Indian Council of Medical Research Consensus Document for the Management of Gastroenteropancreatic Neuroendocrine Neoplasms
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2020; 41(02): 166-172
DOI: DOI: 10.4103/ijmpo.ijmpo_165_19
This consensus document may be used as a framework for more focused and planned research programs to carry forward the process. The aim of the Indian Council of Medical Research Guidelines is to assist oncologists in making major clinical decisions encountered while managing their patients while realizing the fact that some patients may require treatment strategies other than those suggested in these guidelines.
The histological confirmation which includes the measurement of the proliferative index (Ki67) is mandatory prior to the commencement of definitive treatment
All patients should be staged according to the TNM staging system, and risk should be assessed at diagnosis. A baseline contrast-enhanced computed tomography scan of the chest, abdomen, and pelvis should be considered
Selected cases should be referred to genetic clinics (MEN syndrome)
Patients should receive multidisciplinary care under the care of a surgical, medical, radiation oncologist, and nuclear medicine specialist
Primary surgery remains the standard of care for all nonmetastatic tumors. Patients with advanced gastroenteropancreatic neuroendocrine neoplasms (GEP-NENs) should be assessed on an individual basis to determine whether chemotherapy, targeted therapy, PRRT, or best supportive care should be provided
Preferred regimens for chemotherapy include – capecitabine-temozolomide, cisplatin-etoposide and for targeted therapy – everolimus and sunitinib
Patients should be offered regular surveillance after completion of curative resection or treatment of advanced disease
Encourage participation in institutional and ethical review board-approved, registered controlled clinical trials
Refer for early palliative care, if indicated.
Publication History
Received: 04 August 2019
Accepted: 24 October 2019
Article published online:
23 May 2021
© 2020. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
This consensus document may be used as a framework for more focused and planned research programs to carry forward the process. The aim of the Indian Council of Medical Research Guidelines is to assist oncologists in making major clinical decisions encountered while managing their patients while realizing the fact that some patients may require treatment strategies other than those suggested in these guidelines.
The histological confirmation which includes the measurement of the proliferative index (Ki67) is mandatory prior to the commencement of definitive treatment
All patients should be staged according to the TNM staging system, and risk should be assessed at diagnosis. A baseline contrast-enhanced computed tomography scan of the chest, abdomen, and pelvis should be considered
Selected cases should be referred to genetic clinics (MEN syndrome)
Patients should receive multidisciplinary care under the care of a surgical, medical, radiation oncologist, and nuclear medicine specialist
Primary surgery remains the standard of care for all nonmetastatic tumors. Patients with advanced gastroenteropancreatic neuroendocrine neoplasms (GEP-NENs) should be assessed on an individual basis to determine whether chemotherapy, targeted therapy, PRRT, or best supportive care should be provided
Preferred regimens for chemotherapy include – capecitabine-temozolomide, cisplatin-etoposide and for targeted therapy – everolimus and sunitinib
Patients should be offered regular surveillance after completion of curative resection or treatment of advanced disease
Encourage participation in institutional and ethical review board-approved, registered controlled clinical trials
Refer for early palliative care, if indicated.
Incidence
GEP-NENs are tumors resulting from the malignant transformation of cells in the diffuse neuroendocrine system that regulates secretion and motility in the gastrointestinal (GI) tract.[1] The term GEP-NENs is currently the adopted nomenclature for all the NENs of the GI tract (stomach, small and large intestine, rectum) and pancreas.[2] On the basis of clinical behavior, histology, and proliferation rate, NENs are divided into two groups: well-differentiated NENs and poorly differentiated (high grade) neuroendocrine carcinomas (NECs).[3] While often considered to be rare, the incidence of this tumor is on the rise in India and abroad.[4],[5],[6] This increase has been mirrored by a corresponding improvement in survival.[7] Some of this increased incidence may reflect better detection rates. Most of the prevalence and descriptive studies from India are from tertiary referral centers, with a lack of population-based data.
Given the increased incidence of these tumors, it is important for us to better understand their biology and behavior as this will enable us to manage them appropriately.
