Immediate treatment effects of high-dose methotrexate and cranial irradiation on neuropsychological functions of children treated for acute lymphoblastic leukemia at a regional cancer center
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2014; 35(04): 281-287
DOI: DOI: 10.4103/0971-5851.144990
Abstract
Context: Overall cure rates for pediatric acute lymphoblastic leukemia (ALL) have improved; however, the neuropsychological sequelae of ALL treatment have not been adequately documented in India. Aims: The present study assesses the immediate effects of ALL treatment on neuropsychological functioning, at the Regional Cancer Center in Chennai, South India. Materials and Methods: Newly diagnosed with ALL patients (n = 24) (aged 6-15 years; 13M:11F) registered between March 2008 and February 2009 were included. Patients who had received high-dose methotrexate (HD-MTX) and cranial radiotherapy (CRT) as part of their treatment were enrolled for the study. Neurocognitive assessments were done to assess various functions such as performance intelligence, visuo-perception, visuo-spatial, perceptual organization, processing speed, planning, working memory, and immediate verbal memory (IVM) (Malin′s intelligence scale); verbal fluency (ideation fluency test) and verbal attention (vigilance test). Three assessments were done during induction (baseline), after re-induction phase (second) and during the maintenance phase (third). Results: The patients performed significantly worse in the third assessment (mean duration from diagnosis 17.48 months) on performance intelligence quotient (PIQ), visuo-perception, visuo-spatial, processing speed, planning, IVM, verbal attention, and verbal fluency (P < 0 class="i" xss=removed>P > 0.05). Significant difference was observed between age groups 6 and 10 (41.7%) and 11-15 years (58.3%) in perceptual organization, verbal fluency, and verbal attention (P < 0 class="i" xss=removed>P > 0.05). Conclusions: Combining HD MTX and CRT had an immediate effect on neuropsychological sequelae among the children with ALL, however, long-term evaluation is recommended to study the long-term effects.
Keywords
Acute lymphoblastic leukemia - central nervous system prophylaxis - chemotherapy - cranial radiation - neuro-cognitive functionsPublication History
Article published online:
19 July 2021
© 2014. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Context:
Overall cure rates for pediatric acute lymphoblastic leukemia (ALL) have improved; however, the neuropsychological sequelae of ALL treatment have not been adequately documented in India.
Aims:
The present study assesses the immediate effects of ALL treatment on neuropsychological functioning, at the Regional Cancer Center in Chennai, South India.
Materials and Methods:
Newly diagnosed with ALL patients (n = 24) (aged 6–15 years; 13M:11F) registered between March 2008 and February 2009 were included. Patients who had received high-dose methotrexate (HD-MTX) and cranial radiotherapy (CRT) as part of their treatment were enrolled for the study. Neurocognitive assessments were done to assess various functions such as performance intelligence, visuo-perception, visuo-spatial, perceptual organization, processing speed, planning, working memory, and immediate verbal memory (IVM) (Malin's intelligence scale); verbal fluency (ideation fluency test) and verbal attention (vigilance test). Three assessments were done during induction (baseline), after re-induction phase (second) and during the maintenance phase (third).
Results:
The patients performed significantly worse in the third assessment (mean duration from diagnosis 17.48 months) on performance intelligence quotient (PIQ), visuo-perception, visuo-spatial, processing speed, planning, IVM, verbal attention, and verbal fluency (P < 0 xss=removed>P > 0.05). Significant difference was observed between age groups 6 and 10 (41.7%) and 11–15 years (58.3%) in perceptual organization, verbal fluency, and verbal attention (P < 0 xss=removed>P > 0.05).
Conclusions:
Combining HD MTX and CRT had an immediate effect on neuropsychological sequelae among the children with ALL, however, long-term evaluation is recommended to study the long-term effects.
INTRODUCTION
Acute lymphoblastic leukemia (ALL) is the most common form of childhood cancer in India. In the current scenario, the overall cure rates for pediatric ALL have improved up to 65-70%[1] due to central nervous system (CNS) prophylaxis, however, cognitive functioning is compromised by this[2,3,4,5,6] which includes cranial radiotherapy (CRT), intrathecal methotrexate (IT-MTX), and high-dose methotrexate (HD-MTX) literature reviews suggest that children treated with HD-MTX and IT-MTX perform better than children treated with CRT and IT-MTX. The complexity of different treatments for ALL has concluded that these can have an impact on the neuropsychological functioning. Children treated with CRT performed poorly in comparison to those treated with either HD-MTX or IT-MTX group on most neuropsychological functions. From the western review, it can be concluded very few data are available in the neurocognitive sequelae effect with HD-MTX and CRT,[7] there is also paucity of data in India. Moreover, the combined effect of HD-MTX and CRT is unknown. Therefore, a systematic prospective study was conducted to assess the immediate effect of neuropsychological functioning among the children with ALL children treated with combined HD-MTX and CRT at the Regional Cancer Center in Chennai, South India.
MATERIALS AND METHODS
Sample
Patients with ALL who were diagnosed between March 2008 and September 2009 were included in the study. Patients between the age group of 6 and 15 years who were treated with BFM 86 protocols, including CNS prophylactic treatment, that is, CNS-directed RT (18 Gy in 10 fractions) and IT-MTX along with HD-MTX at the Regional Cancer Center in Chennai, South India were taken for the study. Patients with history of any psychiatric illness, neurological disorders, and patients with CNS involvement at the time of the study and during follow-up were excluded. Informed consent was taken from the parents and children. All the eligible children and parents agreed to participate in the study.
Tools used
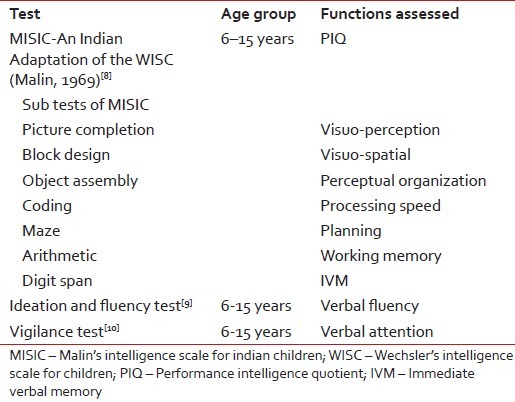
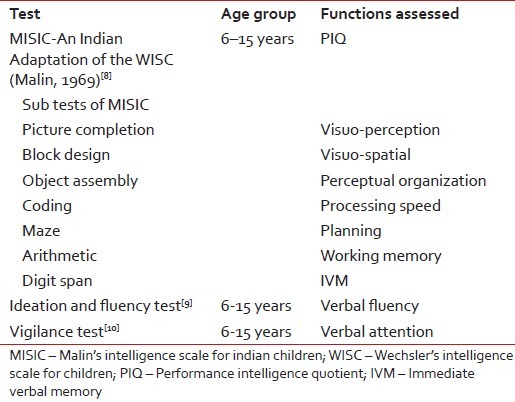
Table 1 shows neuropsychological assessments and its respective evaluative functions.
