Hodgkin lymphoma: A clinicopathological and immunophenotypic study
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2016; 37(01): 59-65
DOI: DOI: 10.4103/0971-5851.177038
Abstract
Introduction: The diagnosis of Hodgkin lymphoma (HL) is defined in terms of its microscopic appearance (histology) and the expression of cell surface markers (immunophenotype). Aims and objectives: This study aims to analyze the clinical features, histomorphology, and immunoprofile of over 200 patients of HL diagnosed over a period of 4 years at our institute and to determine relative frequency of various histological subtypes (based on WHO classification) in relation to age and sex distribution in this part of the country. Materials and Methods: All HL cases diagnosed between January 2006 and December 2009 were retrieved from hospital records. The histopathology of both lymph node and bone marrow biopsy (where ever available) along with immunohistochemistry (CD15, CD30, CD20, and ALK) were reviewed. Results: There was a bimodal age distribution. HL affected people a decade earlier than in the western population. The most common presenting complaint was cervical lymphadenopathy. Mixed cellularity was the most frequent subtype (67%), followed by nodular sclerosing subtype (23.5%). Group A (CD15+, CD30+, CD20−), which represents the archetypical immunophenotype of classical HL (CHL) was the most common type (60.6%). The number of CD15 negative CHL was 35.8% and CD20 positive CHL was 17.5%. CD15 negativity with CD20 positivity was seen in 5% CHL. One out of seven CD20 positive CHL patients showed relapse. Conclusion: In this paper, we have discussed in detail about various clinical and histopathological parameters of HL and their relative frequency in various histological subtypes. This paper is being presented as it is a rather large study from India taking into consideration the clinical, pathologic, and immunophenotypic profile of the patients.
Publication History
Article published online:
12 July 2021
© 2016. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Introduction:
The diagnosis of Hodgkin lymphoma (HL) is defined in terms of its microscopic appearance (histology) and the expression of cell surface markers (immunophenotype).
Aims and objectives:
This study aims to analyze the clinical features, histomorphology, and immunoprofile of over 200 patients of HL diagnosed over a period of 4 years at our institute and to determine relative frequency of various histological subtypes (based on WHO classification) in relation to age and sex distribution in this part of the country.
Materials and Methods:
All HL cases diagnosed between January 2006 and December 2009 were retrieved from hospital records. The histopathology of both lymph node and bone marrow biopsy (where ever available) along with immunohistochemistry (CD15, CD30, CD20, and ALK) were reviewed.
Results:
There was a bimodal age distribution. HL affected people a decade earlier than in the western population. The most common presenting complaint was cervical lymphadenopathy. Mixed cellularity was the most frequent subtype (67%), followed by nodular sclerosing subtype (23.5%). Group A (CD15+, CD30+, CD20−), which represents the archetypical immunophenotype of classical HL (CHL) was the most common type (60.6%). The number of CD15 negative CHL was 35.8% and CD20 positive CHL was 17.5%. CD15 negativity with CD20 positivity was seen in 5% CHL. One out of seven CD20 positive CHL patients showed relapse.
Conclusion:
In this paper, we have discussed in detail about various clinical and histopathological parameters of HL and their relative frequency in various histological subtypes. This paper is being presented as it is a rather large study from India taking into consideration the clinical, pathologic, and immunophenotypic profile of the patients.
INTRODUCTION
The diagnosis of Hodgkin lymphoma (HL) is defined in terms of its microscopic appearance and the expression of cell surface markers. Various approaches in the histological classification of HL have been developed to predict prognosis on a histomorphological basis. However, the literature available on the significance of different histological features in the diagnosis as well as on the prognosis of HL is inadequate, especially in the Indian context. The clinical features and morphological patterns vary from country to country.
Aims and objectives
This study aims to analyze the clinical features, histomorphology, and immunoprofile of over 200 patients of HLs diagnosed over a period of 4 years at our institute and to determine the relative frequency of various histological subtypes (based on WHO classification) in relation to age and sex distribution in this part of the country. We also compared the immunoprofile of HRS cells with other studies.
MATERIALS AND METHODS
All patients diagnosed as HL between January 2006 and December 2009 were included in the study. The clinical features and other laboratory parameters were obtained from the hospital records.