GEP-NENs account for more than 60% of all NENs (29.664 out of 49.012 patients) according to the surveillance, epidemiology, and end-results program database[3] and based on data from India.[8],[9] The most common site for GEP-NENs in most databases is the rectum, followed by the small intestine and colon.[4],[10]
The APNET registry is a longitudinal observational registry of patients with GEP-NENs in India, with six participating centers. Over 277 patients have been recruited by the APNET registry. Like other geographical regions, there is a slight male predominance in India. The most common site of GEP-NENs is the pancreas (44%), followed by duodenum and stomach (10%) and rectum (7%). The primary tumor site was unknown in 8% of patients. Eleven percent of all tumors were functional, with insulinomas being the most common.[11] Ten percent of the tumors were Grade 3 (G3) carcinomas. Rectal NENs have the best 5-year survival rates,[5],[10] while pancreatic NENs are more likely to present with metastases.[4],[8]
Indian data[8],[12] have indicated that pancreatic NENs, despite being the most common site for GEP-NENs, are an uncommon subset among pathological malignant lesions of the pancreas. Patients with MEN-1 or von Hippel-Lindau syndrome tend to present 15–20 years earlier than patients with sporadic NENs.[7]
Purpose
Although international guidelines are available for the management of GEP-NENs, it is not entirely feasible to apply these guidelines to the Indian population owing to differences in the incidence of the disease in different parts of India, varying socioeconomic factors, and availability of resources. Therefore, it is essential to analyze the evidence pertaining to GEP-NENs from India and the rest of the world[13] with an aim to formulate evidence-based guidelines that could be applicable to Indian patients.
Taking into consideration peripheral oncology centers, regional cancer centers, and tertiary cancer centers in major cities, the set of recommendations includes two categories as follows:
Desirable/ideal
Tests and treatments that may not be available at all centers, but the centers should aspire to have them in the near future.
Essential
The bare minimum that should be offered to all the patients by all the centers treating cancer patients.
Diagnosis and Staging
The diagnosis of a GEP-NEN is based on the clinical symptoms, biochemical tests, imaging modalities, and most importantly, histopathology. Most GEP-NENs are incidentally detected as they are largely nonfunctional. Depending on the location, patients may present with GI bleeding, bowel obstruction (due to intussusception), or acute appendicitis. The functional lesions produce characteristic syndrome complexes. Some examples of these include the following: insulinomas secrete insulin, resulting in neuroglycopenic symptoms. Patients with gastrinomas present with recurrent or refractory peptic ulcers and dyspepsia, usually with diarrhea. Glucagonomas are associated with the development of diabetes mellitus, weight loss, and cachexia, and/or migratory necrolytic erythema. Patients with somatostatinomas have diabetes mellitus and/or diarrhea/steatorrhoea. VIPomas are characterized by watery diarrhea, hypokalemia, and achlorhydria syndrome.
Obtaining a biopsy is essential not only to establish the diagnosis but also to know the grade of the tumor, which plays the most crucial role in deciding management. GEP-NENs are a heterogeneous group of tumors that share a common phenotype, with immunoreactivity for pan-neuroendocrine markers such as chromogranin A (CgA), synaptophysin, neuron-specific enolase (NSE), and CD56. However, GEP-NENs arising in different anatomical sites differ in their biology and clinical presentation. Lung origin may be favored by positive staining for thyroid transcription factor 1, intestinal or pancreatic origin by CDX2, and pancreatic or rectal origin by IsI1 and PAX8 staining.[14],[15]
The evaluation of GEP-NENs should include:
Site of origin
Any locoregional or metastatic spread (stage)
Grade of the tumor
Functional status of the tumor and biomarker levels. The biomarkers can be nonspecific like serum CgA, NSE, pancreatic polypeptide or specific like insulin, glucagon, gastrin, vasoactive intestinal peptide, somatostatin, urinary 5-HIAA, or serotonin[16]
Somatostatin receptor (SSTR) expression
Association with known syndromes.