Table 1
Descriptions of the neuropsychological assessments
|
Assessment procedure and intervals
The baseline (first) assessment was conducted after the initiation of induction phase, once the patient's general condition was stabilized. The second assessment was done after the completion of consolidation and re-induction I phase, before the CRT. The third assessment was conducted post completion of CRT and re-induction II as well as during the maintenance period. These assessments did not interfere with the routine treatment, investigations, or other medical procedures. Each assessment was carried out by a team of professionals comprising an oncologist and a psychologist. The duration of the assessments was about 2-3 h, conducted in 50-60 min sessions with at least 5-10 min of break to overcome fatigue. There was approximately 5-6 months gap between each assessment, thereby preventing practice effect. All patients who had enrolled completed all the three assessments and no CNS disease or systemic relapse was observed during the period of study.
Statistical analysis of data
Data were analyzed using nonparametric test, viz., Friedman test was used to assess the difference between the three assessments, followed by Wilcoxon's signed-rank test, for pair-wise comparisons. Mann-Whitney U-test was used to assess the gender and age difference.
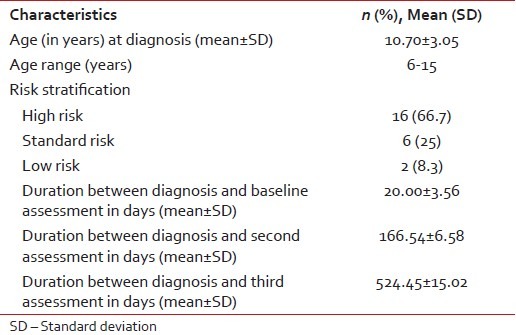
RESULTS
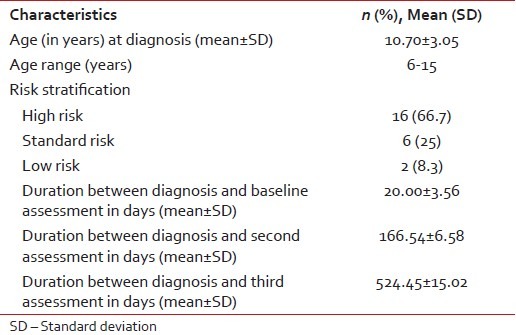
Thirty patients were enrolled for the study, of which 24 completed all the three assessments and they were included in the analysis. Sample characteristics are shown in Table 2. Of the 24 patients included for analysis, 13 (54.2%) were male and 11 (45.8%) were female, age ranged between 6 and 15 years with the mean age being 10.70 years. The duration of the first assessment from diagnosis ranged from 1 to 68 days (mean ± standard deviation (SD) = 20.00 ± 3.56). The duration between first and second assessment ranged from 90 to 217 days (mean ± SD = 146.54 ± 6.46) and it ranged from 117 to 223 days (mean ± SD = 166.54 ± 6.58) from the diagnosis. The duration of the second and third assessment ranged from 180 to 360 days (mean ± SD = 246.26 ± 9.27) and 364-558 days (mean ± SD = 524.45 ± 15.02), respectively, from diagnosis.
Table 2
Sample characteristics
|
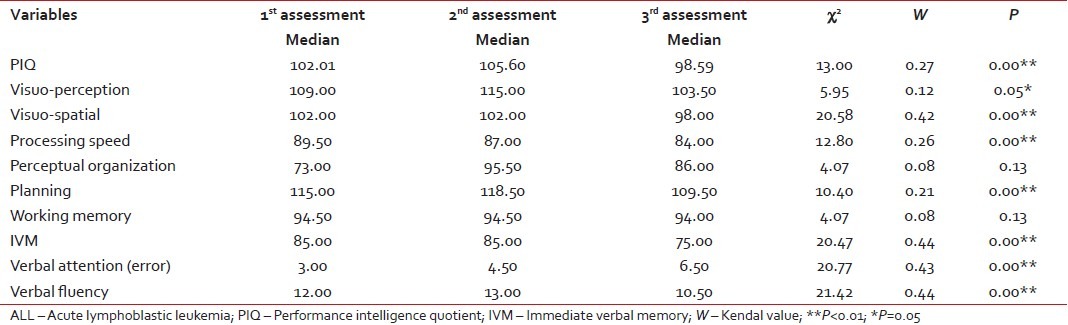
Changes in cognitive functioning following central nervous system prophylactic treatment
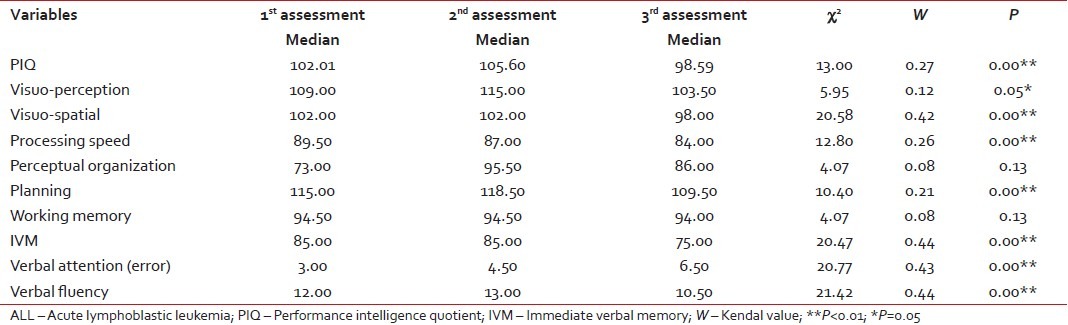
The effect of ALL treatment on Neuro-psychological functions of pediatric patients across three assessments are given in Table 3.