Paraffin sections were reviewed. Hematoxylin and eosin stain (HE) was used to study the basic morphology. The histopathology of both lymph node biopsy and bone marrow biopsy (where ever available) and immunohistochemistry (IHC) were reviewed. A total of 233 patients were retrieved from histopathology and hematopathology files.
Lymph node biopsy
All tissues for histological evaluation were fixed in 10% neutral buffered formalin and routinely prepared for HE staining. The tissue sections were stained with HE stain and Reticulin stain and if necessary Masson's trichrome.
IHC with CD15, CD30, CD20, CD3, CD45, epithelial membrane antigen, and ALK were done where ever necessary. The IHC was performed using Dako monoclonal antibodies by horseradish peroxidase polymer technique.
The following histologic parameters were studied
Architecture of the lymph node: It was marked as total diffuse or partial effacement of the architecture. Other than these two, nodular pattern was also observed.
Composition of background infiltrate: The presence of neutrophils, eosinophils, plasma cells, and lymphocytes were noted.
Fibrosis: It was graded according to the density as mild, moderate, and severe. Wherever possible, Reticulin stain was used to highlight the fibrosis.
Capsule: Whether thickened or not.
Histological grading system was applied for nodular sclerosing HL[1] using the following criteria:
- Sclerotic bands within the lymph node.
- Cohesive clusters or sheets of Hodgkin/reed Sternberg (H/RS) cells.
- Tissue infiltration by neutrophils.
- Coagulative necrosis.
- Morphologic atypia of the H/RS cells.
- The relative amount of lymphocytes.
- Tissue infiltration by eosinophils.
- Immunoprofile of CD15, CD30 and CD20 were studied.
RESULTS
There were a total of 233 patients of HL over a period of 4 years (between 2006 and 2009). After excluding patients with incomplete details and which were reviewed after IHC as NHL, a total of 195 patients were included in the study.
Table 1 shows the age and sex distribution. There was a bimodal age distribution. The first peak was between 6 and 10 years, and second peak between 26 and 30 years, the mean age was 28.7 years. There was male preponderance with male:female ratio of 2.6:1.
Table 1
Age and sex distribution (n = 195)
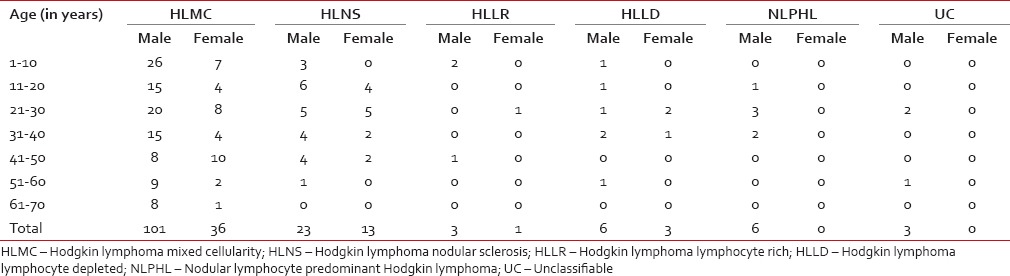
Mixed cellularity was the most frequent subtype (67%), followed by nodular sclerosing subtype (23.5%). Table 1 shows the distribution of various types of HL. There was male preponderance in both types of HL, (classical HL [CHL] - 69.3%, and nodular lymphocyte predominant Hodgkin lymphoma [NLPHL] - 100%) and all the subtypes of CHL (Hodgkin lymphoma mixed cellularity [HLMC] - 74.2%, Hodgkin lymphoma nodular sclerosis [HLNS] - 63.8%, Hodgkin lymphoma lymphocyte rich [HLLR] and Hodgkin lymphoma lymphocyte depleted [HLLD] - 66.6%).
Most common presenting complaint was cervical lymphadenopathy (lap) followed by generalized lymphadenopathy. The other manifestations were inguinal lymphadenopathy, axillary lymphadenopathy, and abdominal mass. Various B symptoms include fever, loss of weight, and appetite. Various other associated symptoms and signs were pain - 8 (6.1%), pruritus - 5 (3.8%), menstrual irregularity - 4 (out of 53 women) (7.5%), pallor - 8 (6.1%), icterus - 2 (1.5%), and edema - 3 (2.3%).
