotic patients, 57.69% were seropositive for hepatitis B surface antigen (HBsAg), 15.38% not only had history of excess alcohol intake but were also HBsAg positive, 3.84% had history of alcoholism, 3.84% had history of Wilson disease and the rest (19.24%) had cryptogenic cirrhosis. Of the 34 non-cirrhotic patients, 35.29% were positive for HBsAg. None of the 60 patients with HCC had positive serology for hepatitis C virus (HCV) or history of hepatitis C infection.
Conclusion:
In our study, most of the patients (>50%) with HCC did not have underlying liver cirrhosis. In the cirrhotic patients, hepatitis B infection was the most common predisposing factor, followed by hepatitis B infection concomitant with alcoholism, alcoholism alone and Wilson disease. In the remaining cirrhotic patients, we could not find any predisposing factor for cirrhosis. Infection with HCV was not found in our studied group. We concluded that etiology of HCC in our province is different from that in the western countries.
INTRODUCTION
Hepatocellular carcinoma (HCC) is the fifth most common cancer and the second cause of cancer-related death of males.[1,2]
In females, HCC is the seventh most common cancer and the sixth cause of cancer-related death.[2] Eighty percent of patients with HCC have underlying chronic hepatitis B or C infection.[3] HCC distribution is different among regions of a country due to difference in exposure to hepatitis viruses and environmental pathogens.[4] The HCC rate is higher in men than in women, with a 2:1 predominancy. Explanation for this male dominancy is that males have a higher possibility of being infected with hepatitis B virus (HBV) and hepatitis C virus (HCV), alcohol intake , smoking and hemochromatosis and have higher levels of androgenic hormones.[5–7] Most cases of HCC are due to viral hepatitis (B and C) or cirrhosis.[8] Etiology of HCC in patients with and without cirrhosis is different.[9–12]
Of the important predisposing factors of HCC in western countries, which included HBV, HCV and alcohol, only HBV seems to directly lead to liver cell transformation.[13]
Other risk factors of HCC included excessive alcohol consumption, aflatoxin intake, nonalcoholic steatohepatitis (NASH) and hereditary hemochromatosis.[14]
MATERIALS AND METHODS
In this cross-sectional, retrospective study, medical records of 60 patients with HCC who were diagnosed between 2006 and 2011 in the Imam Khomeini Hospital of Urmia City were analyzed for age, sex, living in a city or village, smoking, presence of liver cirrhosis and/or known risk factors of HCC. Data were analyzed by SPSS software. Diagnosis of HCC had been made in 50 patients with live biopsy and in the remaining 10 patients with solitary or multiple liver masses in abdominal imaging (size >2 cm) and markedly elevated alfa-fetoprotein (more than 500 ng/ mL). Cirrhosis was defined by typical view of liver in sonography, prolonged prothrombin time (PT) and presence of ascites.
RESULTS
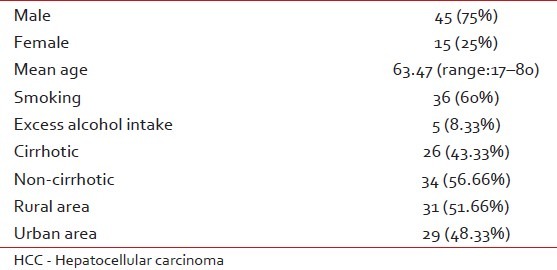
Of 60 patients with HCC, 75% (n=45) were male and 25% were female (n=15). Mean age of the patients was 63.47 years (range: 17–80 years). Mean age for females was 60.2 years (range: 20–80 years) and mean age for males was 66.75 years (range: 17–80 years). 51.66% (n=31) were from rural areas and 48.33% (n=29) were from urban areas. Sixty percent (n=36) of the patients had a history of smoking. 43.33% (n=26) of the patients were cirrhotic while 34 patients (56.66%) were non-cirrhotic [Table 1].
