Extrapulmonary Tuberculosis of Lymph Node Coexist with Diffuse Large B cell Lymphoma: A Case Report
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2017; 38(03): 391-393
DOI: DOI: 10.4103/ijmpo.ijmpo_164_16
Abstract
Extrapulmonary tuberculosis (TB) coexistent with lymphomas in the same organ are rare. Here, we report a case of a 14-year-old male patient who had cauliflower-like ulcerated mass over cervical lymphadenopathy. He was diagnosed extrapulmonary TB. Unresponsiveness of anti tubercular treatment (anti-tubercular) treatment after 6 months, he was diagnosed as diffuse large B-cell lymphoma.
Publication History
Article published online:
04 July 2021
© 2017. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Extrapulmonary tuberculosis (TB) coexistent with lymphomas in the same organ are rare. Here, we report a case of a 14-year-old male patient who had cauliflower-like ulcerated mass over cervical lymphadenopathy. He was diagnosed extrapulmonary TB. Unresponsiveness of anti tubercular treatment (anti-tubercular) treatment after 6 months, he was diagnosed as diffuse large B-cell lymphoma.
Introduction
Tuberculosis (TB) and malignancy represent global threats claiming millions of lives and inflicting formidable suffering worldwide. Surprisingly, the pathophysiological and practical implications of their coexistence have received little attention.[1] It has been reported that the risk of non-Hodgkin lymphoma (NHL) is significantly increased (odds ratio 1.8) in individuals with a history of TB.[2] Extrapulmonary TB coexistent with lymphomas in the same organ are rare.[3] Here, we report a case of a 14-year-old male who had cauliflower-like ulcerated mass over cervical lymphadenopathy. He was diagnosed extrapulmonary TB earlier. Due to unresponsiveness of ATT after 6 months, he was diagnosed as diffuse large B-cell lymphoma (DLBCL).
Case Report
A 14-year-old male patient came to our department with a huge cauliflower-like progressive ulcerated neck mass and bilateral axillary lymphadenopathy for 8 months with grade intermittent fever, weight loss, and fatigue for the past 4 months.
Eight months before, he was diagnosed tubercular lymphadenitis by fine-needle aspiration cytology (FNAC) and given ATT (anti-TB treatment) for the past 6 months. After complete the anti-tubercular drug (ATD), the neck mass was again progressively increased with bilateral axillary lymphadenopathy. Patient also complained low fever, loss of appetite, weight loss, and night sweat. After 1 month, he came to our outpatient department.
In our department, the physical examination revealed a bulky ulcerative cauliflower-like diffuse anterior neck mass measuring 8 cm × 8 cm involving the submental and anterior cervical region and bilateral axillary lymphadenopathy measuring 3 cm × 2 cm each [Figure 1a and andb].b]. FNAC from the solid area of ulcerated neck mass and axillary lymph node were done, and the cytosmear revealed sparse large atypical lymphoid cells over a background of necrosis and acute inflammatory cells. Thus, the diagnosis was suspicion of NHL [Figure 1c]. His routine blood examination was normal except for increased erythrocyte sedimentation rate and neutrophilic leukocytosis with left shift. Serological test such are HIV, hepatitis B surface antigen, and HIV were negative. X-ray and ultrasonography abdomen and pelvis findings were unremarkable. Computed tomography scan of the neck showed cervical lymphadenopathy with central necrosis. Punch biopsy from the ulcerated mass was done and histopathology section showed the presence of atypical lymphoid cells characterized by large cells with round morphology. Some amount of eosinophilic cytoplasm, fine chromatin, and prominent central nucleoli scattered over a loose fibro-collagenous stroma. Some cells had plasmacytoid morphology. There were areas of dense neutrophillic aggregation and necrosis. The diagnosis was given as DLBCL [Figure 1d]. Immunehistochemistry reports revealed the tumor cells are CD20 and negative for Alk-1 and CD30. The final diagnosis was concluded as DLBCL. Peripheral smear and bone marrow aspiration cytology did not show the presence of any atypical lymphoid cells.