Table 3
Effect of ALL treatment on Neuro-psychological functions of pediatric patients
|
Intellectual abilities
The results showed significant changes between the medians of the three assessments in performance intelligence quotient (PIQ) (χ2 = 13.00, P < 0 xss=removed>W = 0.27). Follow-up pair-wise comparison results indicated that there was a significant difference in children's performance score between the first and second assessment (Z = −2.20, P < 0 xss=removed>Z = −3.96, P < 0 xss=removed>Z = −2.75, P < 0>
Visuo-perception
Significant changes were observed between the medians of three assessments in visuo-perception (χ2 = 5.95, P = 0.05). The Kendall's W results indicated that there was a weak agreement in the visuo-perception (W = 0.12). Follow-up pair-wise comparisons results indicated that there was no significant difference in the children's performance score between the first and second assessment (Z = −1.33, P > 0.05); second and third assessment (Z = −1.52, P > 0.05); and third and first assessment (Z = −0.72, P > 0.05). From the results, it can be concluded that performance of children improved in the second assessment when compared to first assessment and compared to the first and second assessment, children had decreased scores in the third assessment.
Visuo-spatial
There was significant change between the medians of the three assessment scores in visuo-spatial (χ2 = 20.58, P < 0 xss=removed>W results indicated that the agreement on the trend of performance among the children with ALL was strong in the visuo-spatial (W = 0.42). Follow-up pair-wise comparison results indicated that there was a significant difference in the children's performance score between second and third assessment (Z = −3.53, P < 0 xss=removed>Z = −2.44, P < 0>
Processing speed
The results showed significant changes between the medians of three assessments in processing speed (χ2 = 12.80, P < 0 xss=removed>W results indicated that the agreement on the trend of performance among the children with ALL was fair in processing speed (W = 0.26). Pair-wise comparison revealed that there was a significant difference in the children's performance score between the second and third assessment (Z = −2.44, P < 0 xss=removed>Z = −2.24, P < 0>
Perceptual organization
There were no significant changes between the medians of the three assessments in perceptual organization (χ2 = 4.07, P > 0.05). The Kendall's W results indicated that there was a weak agreement in the perceptual organization (W = 0.085) in all the three neuropsychological assessments. When comparing to the first assessment, median score of the children had performed better in the second and third assessment.
Planning
There was significant difference between the medians of the three assessments in planning (χ2 = 10.40, P = 0.00). Kendall's W results indicated that the agreement on the trend of performance among the children was fair in planning (W = 0.21). Follow-up pair-wise comparison test indicated that there was a significant difference in the children's performance score between the first and second assessment (Z = −2.36, P < 0>
Working memory
There were no significant difference between the medians of the three assessments in working memory (χ2 = 4.075, P = 0.13). Kendall's W results indicated that there was a weak agreement in working memory (W = 0.085) in all three neuropsychological assessments. There was no difference between the three assessments of children's medians score in working memory.
Immediate verbal memory
Results showed that there was a significant difference between the medians score of the three assessments in immediate verbal memory (IVM) (χ2 = 20.47, P < 0 xss=removed>W results indicated that there was an agreement on the trend of performance among children with ALL children was a strong in IVM (W = 0.44). Pair-wise comparison results showed that there was a significant difference in the children's performance score between second and third assessment (Z = −3.59, P < 0 xss=removed>01). There was no significant difference between the median scores of the first and second assessment in IVM. When compared to the first and second assessment, there was decrease in children's performance in the third assessment.
Verbal attention
Results showed that there was a significant difference between the median scores of the three assessments in verbal attention (error scores) (χ2 = 20.77, P = 0.00). Kendall's W results indicated that there was an agreement on the trend of performance among children with ALL was strong in verbal attention (W = 0.43). Follow-up pair-wise comparisons indicated that there was a significant difference in the children's performance score between the second and third assessment (Z = −3.35, P < 0>
Verbal fluency
Significant changes were observed between the median scores of the three assessments in verbal fluency (χ2 = 21.44, P = 0.00). Kendall's W results indicated that the agreement on the trend of performance among children with ALL children was strong in verbal fluency (W = 0.44). Pair-wise comparisons indicated that there was a significant difference in the children's performance score between the first and second assessment (Z = −2.20, P < 0>
Age and gender
The Mann-Whitney U-test indicated that there was a significant difference between the age group 6-10 years and 11-15 years in perceptual organization, verbal attention, and verbal fluency (P < 0 xss=removed>P < 0 xss=removed>P < 0>
DISCUSSION
The present study suggests that BFM 86 protocol including CRT and IT-MTX along with HD-MTX had an immediate effect on the neuropsychological functioning among children with ALL. Immediately after receiving IT-MTX and HD-MTX, there was no effect, however, in combination with CRT, there was a significant impact observed after 17.48 months from the time of diagnosis. A review study which was conducted by Copeland[11] concluded that neuropsychological impairments usually become evident within 1-3 years following the cranial irradiation and also showed that deficits are progressive.
In the present study, it was found that there was a significant impairment in many domains of neuropsychological functioning in children with ALL after receiving CNS prophylactic treatment, namely PIQ, visuo-perception, visuo-spatial, processing speed, planning, IVM, verbal attention, and verbal fluency.
On Malin's intelligence scale for Indian children (MISIC), when compared between the three assessments, it was found that PIQ of children significantly decreased at third assessment (98.5) compared with first (102.01) and second (105.6) assessment after receiving CNS prophylactic treatment. Though, there was a difference, the median intelligence score fell within the average range (90-109) as per Wechsler intelligence quotient (IQ) classification[8] in the three assessments for the children. The median IQ scores of children with ALL increased in the second assessment when compared to the first and third assessment. First assessment was done immediately after the diagnosis and during the induction period when the child was coping with the diagnosis, new environment, and the treatment procedures compared to the second assessment. Overall median score was within the average category in all the three assessments, three children scored below average (80-89) in the baseline assessment. Of them, two moved to average category during the second assessment and one child scored below average in all the three assessments. In addition, two children moved to below average category in the third assessment from the average category in the first two assessments.
Three Indian studies have reported the effect of CNS prophylactic treatment on neuropsychological functioning of children treated for ALL. Jain et al.,[12] conducted a retrospective study comparing children with ALL (n = 35) who received CNS prophylactic treatment with their healthy siblings (n = 20) who were between the age group of 5-15 years. Results showed that children with ALL performed significantly poorer when compared to their healthy siblings, the difference in their mean scores was 13.6 where the children with ALL received 20 Gy CRT. In the present study, the difference between the second assessment and third assessment was 7.09. Another prospective longitudinal study conducted by Abraham and Appaji,[13] 19 children with ALL treated with CNS prophylactic treatment were found to have significant decline in IQ and deficit in analytical reasoning. Contrary to the above two studies, a comparative study conducted by Bhattacharya et al.,[14] concluded that there was no significant difference in IQ between the children who received CNS prophylactic treatment and children with solid tumor who received only chemotherapy.