Staging of gastroenteropancreatic neuroendocrine neoplasms
The European Neuroendocrine Tumour Society and the American Joint Cancer Committee have proposed a TNM staging system for the different GEP-NENs.[17],[18] GEP-NENs of the stomach, small intestine, colon/rectum, appendix, and pancreas have separate staging systems. Tumor stage, particularly the presence or absence of lymph node or distant metastasis, has the strongest effect on survival.[19] Multidetector computed tomography (MDCT), or magnetic resonance imaging (MRI) scans are often the initial investigations performed for staging GEP-NENs, in which these tumors appear hypervascular along with nuclear imaging techniques (Gallium 68 DOTA scan and/or Fluorodeoxyglucose positron emission tomography [FDG-PET] scan). Endoscopic Ultrasound can be used to define the depth of mural extension and for obtaining tissue samples from deep-seated lesions.
Grading of gastroenteropancreatic neuroendocrine neoplasms
Immunohistochemistry (IHC) estimation of the Ki-67 expression and mitotic index count are used to grade GEP-NENs [Table 1], as per the World Health Organization (WHO) classification [Table 2], into low-grade (G1), intermediate-grade (G2), and high-grade (G3) categories.[2] The G1 and G2 NENs correspond to well-differentiated tumors on morphology, and the G3 NENs to poorly differentiated NECs as per the WHO 2010 classification. However, since the emerging evidence suggested that the G3 pancreatic NEN are heterogeneous in morphology and biology, the recent WHO 2017 classification has introduced a new category of well-differentiated pancreatic neuroendocrine tumors (WD-pNETs) G3, that show lower response rate to platinum-based chemotherapy while better outcomes compared with poorly differentiated pancreatic NECs (PD-pNECs) G3.[20] These NEC can be of small- or large-cell type. The most common sites for extra-pulmonary GEP-NEC are esophagus, rectum, or colon. NECs are rarely associated with a hormonal syndrome.
Functional status
Functional status is based on clinical features of hormone over-secretion, and not by in vitro demonstration of hormonal production by IHC. While the IHC may be positive for multiple hormones on biopsy samples, it is not indicative of functionality. Patients with pancreatic NENs (pNENs) may have symptoms due to the secretion of insulin, glucagon, gastrin, and other peptides. Functional NENs can cause significant symptoms even when small and may be difficult to identify by imaging tests. Biochemical testing is dictated by the clinical symptoms.
Patients with NEN that have metastasized to the liver may have symptoms of episodic flushing and/or diarrhea (carcinoid syndrome). Carcinoid syndrome is related to the secretion of serotonin, histamine, and tachykinins directly into the systemic circulation, bypassing liver metabolism. Rarely, carcinoid syndrome can develop owing to functioning retroperitoneal metastases.
Imaging
The role of imaging for GEP-NENs is in aiding the initial diagnosis, planning management, and in the follow-up after treatment. The role of the radiologist is to determine the exact site of primary tumor, to assess its resectability, to map the metastatic burden, and to find out any complication due to local or metastatic disease. To elucidate this much information, there is a need for the combination of many imaging techniques. Primary NENs are usually small in size and arise in the submucosal layer of the bowel wall, or within the pancreas. These may be multiple and may occur at different sites simultaneously.[21]
MDCT is the initial imaging modality for localization of the primary tumor, staging the disease, and assessing its resectability. Nuclear scanning techniques such as Indium 111 (111 In) octreotide scintigraphy or PET using gallium 68 (most preferred)[22] are complementary to CT scan and are useful in detecting additional sites of disease, or to help localize an undetected primary on conventional CT scan. MRI may be considered for patients CT contrast allergy, or in those who have abnormal renal functions. Video capsule endoscopy, double-balloon enteroscopy, and CT enterography may be used for the evaluation of the primary tumor if the facilities are available and to support the previously mentioned investigations.
Multidisciplinary Treatment for Early Disease [Algorithm 1][INLINE:1]
A multidisciplinary team approach remains at the core of treating all cancers such treatment relies on an effective interdisciplinary network including surgical, medical, and radiation oncologists; gastroenterologists; pathologists; radiologists (for interventional and nuclear medicine); nurse specialists, and palliative care physicians.