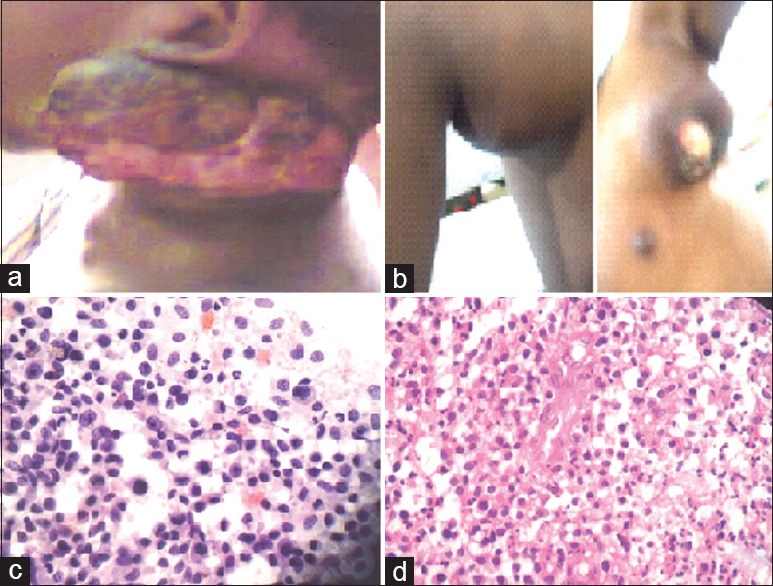
| Figure 1:(a and b) A bulky ulcerative cauliflower-like diffuse anterior neck mass measuring 8 cm × 8 cm involving the submental and anterior cervical region and bilateral axillary lymphadenopathy measuring 3 cm × 2 cm each. (c) Sparse large atypical lymphoid cells over a background of necrosis and acute inflammatory cells. (d) Atypical lymphoid cells some amount of eosinophilic cytoplasm, fine chromatin and prominent central nucleoli scattered over a loose fibro collagenous stroma. Plasmacytoid morphology
Discussion
Nowadays, research for carcinogenesis is expanding and the possible correlation between chronic inflammation and cancer development is slowly being unraveled. Therefore, history of TB infection has been examined as a risk factor for cancer. However, one study stated that previous TB history was merely coincidental with the occurrence of cancer. Although TB and cancer are very common diseases, there has been little attention to the pathophysiological and practical implications of their coexistence.[1]
NHL may be preceded by chronic inflammatory diseases and furthermore has been related to immune deficiency.[4]
NHL in many conditions has been found to be preceded by chronic inflammatory diseases. Association of Helicobacter pylori, campylobacter and hepatitis C virus with NHL has already been well established. However till date, there is no evidence that Mycobacterium tuberculosis predisposes to NHL. Surprisingly, TB did not response till NHL was taken care of, which is difficult to explain. TB is affected by cell-mediated immunity (T-cells) mainly, whereas DLBCL is primarily a B-cell neoplasm. Although combination of TB lymphadenitis and Hodgkin's lymphoma has been reported, the combination of TB lymphadenitis and NHL has not been signaled in the current literature.[5] Extrapulmonary TB coexistent with lymphomas in the same organ are rare.[3]
Geographic location also appears to have an impact on the concurrent appearance of both pathologies.[4]
In resource-poor countries, like India which is located in TB-endemic zone, all cases of cervical lymphadenopathy are conventionally considered a tuberculous etiology, unless proved otherwise, as tubercle bacilli are the most common offending agent of cervical lymphadenopathy.[6] In India, both TB and NHL are common, but simultaneous occurrence of the diseases has rarely been reported.[5]
Conventionally, excision biopsy is done to diagnose tuberculous lymphadenitis but FNAC, a relatively less invasive, painless, and outdoor procedure, seems to have established itself as a safe, cheap, and reliable procedure.[7]
However, it should be kept in mind that there are many other etiologies of cervical lymphadenopathy (although rarer than TB), especially in cases of nonresponders and where inconclusive cytological picture in the absence of strong supportive clinical evidences of TB is the basis of initial advice of ATDs. In such cases, close monitoring of the patients is mandatory and excision biopsy should be done before starting ATT, if facilities are available. Otherwise, this type of invasive procedure may be avoided in the first visit.[6]
It is difficult to differentiate TB and lymphoma on clinical ground only, especially when FNAC is totally inconclusive. In pulmonary TB, there is option for sputum examination for acid-fast bacilli and mycobacterial culture, but in the extra-pulmonary cases, like lymphnode TB, microbiological proof is difficult to obtain.[6]
In a recent report, three patients with a presumed diagnosis of TB on clinical grounds (without bacteriological confirmation) were eventually diagnosed with a Hodgkin disease in two cases, and with a DLBCL in the other case.[2]
Majority of TB lymphadenitis respond to anti-TB therapy (ATT). However, new lymph nodes may appear, or existing lymph nodes may increase in size during treatment in immune-suppressed as well as immunecompetent patients. The most important cause of unresponsive lymphadenopathy is infection caused by atypical or drug-resistant mycobacteria. However, rarely simultaneously double pathology of lymph node may be responsible for unresponsiveness to ATT extremely diverse pathology.[5]
Conclusion
We concluded that when the lymphadenopathy is not responding to the adequate regimen of ATD, excision biopsy should be considered without hesitation. In addition, further research is required to determine if a tuberculous infection, being similar to other chronic infections and inflammatory conditions, may facilitate carcinogenesis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Falagas ME, Kouranos VD, Athanassa Z, Kopterides P. Tuberculosis and malignancy. QJM 2010;103:461-87.