However, in line with Jain and Appaji studies, a western study was conducted by Anderson and Ochs[15,16] who revealed that children with ALL who received cranial irradiation and chemotherapy had poorer intellectual and educational skills in comparison to children who received only chemotherapy or healthy controls.
In the present study, after induction and consolidation phase, that is, before CRT, there was no significant difference in the neuropsychological functioning, which was also concluded from the studies which was conducted by Brown et al.,[17] and Anderson et al.,[15] where, they did not find any short-term effect in the neurocognitive functioning of the children with ALL treated with CNS directed chemotherapy only. Current study indicated a significant impairment on three of the MISIC sub tests; visuo-perception visuo-spatial, processing speed; planning and IVM, between the three assessments. The results of the present study is that certain neuropsychological domains are impaired which were consistent with the previous studies, where these three functions were reported to have impaired repeatedly after receiving CNS prophylactic treatment (visuo-perception,[9,15] visuo-spatial,[9,15] processing speed,[11,15,18] planning and IVM[11,16]). In addition to these functions, nonverbal ability such as perceptual organization and working memory were also found to have impairment in a study conducted by Anderson.[15] In the present study, though there was a decline in the scores of third assessment when compared to the first and second assessment, the impairment was not significant.
Verbal fluency and verbal attention were measured by ideation fluency and vigilance test respectively. On the ideation fluency test, there was a significant impairment in verbal fluency after receiving CNS prophylactic treatment. Result was consistent with the findings of Espy et al.,[18] who, have reported that there is a decline in verbal fluency. The decline in ideation fluency was observed after the radiation therapy was administered.
On Vigilance test, significant impairment was noted in verbal attention during the third assessment. There was a gradual increase in error scores in verbal attention from baseline to third assessment. This decline in verbal attention is progressive after the commencement of treatment. It is possible that both cranial radiation and chemotherapy had influenced verbal attention. Similarly, the study done by Langer et al.[19] and Giralt et al.,[20] concluded that cranial irradiation in combination with MTX therapy was associated with deficits in attention. Moreover, similar impairment in attention was reported in an Indian study conducted by Jain et al.,[12] though, there was a difference in the dosage of CRT administered, 20 Gy in Jain's study whereas, 18 Gy in the current study used.
There was no gender difference in neuropsychological functions. This is in contrast to the previous evidence[3,11,15] where it was reported that females were more affected than males after receiving CNS prophylactic therapy. Most of the previous evidences suggest that females are more prone for neurocognitive side effects than males due to gender difference which is due to the brain development.[3,11] This was not observed in the present study, which may be due to small sample size and less representation of female patients (n = 5).
Among the age groups between 6-10 years and 11-15 years, the children were found to have deficits in perceptual organization, verbal attention, and verbal fluency after receiving CNS prophylactic therapy. Most of the studies suggested that age of treatment is a proxy variable for underlying neurodevelopment maturity. While development of cortical gray matter peaks at approximately 4 years of age, cortical white matter volume continues to rise until 20 years of age. Therefore, those who are younger at the time of radiation treatment generally have less or fully developed white matter. Since both younger and older patients have shown to lose white matter volume at similar rates, the younger irradiated patients continue to display reduced total white matter volume following radiation treatment. These deficits in white matter volume among younger patients have also been associated with increased intellectual morbidity.[21]
In this study, although there was a decline in all the neuropsychological functions among all the children with ALL, long-term follow-up of these patients will reveal whether, this cognitive dysfunction is constant or deteriorating or improving. The current results must be interpreted in the context of some of the common limitations of clinical research. The effects of other contributing factors such as economical, social, environmental, and familial factors are not studied. The present study did not try to find the significant relationship or difference between chemotherapy and radiation. The sample was collected from a single institution and there was no control group. Current results are restricted to the age group of 6-15 years; hence, it cannot be generalized to other age groups. The present study strongly suggests that there is a decline in the cognitive function, early intervention (after 1-year) on cognitive rehabilitation is vital for all survivors. Academic achievement was not measured as the children were hospitalized during the intensive phase of the treatment and subsequently had intermittent admissions, and therefore, not attending their regular school. Hence, there is a need for future studies focusing on academic achievement as well as intervention. Hospital-based educational activities and intervention stimulating the cognition can help these children resume their routine and academic activities at the earliest.
The present study implicates that combined use of CRT and HD-MTX had an immediate effect on the neurocognitive functions among children with ALL. Cognitive rehabilitation is vital to improve their overall level of cognitive functioning and quality of life. Involving parents and teachers in the recovery process is crucial. The current study has focused on the short-term cognitive effects of CNS prophylaxis treatment and this can be expanded to look into the long term effect.
The present study supports the need for continued evaluation of neurocognitive functioning in Indian children with ALL, who are receiving CNS prophylactic therapy to identify potential neurocognitive sequelae of treatment. Prevention of neurocognitive sequelae through rehabilitative measures and continuation of school and pharmacotherapy for these children is recommended.
ACKNOWLEDGMENT
The authors are grateful to all pediatric cancer patients who participated in the study. We are grateful to Dr. Surendran, Assistant Professor, Department of Psycho-oncology, for helping in the conceptualization of the study design, and Ms. Prema Loganathan, and Ms. Saritha, Psychologists, Department of Psycho-oncology, for their assistance in administering the tests. We thank Ms. Subathra Jayaram, Ph. D. Research Scholar and Ms. Sakunthala for editing the manuscript.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Arora RS, Eden TO, Kapoor G. Epidemiology of childhood cancer in India. Indian J Cancer 2009;46:264-73.
- Copeland DR, Dowell RE Jr, Fletcher JM, Bordeaux JD, Sullivan MP, Jaffe N, et al. Neuropsychological effects of childhood cancer treatment. J Child Neurol 1988;3:53-62.
- Moleski M. Neuropsychological, neuroanatomical, and neurophysiological consequences of CNS chemotherapy for acute lymphoblastic leukemia. Arch Clin Neuropsychol 2000;15:603-30.
- Buizer AI, de Sonneville LM, Veerman AJ. Effects of chemotherapy on neurocognitive function in children with acute lymphoblastic leukemia: A critical review of the literature. Pediatr Blood Cancer 2009;52:447-54.
- Campbell LK, Scaduto M, Van Slyke D, Niarhos F, Whitlock JA, Compas BE. Executive function, coping, and behavior in survivors of childhood acute lymphocytic leukemia. J Pediatr Psychol 2009;34:317-27.
- Rowland JH, Glidewell OJ, Sibley RF, Holland JC, Tull R, Berman A, et al. Effects of different forms of central nervous system prophylaxis on neuropsychologic function in childhood leukemia. J Clin Oncol 1984;2:1327-35.