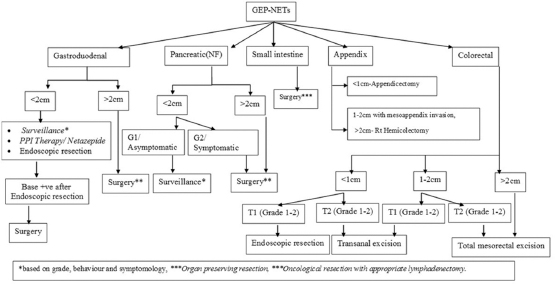
| Algorithm 1: The management of gastroenteropancreatic neuroendocrine neoplasms with locoregional disease
All new patients should be discussed at a tumor board or interdisciplinary team meeting, and the treatment strategy should be confirmed based on a complete workup of the patient. In most patients with localized disease, resection will be the treatment of choice.
Surgical Principles for the Management of Gastroenteropancreatic Neuroendocrine Neoplasms
Prior to surgery, all symptoms of hormonal excess must be treated. Octreotide or lanreotide can be considered for symptom control in most pNENs, although caution is advised in patients with an insulinoma as the medication can worsen hypoglycemia, resulting in fatal complications. For insulinomas, adequate glycemic control should be achieved with diet, diazoxide and/or Everolimus. Gastrin hypersecretion in patients with gastrinomas can be controlled with proton pump inhibitors. Patients with glucagonoma also need good glycemic control
Resection should include complete removal of the tumor with negative margins along with regional lymphadenectomy
A thorough exploration to detect synchronous primary tumors should be performed as their incidence is 15%–30%
Cholecystectomy is recommended when performing surgery for advanced NENs in patients anticipated to receive long-term octreotide therapy, as these patients are at higher risk of developing biliary symptoms and cholecystitis
In patients with functional carcinoid tumors, Octreotide therapy should be administered parenterally prior to induction of anesthesia to prevent carcinoid crisis
All patients who might require a splenectomy should preoperatively receive the trivalent vaccine (i.e. pneumococcus, hemophilus influenzae b, meningococcal group C).
Multidisciplinary Treatment for Gastroenteropancreatic Neuroendocrine Neoplasms (Including Metastatic Disease
Overall, the prognosis of GEP-NENs remains good and largely depends on the stage and grade of the tumor. The prognosis for GEP-NEC is poor for all stages of disease with a median survival (from the time of diagnosis) of 38 months for localized disease, 16 months for regional disease, and 5 months for metastatic disease.[23],[24],[25],[26] Long-term relapse-free survival is possible among patients with localized disease who are treated with multimodality therapy.
General approach [Algorithm 2][INLINE:2]
Unfortunately, most patients will present with metastatic disease not amenable to resection. However, when a complete resection of primary, as well as, the metastatic disease is possible in G1/G2 tumors, surgery remains the treatment of choice and can lead to cure.[27] In advanced G3 tumor NEC or advanced G1/G2 tumor NETs (relabeled as NENs), where R0 resection is not possible, the intent of treatment remains achieving palliation of symptoms and improvement in progression-free survival. Many patients will benefit in terms of both quality of life and survival from the use of systemic chemotherapy and supportive measures.
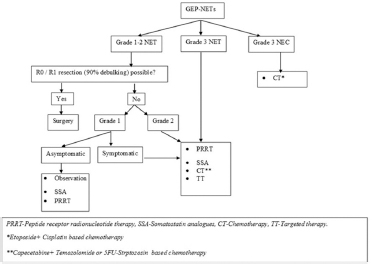
| Algorithm 2: The management of advanced/metastatic/recurrent gastroenteropancreatic neuroendocrine neoplasms
Data to support the current treatment of GEP-NEC is based on retrospective reports and parallel recommendations from small cell carcinomas of the lung. GEP-NECs respond to systemic chemotherapy, and platinum-based chemotherapy represents the backbone of treatment for advanced-stage GEP-NEC, especially if the Ki67 is more than 55%.[24],[28],[29],[30],[31],[32]
Somatostatin analogs
Octreotide and lanreotide are the commonly used SSAs in GEP-NENs for symptom control. In addition to symptom control, octreotide also has antiproliferative and anticancer effects in NENs and can improve progression-free survival.[33],[34] Currently, there is no evidence to suggest the superiority of octreotide over lanreotide and vice versa. In addition, it is unclear whether treatment with SSAs is better than “watch-and-wait” approach in patients with very slow-growing disease.