Lymph node groups involved
Isolated cervical group of lymph node involvement was the most common pattern of involvement seen in 19.48% of patients (38/195). Cervical lymph nodes were the most common group of lymph nodes to be involved either singly or along with other group of nodes in all histological subtypes (114 out of 195 patients). The most common histological subtype in all groups was HLMC, followed HLNS.
In HLMC subtype, the most common lymph node group involved was cervical (80/137 [58.3%]) followed by abdominal (42/137 [30.6%]), axillary (39/137 [28.4%]), inguinal (29/137 [(21.1%]), and mediastinal (29/137 [21.1%]).
In HLNS subtype, the most common lymph node group involved was cervical (22/36 [61.1%]) followed by axillary (11/36 [30.5%]), mediastinal (10/36 [27.7%]), abdominal (9/36 [25%]), and inguinal (5/36 [13.8%]).
In HLLD subtype, the most common lymph node group involved was cervical (4/9 [44.4%]) followed by inguinal (3/9 [33.3%]) and abdominal (3/9 [33.3%]).
In HLLR subtype, the most common lymph node group involved was cervical (3/4 [75%]) followed by axillary (2/4 [50%]).
In NLPHL subtype, the most common lymph node group involved was cervical (4/6 [66.6%]), followed by axillary (2/6 [33.3%]), abdominal (2/6 [33.3%]), and mediastinal (1/6 [16.6%]).
Hepatosplenomegaly
Hepatomegaly was present in 20 patients and splenomegaly was in 28 patients. One patient had splenectomy other extranodal sites involved were bone marrow, lung, (14 and 9 patients respectively) kidney, skin, and mandible (one case each).
Socioeconomic status
Socioeconomic status (SE) was known for 76 patients. They were classified into low middle and higher economic status depending on the occupation, income, and educational status. There was a slight prominence of HLMC in lower SE group (50.9%) than higher SE group whereas HLNS was more common in middle SE group (58.3%).
Bone marrow
As part of staging work-up, bone marrow study was done in 74 patients. Marrow involvement was seen in 14 patients.
Immunophenotyping
IHC was done in 155 patients. Reed Sternberg (RS) cells showed membrane and Golgi region positivity with both CD15 and CD30 in 93 patients. CD30 was positive in 93.5% of patients of CHL (145/155) and negative in all patients of NLPHL. CD15 was positive in 60.6% of patients of CHL, and negative in all patients of NLPHL. CD20 was positive in all patients of NLPHL and 7 patients of CHL (17.5%; 7/40) (3 patients of HLNS, and 4 patients of HLMC). However, CD20 was negative in HLLD and HLLR variants of CHL. Of the 7 patients of CHL with CD20 positivity, one patient developed relapse during the 5 years follow-up period (1/7, 14.2%). CD15 negativity with CD20 positivity was seen in 5% patients of otherwise typical CHL.
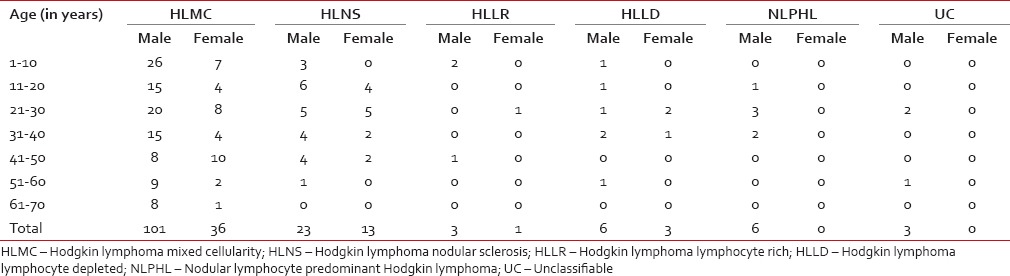
The patients were divided into six immunophenotypic groups; Group A (CD15+, CD30+, CD20−), Group B (CD15−, CD30+, CD20−), Group C (CD15+, CD30+, CD20+), Group D (CD15−, CD30+, CD20+) and Group E (CD15−, CD30−, CD20+), Group F (CD30−, CD20−, CD15+) as described by von Wasielewski et al[2] shown in Table 2.