- Spiegler BJ, Kennedy K, Maze R, Greenberg ML, Weitzman S, Hitzler JK, et al. Comparison of long-term neurocognitive outcomes in young children with acute lymphoblastic leukemia treated with cranial radiation or high-dose or very high-dose intravenous methotrexate. J Clin Oncol 2006;24:3858-64.
- Malin AJ. Manual for Malin′s Intelligence Scale for Indian Children (MISIC). Lucknow: Indian Psychological Corporation; 1969.
- Mukundan CR. NIMHANS Neuropsychological Battery: test Description, Instructions, Clinical Data and Interpretation. NIMHANS, India, Bangalore: NIMHANS Publications; 1996.
- Strub RL, Black FW. The Mental Status Examination in Neurology. 3 rd ed. New Delhi: Jaypee Brothers Medical Publishers (p) Ltd.; 1995.
- Copeland DR. Neuropsychological and psychosocial effects of childhood leukemia and its treatment. CA Cancer J Clin 1992;42:283-95.
- Jain Y, Choudhry VP, Arya LS, Mehta M. Neuropsychological abnormalities following CNS prophylaxis in children with acute lymphatic leukemia. Indian J Pediatr 1993;60:675-81.
- Abraham A, Appaji L. Cognitive assessment of children with acute lymphoblastic leukemia: Preliminary findings. Indian J Med Paediatr Oncol 2009;30:14-9.
- Bhattacharya B, Marwaha RK, Malhotra S, Pershad D. Intellectual functions in childhood malignant disorders. Indian Pediatr 1995;32:869-75.
- Anderson V, Smibert E, Ekert H, Godber T. Intellectual, educational, and behavioural sequelae after cranial irradiation and chemotherapy. Arch Dis Child 1994;70:476-83.
- Ochs J, Mulhern R, Fairclough D, Parvey L, Whitaker J, Ch′ien L, et al. Comparison of neuropsychologic functioning and clinical indicators of neurotoxicity in long-term survivors of childhood leukemia given cranial radiation or parenteral methotrexate: a prospective study. J Clin Oncol 1991;9:145-51.
- Brown RT, Madan-Swain A, Pais R, Lambert RG, Baldwin K, Casey R, et al. Cognitive status of children treated with central nervous system prophylactic chemotherapy for acute lymphocytic leukemia. Arch Clin Neuropsychol 1992;7:481-97.
- Espy KA, Moore IM, Kaufmann PM, Kramer JH, Matthay K, Hutter JJ. Chemotherapeutic CNS prophylaxis and neuropsychologic change in children with acute lymphoblastic leukemia: A prospective study. J Pediatr Psychol 2001;26:1-9.
- Langer T, Martus P, Ottensmeier H, Hertzberg H, Beck JD, Meier W. CNS late-effects after ALL therapy in childhood. Part III: Neuropsychological performance in long-term survivors of childhood ALL: Impairments of concentration, attention, and memory. Med Pediatr Oncol 2002;38:320-8.
- Giralt J, Ortega JJ, Olive T, Verges R, Forio I, Salvador L. Long-term neuropsychologic sequelae of childhood leukemia: Comparison of two CNS prophylactic regimens. Int J Radiat Oncol Biol Phys 1992;24:49-53.
- Reddick WE, Shan ZY, Glass JO, Helton S, Xiong X, Wu S, et al. Smaller white-matter volumes are associated with larger deficits in attention and learning among long-term survivors of acute lymphoblastic leukemia. Cancer 2006;106:941-9.
Abstract
Context:
Overall cure rates for pediatric acute lymphoblastic leukemia (ALL) have improved; however, the neuropsychological sequelae of ALL treatment have not been adequately documented in India.
Aims:
The present study assesses the immediate effects of ALL treatment on neuropsychological functioning, at the Regional Cancer Center in Chennai, South India.
Materials and Methods:
Newly diagnosed with ALL patients (n = 24) (aged 6–15 years; 13M:11F) registered between March 2008 and February 2009 were included. Patients who had received high-dose methotrexate (HD-MTX) and cranial radiotherapy (CRT) as part of their treatment were enrolled for the study. Neurocognitive assessments were done to assess various functions such as performance intelligence, visuo-perception, visuo-spatial, perceptual organization, processing speed, planning, working memory, and immediate verbal memory (IVM) (Malin's intelligence scale); verbal fluency (ideation fluency test) and verbal attention (vigilance test). Three assessments were done during induction (baseline), after re-induction phase (second) and during the maintenance phase (third).
Results:
The patients performed significantly worse in the third assessment (mean duration from diagnosis 17.48 months) on performance intelligence quotient (PIQ), visuo-perception, visuo-spatial, processing speed, planning, IVM, verbal attention, and verbal fluency (P < 0 xss=removed>P > 0.05). Significant difference was observed between age groups 6 and 10 (41.7%) and 11–15 years (58.3%) in perceptual organization, verbal fluency, and verbal attention (P < 0 xss=removed>P > 0.05).
Conclusions:
Combining HD MTX and CRT had an immediate effect on neuropsychological sequelae among the children with ALL, however, long-term evaluation is recommended to study the long-term effects.
INTRODUCTION
Acute lymphoblastic leukemia (ALL) is the most common form of childhood cancer in India. In the current scenario, the overall cure rates for pediatric ALL have improved up to 65-70%[1] due to central nervous system (CNS) prophylaxis, however, cognitive functioning is compromised by this[2,3,4,5,6] which includes cranial radiotherapy (CRT), intrathecal methotrexate (IT-MTX), and high-dose methotrexate (HD-MTX) literature reviews suggest that children treated with HD-MTX and IT-MTX perform better than children treated with CRT and IT-MTX. The complexity of different treatments for ALL has concluded that these can have an impact on the neuropsychological functioning. Children treated with CRT performed poorly in comparison to those treated with either HD-MTX or IT-MTX group on most neuropsychological functions. From the western review, it can be concluded very few data are available in the neurocognitive sequelae effect with HD-MTX and CRT,[7] there is also paucity of data in India. Moreover, the combined effect of HD-MTX and CRT is unknown. Therefore, a systematic prospective study was conducted to assess the immediate effect of neuropsychological functioning among the children with ALL children treated with combined HD-MTX and CRT at the Regional Cancer Center in Chennai, South India.