Peptide receptor radionuclide therapy
PRRT is a form of systemic radionuclide-based treatment and is highly effective when tumors have high SSTR [removed]specifically SSTR2). Yttrium-90 (90Y) and Lutetium-177 (177 Lu) are the most commonly used radioisotopes for delivering PRRT. This therapy has also been shown to be effective in patients who progress on long-acting SST therapy and can achieve significant symptom control and even improve survival.[35] PRRT with 177Lu-DOTATATE is generally well tolerated, with the most common adverse events being renal insufficiency and bone marrow suppression. Currently, PRRT is indicated for use in advanced SSTR positive, well-differentiated GEP-NENs, in combination, or as an alternative to SST analogs. Another emerging strategy in a higher grade (G2/G3) GEP-NENs, is the combination of capecitabine and temozolomide chemotherapy with PRRT (Chemo-PRRT), especially with tumors demonstrating an uptake on Gallium as well as FDG-PET scan (dual scan). However, this approach is still investigational.[36]
Adjuvant therapy
Adjuvant or neoadjuvant chemoradiation is reasonable if the risk of local recurrence is thought to be higher than average, depending on the anatomic location of the tumor (e.g., rectum).
Systemic chemotherapy and targeted therapy [Table 3] [34],[37],[38],[39],[40],[41],[42],[43],[44]
Systemic Chemotherapy: In advanced, metastatic G3 NECs, cisplatin, and etoposide combination chemotherapy is the first line of treatment[45] and is associated with rapid responses. However, the remissions are often of short duration. Furthermore, the response rates are dependent on the Ki-67 index-higher the index, higher is the response to platinum-based chemotherapy.[41] FOLFIRI (folinic acid, 5-fluorouracil/5-FU, and irinotecan) or FOLFIRINOX (folinic acid, fluorouracil, oxaliplatin, and irinotecan) can be used as a second line, after disease progression and have been shown to have varying response rates.[38]
Table 3 Medical management for gastroenteropancreatic neuroendocrine neoplasms
G1-3 GEP-NENs that do not respond to or progress on, other modalities can be treated with cytotoxic chemotherapy with streptozocin, 5-FU, temozolomide, or Capecitabine.
Targeted therapy: Everolimus, an mTOR pathway inhibitor, is approved for advanced, progressive, well-differentiated, non-functioning GEP-NENs.[43],[44] However, due to significant adverse effects such as neutropenia, infections, rash, diarrhea, and hyperglycemia, it is currently reserved for patients with significant progression of disease on other modalities. Sunitinib, a tyrosine kinase inhibitor, is also approved for use in advanced pNENs.[40]
Relapsed or progressive disease
There are little data on second-line therapy (and no studies comparing chemotherapy versus best supportive care), and no standard regimen has been established. Patients who progress more than 3 months after discontinuation of first-line treatment may still be platinum-sensitive. However, the other second and third-line systemic chemotherapy or targeted therapies may be used as mentioned above.
Given the tumor expression of programmed cell death ligand 1 (PD-L1)/PD protein 1 (PD-1) in patients with GEP-NEN, immunotherapy may play a role in the treatment of patients with GEP-NEN.[46]
Follow-Up and Rehabilitation
Patients should be encouraged to maintain lead a healthy lifestyle and abstain from tobacco and alcohol. The aim of the follow-up is to detect recurrences early as well as to assess any complication due to surgery/radiotherapy. Postsurgery, the follow-up is done every 3–4 months for the 1st year with each visit comprised of clinical examination (including history and physical examination). The follow-up in years 2–3 is every 6 months and annually, thereafter till year 5. At the end of each of the first 3 years, a CT scan of the chest, abdomen, and pelvis is recommended. For patients with advanced GEP-NENs, the scans are symptom-driven or for response assessment.