Table 2
Immunohistochemistry patterns (n = 155)
Histological features
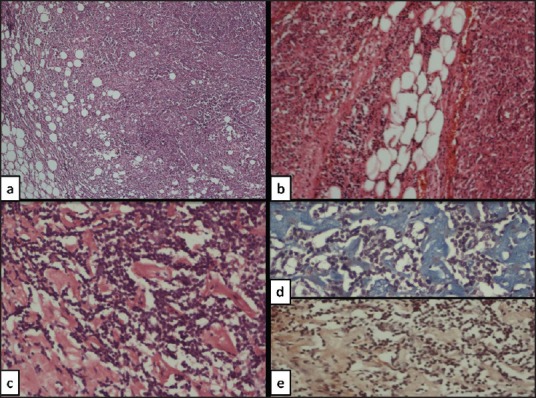
Various histological parameters analyzed and there relative frequency in various histological subtypes is detailed in Table 3. The classification of histologic subtypes was made as per WHO guidelines.[3] The histological features and IHC profile are depicted in Figures Figures11 and and22 respectively.
Table 3
Histological parameters
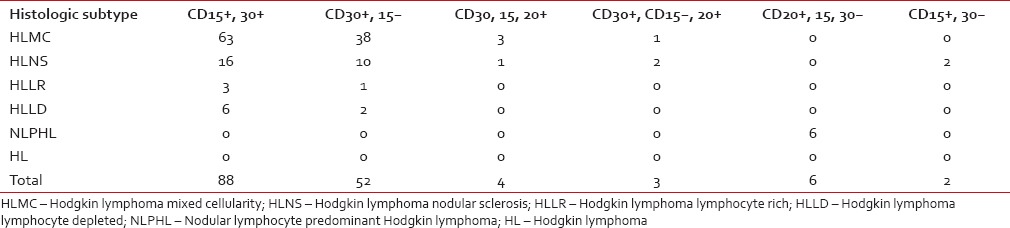
| Fig. 1 Various histological parameters studied (H and E): (a and b) Extracapsular infiltration (×100) (c-e) paraamyloid (d) Masson trichrome, (e) Congo red ×400
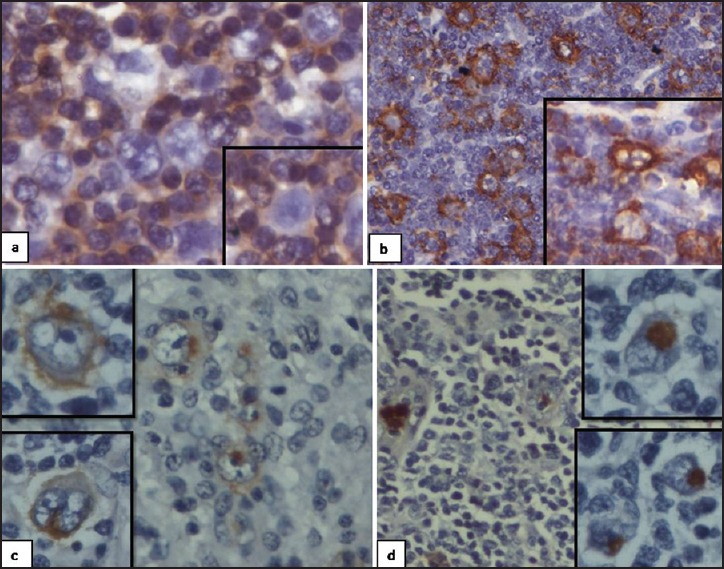
| Fig. 2 Immunohistochemistry (a) CD3 – positive in T lymphocytes forming rosettes around Reed Sternberg cells which is negative for CD3 (b) CD20 – positive in Reed Sternberg cells and B lymphocytes (c) CD 15 – positive in myeloid precursors and Reed Sternberg cells (Golgi and membrane positivity) (d) CD30 positive in Reed Sternberg cells (Golgi and membrane positivity)
Capsule
In cases where the capsule was not included in the sections and in core biopsies, it was denoted as absent capsule. Capsular thickening was most frequent in HLNS subtype. In HLMC, HLLD, and NLPHL subtypes, capsular thickening was less common.
Extra capsular invasion
Extra capsular invasion was seen in 4.6% (9/195) of patients.
Complete effacement of architecture was more frequent than partial effacement in all the subtypes.
Fibrous bands were seen in all patients of HLNS and 5.1% patients of HLMC. However, the presence of Lacunar cells was taken as the diagnostic criterion to classify it as HLNS in addition to the presence of fibrous bands.