MATERIALS AND METHODS
Sample
Patients with ALL who were diagnosed between March 2008 and September 2009 were included in the study. Patients between the age group of 6 and 15 years who were treated with BFM 86 protocols, including CNS prophylactic treatment, that is, CNS-directed RT (18 Gy in 10 fractions) and IT-MTX along with HD-MTX at the Regional Cancer Center in Chennai, South India were taken for the study. Patients with history of any psychiatric illness, neurological disorders, and patients with CNS involvement at the time of the study and during follow-up were excluded. Informed consent was taken from the parents and children. All the eligible children and parents agreed to participate in the study.
Tools used
Table 1 shows neuropsychological assessments and its respective evaluative functions.
Table 1
Descriptions of the neuropsychological assessments
|
Assessment procedure and intervals
The baseline (first) assessment was conducted after the initiation of induction phase, once the patient's general condition was stabilized. The second assessment was done after the completion of consolidation and re-induction I phase, before the CRT. The third assessment was conducted post completion of CRT and re-induction II as well as during the maintenance period. These assessments did not interfere with the routine treatment, investigations, or other medical procedures. Each assessment was carried out by a team of professionals comprising an oncologist and a psychologist. The duration of the assessments was about 2-3 h, conducted in 50-60 min sessions with at least 5-10 min of break to overcome fatigue. There was approximately 5-6 months gap between each assessment, thereby preventing practice effect. All patients who had enrolled completed all the three assessments and no CNS disease or systemic relapse was observed during the period of study.
Statistical analysis of data
Data were analyzed using nonparametric test, viz., Friedman test was used to assess the difference between the three assessments, followed by Wilcoxon's signed-rank test, for pair-wise comparisons. Mann-Whitney U-test was used to assess the gender and age difference.
RESULTS
Thirty patients were enrolled for the study, of which 24 completed all the three assessments and they were included in the analysis. Sample characteristics are shown in Table 2. Of the 24 patients included for analysis, 13 (54.2%) were male and 11 (45.8%) were female, age ranged between 6 and 15 years with the mean age being 10.70 years. The duration of the first assessment from diagnosis ranged from 1 to 68 days (mean ± standard deviation (SD) = 20.00 ± 3.56). The duration between first and second assessment ranged from 90 to 217 days (mean ± SD = 146.54 ± 6.46) and it ranged from 117 to 223 days (mean ± SD = 166.54 ± 6.58) from the diagnosis. The duration of the second and third assessment ranged from 180 to 360 days (mean ± SD = 246.26 ± 9.27) and 364-558 days (mean ± SD = 524.45 ± 15.02), respectively, from diagnosis.
Table 2
Sample characteristics
|
Changes in cognitive functioning following central nervous system prophylactic treatment
The effect of ALL treatment on Neuro-psychological functions of pediatric patients across three assessments are given in Table 3.
Table 3
Effect of ALL treatment on Neuro-psychological functions of pediatric patients
|
Intellectual abilities
The results showed significant changes between the medians of the three assessments in performance intelligence quotient (PIQ) (χ2 = 13.00, P < 0 xss=removed>W = 0.27). Follow-up pair-wise comparison results indicated that there was a significant difference in children's performance score between the first and second assessment (Z = −2.20, P < 0 xss=removed>Z = −3.96, P < 0 xss=removed>Z = −2.75, P < 0>
Visuo-perception
Significant changes were observed between the medians of three assessments in visuo-perception (χ2 = 5.95, P = 0.05). The Kendall's W results indicated that there was a weak agreement in the visuo-perception (W = 0.12). Follow-up pair-wise comparisons results indicated that there was no significant difference in the children's performance score between the first and second assessment (Z = −1.33, P > 0.05); second and third assessment (Z = −1.52, P > 0.05); and third and first assessment (Z = −0.72, P > 0.05). From the results, it can be concluded that performance of children improved in the second assessment when compared to first assessment and compared to the first and second assessment, children had decreased scores in the third assessment.
Visuo-spatial
There was significant change between the medians of the three assessment scores in visuo-spatial (χ2 = 20.58, P < 0 xss=removed>W results indicated that the agreement on the trend of performance among the children with ALL was strong in the visuo-spatial (W = 0.42). Follow-up pair-wise comparison results indicated that there was a significant difference in the children's performance score between second and third assessment (Z = −3.53, P < 0 xss=removed>Z = −2.44, P < 0>
Processing speed
The results showed significant changes between the medians of three assessments in processing speed (χ2 = 12.80, P < 0 xss=removed>W results indicated that the agreement on the trend of performance among the children with ALL was fair in processing speed (W = 0.26). Pair-wise comparison revealed that there was a significant difference in the children's performance score between the second and third assessment (Z = −2.44, P < 0 xss=removed>Z = −2.24, P < 0>
Perceptual organization
There were no significant changes between the medians of the three assessments in perceptual organization (χ2 = 4.07, P > 0.05). The Kendall's W results indicated that there was a weak agreement in the perceptual organization (W = 0.085) in all the three neuropsychological assessments. When comparing to the first assessment, median score of the children had performed better in the second and third assessment.
Planning
There was significant difference between the medians of the three assessments in planning (χ2 = 10.40, P = 0.00). Kendall's W results indicated that the agreement on the trend of performance among the children was fair in planning (W = 0.21). Follow-up pair-wise comparison test indicated that there was a significant difference in the children's performance score between the first and second assessment (Z = −2.36, P < 0>
Working memory
There were no significant difference between the medians of the three assessments in working memory (χ2 = 4.075, P = 0.13). Kendall's W results indicated that there was a weak agreement in working memory (W = 0.085) in all three neuropsychological assessments. There was no difference between the three assessments of children's medians score in working memory.
Immediate verbal memory
Results showed that there was a significant difference between the medians score of the three assessments in immediate verbal memory (IVM) (χ2 = 20.47, P < 0 xss=removed>W results indicated that there was an agreement on the trend of performance among children with ALL children was a strong in IVM (W = 0.44). Pair-wise comparison results showed that there was a significant difference in the children's performance score between second and third assessment (Z = −3.59, P < 0 xss=removed>01). There was no significant difference between the median scores of the first and second assessment in IVM. When compared to the first and second assessment, there was decrease in children's performance in the third assessment.