References
- Modlin IM, Oberg K, Chung DC, Jensen RT, de Herder WW, Thakker RV. et al. Gastroenteropancreatic neuroendocrine tumours. Lancet Oncol 2008; 9: 61-72
- Rindi G, Arnold R, Bosman F, Capella C, Klimstra D, Kloppel G. et al. Nomenclature and classification of neuroendocrine neoplasms of the digestive system. In: Bosman F, Carneiro F, Hruban R, Theise N. editors WHO Classification of Tumours of the Digestive System. Lyon: IARC Press; 2010: 13-4
- Bosman FT, Carneiro F, Hruban RH, Theise ND. World Health Organization Classification of Tumours of the Digestive System. 4th ed. Geneva, Switzerland: World Health Organization Press; 2010
- Lawrence B, Gustafsson BI, Chan A, Svejda B, Kidd M, Modlin IM. The epidemiology of gastroenteropancreatic neuroendocrine tumors. Endocrinol Metab Clin North Am 2011; 40: 1-18 vii
- Hauso O, Gustafsson BI, Kidd M, Waldum HL, Drozdov I, Chan AK. et al. Neuroendocrine tumor epidemiology: Contrasting Norway and North America. Cancer 2008; 113: 2655-64
- Ito T, Igarashi H, Nakamura K, Sasano H, Okusaka T, Takano K. et al. Epidemiological trends of pancreatic and gastrointestinal neuroendocrine tumors in Japan: A nationwide survey analysis. J Gastroenterol 2015; 50: 58-64
- Yao JC, Hassan M, Phan A, Dagohoy C, Leary C, Mares JE. et al. One hundred years after “carcinoid”: Epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol 2008; 26: 3063-72
- Amarapurkar DN, Juneja MP, Patel ND, Amarapurkar AD, Amarapurkar PD. A retrospective clinico-pathological analysis of neuroendocrine tumors of the gastrointestinal tract. Trop Gastroenterol 2010; 31: 101-4
- Palepu J, Shrikhande SV, Bhaduri D, Shah RC, Sirohi B, Chhabra V. et al. Trends in diagnosis of gastroenteropancreatic neuroendocrine tumors (GEP-NETs) in India: A report of multicenter data from a web-based registry. Indian J Gastroenterol 2017; 36: 445-51
- Tsai HJ, Wu CC, Tsai CR, Lin SF, Chen LT, Chang JS. The epidemiology of neuroendocrine tumors in Taiwan: A nation-wide cancer registry-based study. PLoS One 2013; 8: e62487
- Desjardins A. Technique de la pancreatectomie. Rev Chir Paris 1907; 35: 945
- Belachew M, Zimmermann JM. Evolution of a paradigm for laparoscopic adjustable gastric banding. Am J Surg 2002; 184: 21S-5S
- Steinmüller T, Kianmanesh R, Falconi M, Scarpa A, Taal B, Kwekkeboom DJ. et al. Consensus guidelines for the management of patients with liver metastases from digestive (neuro) endocrine tumors: Foregut, midgut, hindgut, and unknown primary. Neuroendocrinology 2008; 87: 47-62
- Klimstra DS, Modlin IR, Coppola D, Lloyd RV, Suster S. The pathologic classification of neuroendocrine tumors: A review of nomenclature, grading, and staging systems. Pancreas 2010; 39: 707-12
- Toouli J, Kow L, Ramos AC, Aigner F, Pattyn P, Galvão-Neto MP. et al. International multicenter study of safety and effectiveness of Swedish adjustable gastric band in 1-, 3-, and 5-year follow-up cohorts. Surg Obes Relat Dis 2009; 5: 598-609
- Sansone A, Lauretta R, Vottari S, Chiefari A, Barnabei A, Romanelli F. et al. Specific and non-specific biomarkers in neuroendocrine gastroenteropancreatic tumors. Cancers (Basel) 2019; 11: E1113