Nodule formation was seen in all patients (100%) of HLNS and NLPHL; however, the nodules of HLNS were surrounded by fibrous bands. Nodule formation was also seen occasionally in HLMC and HLLD (3.6% and 11.1%, respectively).
Background fibrosis/hyalinization was seen in all patients of HLNS, and rarely in HLMC and HLLD subtypes.
Necrosis was seen in 8.7% (17/195) of patients, even without history of prior therapy.
In addition to these, other histological findings noted less frequently were para-amyloid (3.5% [7/195]), granulomas (5.6% [11/195]), and frequent mitotic figures (5.6% [11/195]).
Hodgkin lymphoma nodular sclerosis
Various parameters described by von Wasielewski et al.[1] were analyzed in all cases diagnosed as HLNS. Sclerotic thickening of lymph node capsule was noted in 28 cases, sclerotic bands within the lymph node were seen in 36 cases, total involvement of the lymph node by neoplastic and inflammatory cells were seen in 35 cases and partial in one case, cohesive clusters or sheets of H/RS cells were seen in 2 cases, tissue infiltration by neutrophils were seen in 10 cases, coagulative necrosis was seen in 4 cases, morphologic atypia of the H/RS cells was seen in one case, and tissue infiltration by eosinophils were present in 28 cases out of total 36 cases studied.
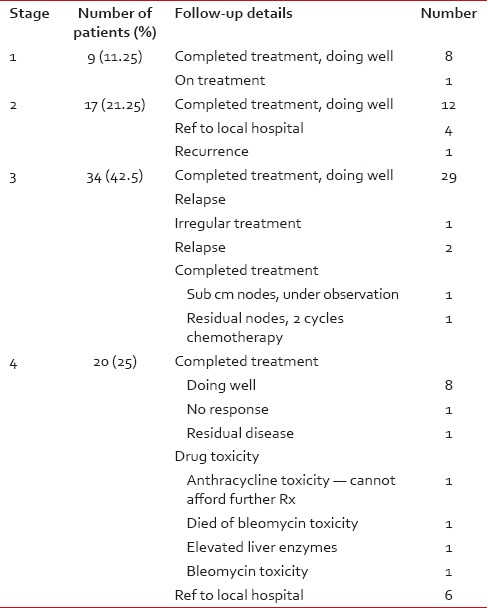
Clinical stage and treatment details
Clinical stage was known in 80 patients. Most of the patients were of Stage 3 (42.5%, 34/80), followed by Stage 4 (25%, 20/80), Stage 2 (21.25%, 17/80), and Stage 1 (11.25%, 9/80).
Treatment details were available for 100 patients. Most of these patients (99/100) were treated with doxorubicin, bleomycin, vinblastine, and dacarbazine regimen with a median number of four cycles, expect one patient who was given CHOP regimen. Of these, 12 patients were given local radiotherapy in addition to chemotherapy. The follow-up period ranged between 4 years and 6 months with median of 2 years.
Most frequent complication observed during the course of treatment was bleomycin toxicity, which was seen in 4 cases. Other complications such as anthracycline toxicity, pharyngitis, acute renal failure, and elevated liver enzymes, in one case each. Tuberculosis, chicken pox, and Pneumocystis pneumonia were seen in one case each.
Death (2/100) was mainly due to drug complications. Two patients died during the course of treatment, one patient died of renal failure and other patient died of respiratory arrest following bleomycin toxicity.
Residual disease after treatment was seen in 3% (3/100) of patients, of which 2 patients had sub centimeter nodes and were under observation and one patient of Stage 4 was downgraded to Stage 2 and further received two more cycles.
Relapse after treatment was seen in three patients, of which one patient was receiving irregular treatment. One patient did not show any response to treatment and the diagnosis was revised as T-cell rich B-cell lymphoma. Most of the treatment failures were due poor patient compliance because of poor SE status and lack of awareness.
The overall survival (OS) was 98%, progress free survival (PFS) was 95%, and disease-free survival was 92%. Details regarding treatment and follow-up are given in Table 6.
Table 6
Depicting clinical stage, treatment and follow-up details
DISCUSSION
The literature available on significance of various histological features in diagnosis and prognosis of HL is still inadequate, especially in Indian context. With the aim of facilitating histological diagnosis of HL, a comprehensive review of various clinical and histological parameters, along with immunophenotyping was done.