Verbal attention
Results showed that there was a significant difference between the median scores of the three assessments in verbal attention (error scores) (χ2 = 20.77, P = 0.00). Kendall's W results indicated that there was an agreement on the trend of performance among children with ALL was strong in verbal attention (W = 0.43). Follow-up pair-wise comparisons indicated that there was a significant difference in the children's performance score between the second and third assessment (Z = −3.35, P < 0>
Verbal fluency
Significant changes were observed between the median scores of the three assessments in verbal fluency (χ2 = 21.44, P = 0.00). Kendall's W results indicated that the agreement on the trend of performance among children with ALL children was strong in verbal fluency (W = 0.44). Pair-wise comparisons indicated that there was a significant difference in the children's performance score between the first and second assessment (Z = −2.20, P < 0>
Age and gender
The Mann-Whitney U-test indicated that there was a significant difference between the age group 6-10 years and 11-15 years in perceptual organization, verbal attention, and verbal fluency (P < 0 xss=removed>P < 0 xss=removed>P < 0>
DISCUSSION
The present study suggests that BFM 86 protocol including CRT and IT-MTX along with HD-MTX had an immediate effect on the neuropsychological functioning among children with ALL. Immediately after receiving IT-MTX and HD-MTX, there was no effect, however, in combination with CRT, there was a significant impact observed after 17.48 months from the time of diagnosis. A review study which was conducted by Copeland[11] concluded that neuropsychological impairments usually become evident within 1-3 years following the cranial irradiation and also showed that deficits are progressive.
In the present study, it was found that there was a significant impairment in many domains of neuropsychological functioning in children with ALL after receiving CNS prophylactic treatment, namely PIQ, visuo-perception, visuo-spatial, processing speed, planning, IVM, verbal attention, and verbal fluency.
On Malin's intelligence scale for Indian children (MISIC), when compared between the three assessments, it was found that PIQ of children significantly decreased at third assessment (98.5) compared with first (102.01) and second (105.6) assessment after receiving CNS prophylactic treatment. Though, there was a difference, the median intelligence score fell within the average range (90-109) as per Wechsler intelligence quotient (IQ) classification[8] in the three assessments for the children. The median IQ scores of children with ALL increased in the second assessment when compared to the first and third assessment. First assessment was done immediately after the diagnosis and during the induction period when the child was coping with the diagnosis, new environment, and the treatment procedures compared to the second assessment. Overall median score was within the average category in all the three assessments, three children scored below average (80-89) in the baseline assessment. Of them, two moved to average category during the second assessment and one child scored below average in all the three assessments. In addition, two children moved to below average category in the third assessment from the average category in the first two assessments.
Three Indian studies have reported the effect of CNS prophylactic treatment on neuropsychological functioning of children treated for ALL. Jain et al.,[12] conducted a retrospective study comparing children with ALL (n = 35) who received CNS prophylactic treatment with their healthy siblings (n = 20) who were between the age group of 5-15 years. Results showed that children with ALL performed significantly poorer when compared to their healthy siblings, the difference in their mean scores was 13.6 where the children with ALL received 20 Gy CRT. In the present study, the difference between the second assessment and third assessment was 7.09. Another prospective longitudinal study conducted by Abraham and Appaji,[13] 19 children with ALL treated with CNS prophylactic treatment were found to have significant decline in IQ and deficit in analytical reasoning. Contrary to the above two studies, a comparative study conducted by Bhattacharya et al.,[14] concluded that there was no significant difference in IQ between the children who received CNS prophylactic treatment and children with solid tumor who received only chemotherapy.
However, in line with Jain and Appaji studies, a western study was conducted by Anderson and Ochs[15,16] who revealed that children with ALL who received cranial irradiation and chemotherapy had poorer intellectual and educational skills in comparison to children who received only chemotherapy or healthy controls.
In the present study, after induction and consolidation phase, that is, before CRT, there was no significant difference in the neuropsychological functioning, which was also concluded from the studies which was conducted by Brown et al.,[17] and Anderson et al.,[15] where, they did not find any short-term effect in the neurocognitive functioning of the children with ALL treated with CNS directed chemotherapy only. Current study indicated a significant impairment on three of the MISIC sub tests; visuo-perception visuo-spatial, processing speed; planning and IVM, between the three assessments. The results of the present study is that certain neuropsychological domains are impaired which were consistent with the previous studies, where these three functions were reported to have impaired repeatedly after receiving CNS prophylactic treatment (visuo-perception,[9,15] visuo-spatial,[9,15] processing speed,[11,15,18] planning and IVM[11,16]). In addition to these functions, nonverbal ability such as perceptual organization and working memory were also found to have impairment in a study conducted by Anderson.[15] In the present study, though there was a decline in the scores of third assessment when compared to the first and second assessment, the impairment was not significant.
Verbal fluency and verbal attention were measured by ideation fluency and vigilance test respectively. On the ideation fluency test, there was a significant impairment in verbal fluency after receiving CNS prophylactic treatment. Result was consistent with the findings of Espy et al.,[18] who, have reported that there is a decline in verbal fluency. The decline in ideation fluency was observed after the radiation therapy was administered.
On Vigilance test, significant impairment was noted in verbal attention during the third assessment. There was a gradual increase in error scores in verbal attention from baseline to third assessment. This decline in verbal attention is progressive after the commencement of treatment. It is possible that both cranial radiation and chemotherapy had influenced verbal attention. Similarly, the study done by Langer et al.[19] and Giralt et al.,[20] concluded that cranial irradiation in combination with MTX therapy was associated with deficits in attention. Moreover, similar impairment in attention was reported in an Indian study conducted by Jain et al.,[12] though, there was a difference in the dosage of CRT administered, 20 Gy in Jain's study whereas, 18 Gy in the current study used.
There was no gender difference in neuropsychological functions. This is in contrast to the previous evidence[3,11,15] where it was reported that females were more affected than males after receiving CNS prophylactic therapy. Most of the previous evidences suggest that females are more prone for neurocognitive side effects than males due to gender difference which is due to the brain development.[3,11] This was not observed in the present study, which may be due to small sample size and less representation of female patients (n = 5).
Among the age groups between 6-10 years and 11-15 years, the children were found to have deficits in perceptual organization, verbal attention, and verbal fluency after receiving CNS prophylactic therapy. Most of the studies suggested that age of treatment is a proxy variable for underlying neurodevelopment maturity. While development of cortical gray matter peaks at approximately 4 years of age, cortical white matter volume continues to rise until 20 years of age. Therefore, those who are younger at the time of radiation treatment generally have less or fully developed white matter. Since both younger and older patients have shown to lose white matter volume at similar rates, the younger irradiated patients continue to display reduced total white matter volume following radiation treatment. These deficits in white matter volume among younger patients have also been associated with increased intellectual morbidity.[21]
In this study, although there was a decline in all the neuropsychological functions among all the children with ALL, long-term follow-up of these patients will reveal whether, this cognitive dysfunction is constant or deteriorating or improving. The current results must be interpreted in the context of some of the common limitations of clinical research. The effects of other contributing factors such as economical, social, environmental, and familial factors are not studied. The present study did not try to find the significant relationship or difference between chemotherapy and radiation. The sample was collected from a single institution and there was no control group. Current results are restricted to the age group of 6-15 years; hence, it cannot be generalized to other age groups. The present study strongly suggests that there is a decline in the cognitive function, early intervention (after 1-year) on cognitive rehabilitation is vital for all survivors. Academic achievement was not measured as the children were hospitalized during the intensive phase of the treatment and subsequently had intermittent admissions, and therefore, not attending their regular school. Hence, there is a need for future studies focusing on academic achievement as well as intervention. Hospital-based educational activities and intervention stimulating the cognition can help these children resume their routine and academic activities at the earliest.