- Sundin A, Vullierme MP, Kaltsas G, Plöckinger U. Mallorca Consensus Conference participants, European Neuroendocrine Tumor Society. ENETS consensus guidelines for the standards of care in neuroendocrine tumors: Radiological examinations. Neuroendocrinology 2009; 90: 167-83
- Edge S, Byrd D, Compton C, Fritz AG, Greene F, Trotti A. editors AJCC Cancer Staging Manual. 7th ed. New York: Springer Verlag; 2009
- Whipple AO. The rationale of radical surgery for cancer of the pancreas and ampullary region. Ann Surg 1941; 114: 612-5
- Lloyd R, Osamura R, Kloppel G, Rosai J. WHO Classification of Tumours of Endocrine Organs. Lyon, France: IARC Press; 2017
- Megibow AJ. Update in imaging of cystic pancreatic masses for gastroenterologists. Clin Gastroenterol Hepatol 2008; 6: 1194-7
- Coffey XVII RC. Pancreato-enterostomy and pancreatectomy: A preliminary report. Ann Surg 1909; 50: 1238-64
- Xia BT, Fu B, Wang J, Kim Y, Ahmad SA, Dhar VK. et al. Does radiologic response correlate to pathologic response in patients undergoing neoadjuvant therapy for borderline resectable pancreatic malignancy?. J Surg Oncol 2017; 115: 376-83
- Vakalopoulos KA, Daams F, Wu Z, Timmermans L, Jeekel JJ, Kleinrensink GJ. et al. Tissue adhesives in gastrointestinal anastomosis: A systematic review. J Surg Res 2013; 180: 290-300
- Suker M, Beumer BR, Sadot E, Marthey L, Faris JE, Mellon EA. et al. FOLFIRINOX for locally advanced pancreatic cancer: A systematic review and patient-level meta-analysis. Lancet Oncol 2016; 17: 801-10
- Veldhuisen E, Vogel J, Busch O, Lienden K, Hanneke W. CA19-9 response combined with CT-imaging accurately predicts resectability of locally advanced pancreatic carcinoma following neoadjuvant chemotherapy. Pancreatology 2017; 17: S38-9
- Gaikwad V, Patkar S, Barreto SG, Sirohi B, Goel M, Shrikhande SV. Outcomes of 101 consecutive surgical resections of gastroenteropancreatic neuroendocrine tumours (GEPNETs) at tata memorial hospital: A referral bias for nonfunctional duodenopancreatic tumours and the need for greater awareness of GEPNETs as a distinct entity. Indian J Surg 2017; 79: 226-33
- Ramia JM, de la Plaza R, Adel F, Ramiro C, Arteaga V, Garcia-Parreño J. Wrapping in pancreatic surgery: A systematic review. ANZ J Surg 2014; 84: 921-4
- Zhang X, Dong X, Liu P, Yan Y, Wei Y, Zechner D. et al. Binding versus conventional pancreaticojejunostomy in preventing postoperative pancreatic fistula: A Systematic review and meta-analysis. Dig Surg 2017; 34: 265-80
- Gong J, He S, Cheng Y, Cheng N, Gong J, Zeng Z. Fibrin sealants for the prevention of postoperative pancreatic fistula following pancreatic surgery. Cochrane Database Syst Rev 2018; 6: CD009621
- Shrikhande SV, Sivasanker M, Vollmer CM, Friess H, Besselink MG, Fingerhut A. et al. Pancreatic anastomosis after pancreatoduodenectomy: A position statement by the international study group of pancreatic surgery (ISGPS). Surgery 2017; 161: 1221-34
- Ecker BL, McMillan MT, Asbun HJ, Ball CG, Bassi C, Beane JD. et al. Characterization and optimal management of high-risk pancreatic anastomoses during pancreatoduodenectomy. Ann Surg 2018; 267: 608-16
- Shojamanesh H, Gibril F, Louie A, Ojeaburu JV, Bashir S, Abou-Saif A. et al. Prospective study of the antitumor efficacy of long-term octreotide treatment in patients with progressive metastatic gastrinoma. Cancer 2002; 94: 331-43