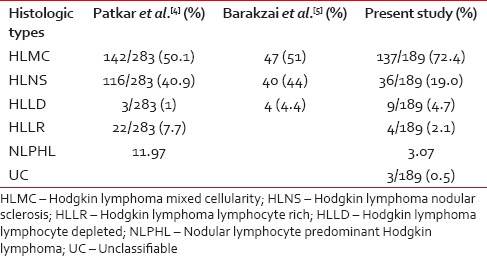
In this single institutional study, we reviewed 195 patients of HL along with all clinical, pathological and management details after excluding patients with incomplete details. The frequency of different histologic subtypes is compared with other studies in Table 4.
Table 4
Comparison of relative frequency of various histological subtypes in various studies
There was a bimodal age distribution with 2 peaks. The mean and median ages were a decade earlier than in western population. There was an overall male predominance with male:female ratio of 2.6:1, (CHL n = 189, male - 136/189, 71.9%:female - 53/189, 28%; NLPHL, n = 6, male - 6 [(100%]) similar to that reported by Patkar et al.[4] (CHL, male - 71%, female - 29%; NLPHL male - 78%, female - 22%) and Barakzai and Pervez[5] (CHL, male - 70, [76.9%]:female - 21 [23.%]).
The histological parameters analyzed such as, thickness of capsule, extacapsular invasion, effacement — whether complete or partial, fibrous bands, nodule formation, composition of background population of cells, type of RS cells, the presence of para amyloid, granulomas, necrosis, and mitosis did not have any prognostic significance independently. Prognosis was influenced by the clinical stage and other associated co-morbid illnesses. The individual histologic features did not predict for any difference in PFS or disease-specific survival.
Unlike Western population where HLNS is the most frequent subtype, HLMS was the most frequent (67%) in this study, followed by nodular sclerosing subtype (23.5%). In comparison to other Indian studies the frequency of HLMC was more in this study [Table 5]. The frequency of HLNS was low in our study because we applied very strict criteria and did not call it as HLNS unless it satisfied all the features.
Table 5
Comparison of immunophenotype in various study groups
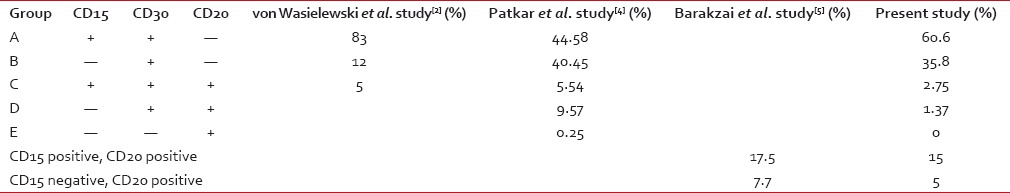
The patients were divided into six immunophenotypic groups as described by von Wasielewski et al.[2] The immunophenotype of patients in Group A represents the archetypical immunophenotype of CHL. Similar to the other two studies shown in Table 6, these patients were in a majority (60.6%). This is lower than that observed by von Wasielewski et al.[2] (83%) and higher than that of Patker et al.[4] Group B patients differed from Group A in lacking immunoreactivity for CD15. This group accounted for 35.8% of the patients of CHL.
Various studies have demonstrated positivity for CD20, ranging from 5% to 50%. In this study, 17.5% (7/40) patients of CHL were immunoreactive for CD20 which is similar to that reported by Barakzai and Pervez[5] (19.8%). CD15 negativity with CD20 positivity was seen in 2 (5%) patients of otherwise typical CHL which is also similar to that reported by Barakzai and Pervez[5] (7.7%) [Table 6].
The significance of CD20 expression by the RS cells is, as of now, a matter of controversy. In this study, one out of seven CD20 positive CHL patients showed relapse.
There was a slight prominence of HLMC in lower SE group (50.9%) than higher SE group whereas HLNS was more common in middle SE group (58.3%). Our results are in correlation with that reported in literature.[3] HLNS is a more common among resource rich.[3] HLMC and HLLD are more common in resource poor, correlating with increased incidence of Epstein-Barr virus (EBV) infection in this group.[3] However, we have not confirmed our findings by correlating with EBV infection in this study.