The present study implicates that combined use of CRT and HD-MTX had an immediate effect on the neurocognitive functions among children with ALL. Cognitive rehabilitation is vital to improve their overall level of cognitive functioning and quality of life. Involving parents and teachers in the recovery process is crucial. The current study has focused on the short-term cognitive effects of CNS prophylaxis treatment and this can be expanded to look into the long term effect.
The present study supports the need for continued evaluation of neurocognitive functioning in Indian children with ALL, who are receiving CNS prophylactic therapy to identify potential neurocognitive sequelae of treatment. Prevention of neurocognitive sequelae through rehabilitative measures and continuation of school and pharmacotherapy for these children is recommended.
ACKNOWLEDGMENT
The authors are grateful to all pediatric cancer patients who participated in the study. We are grateful to Dr. Surendran, Assistant Professor, Department of Psycho-oncology, for helping in the conceptualization of the study design, and Ms. Prema Loganathan, and Ms. Saritha, Psychologists, Department of Psycho-oncology, for their assistance in administering the tests. We thank Ms. Subathra Jayaram, Ph. D. Research Scholar and Ms. Sakunthala for editing the manuscript.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Arora RS, Eden TO, Kapoor G. Epidemiology of childhood cancer in India. Indian J Cancer 2009;46:264-73.
- Copeland DR, Dowell RE Jr, Fletcher JM, Bordeaux JD, Sullivan MP, Jaffe N, et al. Neuropsychological effects of childhood cancer treatment. J Child Neurol 1988;3:53-62.
- Moleski M. Neuropsychological, neuroanatomical, and neurophysiological consequences of CNS chemotherapy for acute lymphoblastic leukemia. Arch Clin Neuropsychol 2000;15:603-30.
- Buizer AI, de Sonneville LM, Veerman AJ. Effects of chemotherapy on neurocognitive function in children with acute lymphoblastic leukemia: A critical review of the literature. Pediatr Blood Cancer 2009;52:447-54.
- Campbell LK, Scaduto M, Van Slyke D, Niarhos F, Whitlock JA, Compas BE. Executive function, coping, and behavior in survivors of childhood acute lymphocytic leukemia. J Pediatr Psychol 2009;34:317-27.
- Rowland JH, Glidewell OJ, Sibley RF, Holland JC, Tull R, Berman A, et al. Effects of different forms of central nervous system prophylaxis on neuropsychologic function in childhood leukemia. J Clin Oncol 1984;2:1327-35.
- Spiegler BJ, Kennedy K, Maze R, Greenberg ML, Weitzman S, Hitzler JK, et al. Comparison of long-term neurocognitive outcomes in young children with acute lymphoblastic leukemia treated with cranial radiation or high-dose or very high-dose intravenous methotrexate. J Clin Oncol 2006;24:3858-64.
- Malin AJ. Manual for Malin′s Intelligence Scale for Indian Children (MISIC). Lucknow: Indian Psychological Corporation; 1969.
- Mukundan CR. NIMHANS Neuropsychological Battery: test Description, Instructions, Clinical Data and Interpretation. NIMHANS, India, Bangalore: NIMHANS Publications; 1996.
- Strub RL, Black FW. The Mental Status Examination in Neurology. 3 rd ed. New Delhi: Jaypee Brothers Medical Publishers (p) Ltd.; 1995.
- Copeland DR. Neuropsychological and psychosocial effects of childhood leukemia and its treatment. CA Cancer J Clin 1992;42:283-95.
- Jain Y, Choudhry VP, Arya LS, Mehta M. Neuropsychological abnormalities following CNS prophylaxis in children with acute lymphatic leukemia. Indian J Pediatr 1993;60:675-81.
- Abraham A, Appaji L. Cognitive assessment of children with acute lymphoblastic leukemia: Preliminary findings. Indian J Med Paediatr Oncol 2009;30:14-9.
- Bhattacharya B, Marwaha RK, Malhotra S, Pershad D. Intellectual functions in childhood malignant disorders. Indian Pediatr 1995;32:869-75.
- Anderson V, Smibert E, Ekert H, Godber T. Intellectual, educational, and behavioural sequelae after cranial irradiation and chemotherapy. Arch Dis Child 1994;70:476-83.
- Ochs J, Mulhern R, Fairclough D, Parvey L, Whitaker J, Ch′ien L, et al. Comparison of neuropsychologic functioning and clinical indicators of neurotoxicity in long-term survivors of childhood leukemia given cranial radiation or parenteral methotrexate: a prospective study. J Clin Oncol 1991;9:145-51.
- Brown RT, Madan-Swain A, Pais R, Lambert RG, Baldwin K, Casey R, et al. Cognitive status of children treated with central nervous system prophylactic chemotherapy for acute lymphocytic leukemia. Arch Clin Neuropsychol 1992;7:481-97.
- Espy KA, Moore IM, Kaufmann PM, Kramer JH, Matthay K, Hutter JJ. Chemotherapeutic CNS prophylaxis and neuropsychologic change in children with acute lymphoblastic leukemia: A prospective study. J Pediatr Psychol 2001;26:1-9.
- Langer T, Martus P, Ottensmeier H, Hertzberg H, Beck JD, Meier W. CNS late-effects after ALL therapy in childhood. Part III: Neuropsychological performance in long-term survivors of childhood ALL: Impairments of concentration, attention, and memory. Med Pediatr Oncol 2002;38:320-8.
- Giralt J, Ortega JJ, Olive T, Verges R, Forio I, Salvador L. Long-term neuropsychologic sequelae of childhood leukemia: Comparison of two CNS prophylactic regimens. Int J Radiat Oncol Biol Phys 1992;24:49-53.
- Reddick WE, Shan ZY, Glass JO, Helton S, Xiong X, Wu S, et al. Smaller white-matter volumes are associated with larger deficits in attention and learning among long-term survivors of acute lymphoblastic leukemia. Cancer 2006;106:941-9.


 PDF
PDF  Views
Views  Share
Share