Table 1
Clinical data of 60 patients with HCC
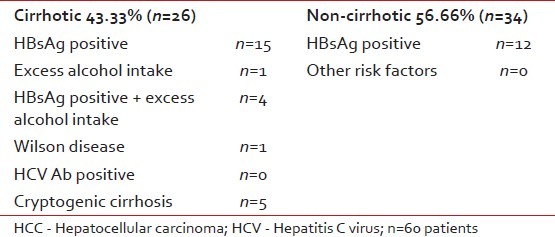
Of the 26 cirrhotic patients, 57.69% (n=15) had positive hepatitis B surface antigen (HBsAg), 15.38% (n=4) had HBs antigenemia combined with history of excess alcohol intake, 3.84% (n=1) had history of excess alcohol consumption, 3.84% (n=1) had history of Wilson disease and 19.24% (n=5) had cryptogenic cirrhosis. Of the 34 non-cirrhotic patients, 35.29% (n=12) were positive for HBsAg. None of the 60 patients with HCC had positive serology for HCV or history of hepatitis C infection [Table 2]. In our study, most of the patients (>50%) with HCC had no underlying liver cirrhosis. Of the cirrhotic patients (n=26), hepatitis B infection, alcoholism and Wilson disease were the causative agents and in 19.20% (n=4), we could not find any etiology of cirrhosis. Infection with HCV was not found in our studied group. We concluded that etiology of HCC in our province (West Azarbaijan of Iran) is different from that of other western countries.
Table 2
Risk factors for HCC in our studied group
DISCUSSION
Goetze et al. from eastern Germany studied 640 patients with HCC. In their study, 223 of the patients (83.5%) had liver cirrhosis. Alcohol-induced chronic liver disease followed by hepatitis C infection, NASH, hepatitis B infection, cryptogenic liver cirrhosis, alcohol in combination with viral hepatitis, hemochromatosis and hepatitis B and C coinfection were the causative agents of HCC.[14]
Chiesa et al. from Italy studied 174 patients with newly diagnosed HCC. They found liver cirrhosis in 142 cases, excluded in 21 cases and remained undefined in 11 cases. They showed that most HCC cases are due to HBV, HCV or alcohol intake in both the presence and the absence of cirrhosis.[15]
Iqbal et al. from north of Pakistan studied 100 patients with HCC. Seventy-four percent of them were HCV positive, 13% were HBsAg positive, 4% patients were HCV and HBsAg positive and in the remaining 9%, no predisposing cause was found. Eighty percent of them were cirrhotic.[16]
Uzunalimoğlu et al. from Turkey studied 207 patients with HCC; they concluded that HBV infection is the highest leading cause of HCC in Turkey, followed by hepatitis C infection and alcoholic liver disease.[17]
A metaanalysis was performed on 27,881 HCC patients for seroprevalence of HBsAg and HCV Ab from 90 studies. A predominancy for HBsAg was found in HCC patients from Asian, African and Latin American countries, but anti-HCV dominancy was found in Europe, North America, Japan, Pakistan, Mongolia and Egypt. Anti-HCV was found to be higher than HBsAg in Europe and in the United States.[18]
In this study, we found that most of the patients with HCC did not have hepatitis B and none of them had HCV infection; thus, it seems likely that high dietary exposure with aflatoxin and other environmental factors and toxins are possible predisposing factors for HCC. Aflatoxin was found in mouldy peanuts, wheat, soya beans, corn and rice; thus, we recommend searching for aflatoxin in these foods in West Azarbaijan of Iran. Giving information to people for proper care of crops and foods’ storage can prevent from HCC in this province of Iran.
ACKNOWLEDGMENT
This work is a result from a thesis which was supported by Urmia University of Medical Sciences. Our special thank to staff of Imam Khomeini hospital that helped us in providing medical records of patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.


 PDF
PDF  Views
Views  Share
Share