Most of the patients presented at advanced stage (Stage 3-42.5%), the patients presented even later when isolated intra-abdominal nodes were involved. In this study, the response to treatment was good when the patients had regular treatment. With median follow-up of 2 years, the OS was 98%, PFS was 95% and disease free survival was 92% which was higher compared to Laskar study[6] (event free survival [EFS] and OS in the chemotherapy alone arm were 76% and 89%, respectively and 88% and 100% in the chemotherapy radiotherapy arm). In Arya et al. study[7] the 5-year actuarial OS and EFS are 91.5 and 87.9%, respectively in children with median age of 8 years with chemotherapy alone. The treatment failures in this study were mainly due to poor patient compliance because of poor SE status and lack of awareness.
CONCLUSION
The age at presentation in HL was a decade earlier than in western population. Mixed cellularity was the most frequent subtype (67%), followed by nodular sclerosing subtype (23.5%).
In this paper, we have discussed in detail about various clinical and histopathological parameters of HL and their relative frequency in various histological subtypes. Most common presenting complaint was cervical lymphadenopathy. Prognosis was influenced by the clinical stage and other associated co-morbid illnesses rather than individual histological parameters.
The most common immunoprofile of HRS cells was represented by Group A (CD15+, CD30+, CD20−), which is the archetypical immunophenotype of CHL (60.6%).
India seems to have a high number of CD15 negative (35.8%) and a relatively higher number of CD20 positive CHL (17.5%) patients as compared to the western population.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no confliicts of interest.
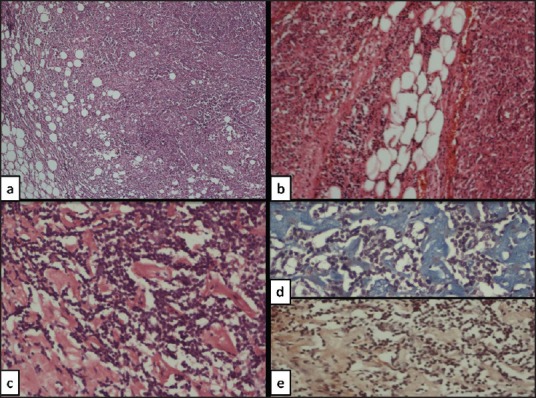
| Fig. 1 Various histological parameters studied (H and E): (a and b) Extracapsular infiltration (×100) (c-e) paraamyloid (d) Masson trichrome, (e) Congo red ×400
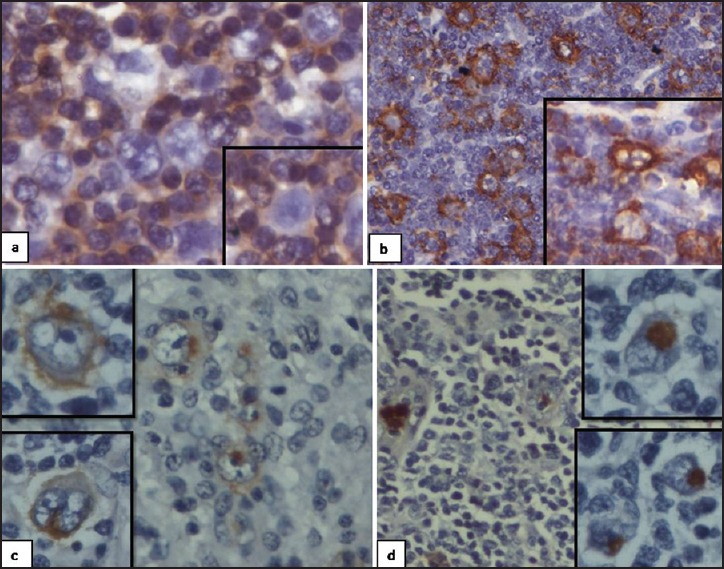
| Fig. 2 Immunohistochemistry (a) CD3 – positive in T lymphocytes forming rosettes around Reed Sternberg cells which is negative for CD3 (b) CD20 – positive in Reed Sternberg cells and B lymphocytes (c) CD 15 – positive in myeloid precursors and Reed Sternberg cells (Golgi and membrane positivity) (d) CD30 positive in Reed Sternberg cells (Golgi and membrane positivity)


 PDF
PDF  Views
Views  Share
Share