- Dres M, Demoule A, Schmidt M, Similowski T. Tuberculosis hiding a non-Hodgkin lymphoma “there may be more to this than meets the eye”. Respir Med Case Rep 2012;7:15-6.
- Sachdev R, Duggal R, Agrawal K, Goel S. Coexistent nodal diffuse large B-cell lymphoma with extrapulmonary tuberculosis: A rare case. Int J Surg Pathol 2016;24:70-2.
- Fanourgiakis P, Mylona E, Androulakis II, Eftychiou C, Vryonis E, Georgala A, et al. Non-Hodgkin's lymphoma and tuberculosis coexistence in the same organs: A report of two cases. Postgrad Med J 2008;84:276-7.
- Mandal PK, Sarkar S, Ghosh MK, Bhattacharyya M. Simultaneous dual pathology in lymph node. Mediterr J Hematol Infect Dis 2014;6:e2014036.
- Pandit S, Choudhury S, Das A, Das SK, Bhattacharya S. Cervical lymphadenopathy – Pitfalls of blind antitubercular treatment. J Health Popul Nutr 2014;32:155-9.
- Gupta PR. Difficulties in managing lymph node tuberculosis. Lung India 2004;21:50-3.
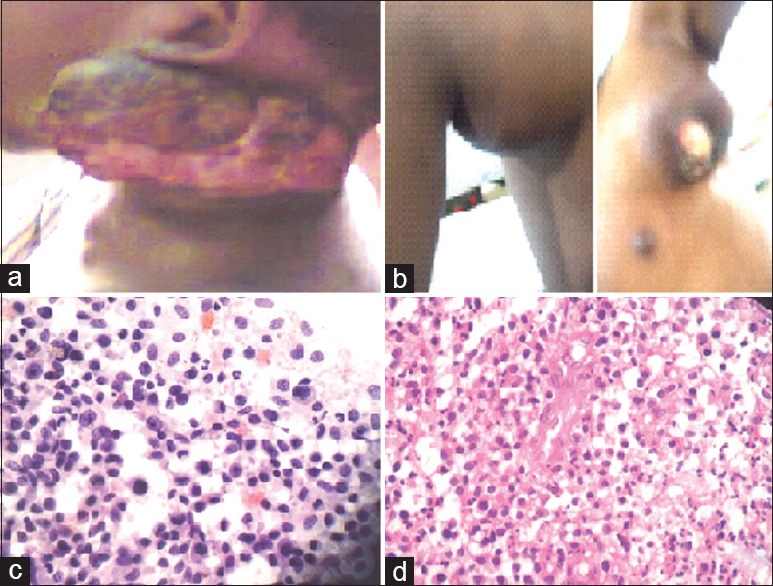
| Figure 1:(a and b) A bulky ulcerative cauliflower-like diffuse anterior neck mass measuring 8 cm × 8 cm involving the submental and anterior cervical region and bilateral axillary lymphadenopathy measuring 3 cm × 2 cm each. (c) Sparse large atypical lymphoid cells over a background of necrosis and acute inflammatory cells. (d) Atypical lymphoid cells some amount of eosinophilic cytoplasm, fine chromatin and prominent central nucleoli scattered over a loose fibro collagenous stroma. Plasmacytoid morphology
References
- Falagas ME, Kouranos VD, Athanassa Z, Kopterides P. Tuberculosis and malignancy. QJM 2010;103:461-87.
- Dres M, Demoule A, Schmidt M, Similowski T. Tuberculosis hiding a non-Hodgkin lymphoma “there may be more to this than meets the eye”. Respir Med Case Rep 2012;7:15-6.
- Sachdev R, Duggal R, Agrawal K, Goel S. Coexistent nodal diffuse large B-cell lymphoma with extrapulmonary tuberculosis: A rare case. Int J Surg Pathol 2016;24:70-2.
- Fanourgiakis P, Mylona E, Androulakis II, Eftychiou C, Vryonis E, Georgala A, et al. Non-Hodgkin's lymphoma and tuberculosis coexistence in the same organs: A report of two cases. Postgrad Med J 2008;84:276-7.
- Mandal PK, Sarkar S, Ghosh MK, Bhattacharyya M. Simultaneous dual pathology in lymph node. Mediterr J Hematol Infect Dis 2014;6:e2014036.
- Pandit S, Choudhury S, Das A, Das SK, Bhattacharya S. Cervical lymphadenopathy – Pitfalls of blind antitubercular treatment. J Health Popul Nutr 2014;32:155-9.
- Gupta PR. Difficulties in managing lymph node tuberculosis. Lung India 2004;21:50-3.


 PDF
PDF  Views
Views  Share
Share