- Rinke A, Müller HH, Schade-Brittinger C, Klose KJ, Barth P, Wied M. et al. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors: A report from the PROMID study group. J Clin Oncol 2009; 27: 4656-63
- Strosberg J, Wolin E, Chasen B, Kulke M, Bushnell D, Caplin M. et al. Health-related quality of life in patients with progressive midgut neuroendocrine tumors treated with177 Lu-dotatate in the phase III NETTER-1 trial. J Clin Oncol 2018; 36: 2578-84
- Kesavan M, Claringbold PG, Turner JH. Hematological toxicity of combined 177Lu-octreotate radiopeptide chemotherapy of gastroenteropancreatic neuroendocrine tumors in long-term follow-up. Neuroendocrinology 2014; 99: 108-17
- Caplin ME, Pavel M, Ćwikła JB, Phan AT, Raderer M, Sedláčková E. et al. Lanreotide in metastatic enteropancreatic neuroendocrine tumors. N Engl J Med 2014; 371: 224-33
- Hentic O, Hammel P, Couvelard A, Rebours V, Zappa M, Palazzo M. et al. FOLFIRI regimen: An effective second-line chemotherapy after failure of etoposide-platinum combination in patients with neuroendocrine carcinomas grade 3. Endocr Relat Cancer 2012; 19: 751-7
- Moertel CG, Lefkopoulo M, Lipsitz S, Hahn RG, Klaassen D. Streptozocin-doxorubicin, streptozocin-fluorouracil or chlorozotocin in the treatment of advanced islet-cell carcinoma. N Engl J Med 1992; 326: 519-23
- Raymond E, Dahan L, Raoul JL, Bang YJ, Borbath I, Lombard-Bohas C. et al. Sunitinib malate for the treatment of pancreatic neuroendocrine tumors. N Engl J Med 2011; 364: 501-13
- Sorbye H, Welin S, Langer SW, Vestermark LW, Holt N, Osterlund P. et al. Predictive and prognostic factors for treatment and survival in 305 patients with advanced gastrointestinal neuroendocrine carcinoma (WHO G3): The NORDIC NEC study. Ann Oncol 2013; 24: 152-60
- Strosberg JR, Fine RL, Choi J, Nasir A, Coppola D, Chen DT. et al. First-line chemotherapy with capecitabine and temozolomide in patients with metastatic pancreatic endocrine carcinomas. Cancer 2011; 117: 268-75
- Yao JC, Fazio N, Singh S, Buzzoni R, Carnaghi C, Wolin E. et al. Everolimus for the treatment of advanced, non-functional neuroendocrine tumours of the lung or gastrointestinal tract (RADIANT-4): A randomised, placebo-controlled, phase 3 study. Lancet 2016; 387: 968-77
- Yao JC, Shah MH, Ito T, Bohas CL, Wolin EM, Van Cutsem E. et al. Everolimus for advanced pancreatic neuroendocrine tumors. N Engl J Med 2011; 364: 514-23
- Iwasa S, Morizane C, Okusaka T, Ueno H, Ikeda M, Kondo S. et al. Cisplatin and etoposide as first-line chemotherapy for poorly differentiated neuroendocrine carcinoma of the hepatobiliary tract and pancreas. Jpn J Clin Oncol 2010; 40: 313-8
- Wang C, Yu J, Fan Y, Ma K, Ning J, Hu Y. et al. The clinical significance of PD-L1/PD-1 expression in gastroenteropancreatic neuroendocrine neoplasia. Ann Clin Lab Sci 2019; 49: 448-56
Address for correspondence
Publication History
Received: 04 August 2019
Accepted: 24 October 2019
Article published online:
23 May 2021
© 2020. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
References
- Modlin IM, Oberg K, Chung DC, Jensen RT, de Herder WW, Thakker RV. et al. Gastroenteropancreatic neuroendocrine tumours. Lancet Oncol 2008; 9: 61-72
- Rindi G, Arnold R, Bosman F, Capella C, Klimstra D, Kloppel G. et al. Nomenclature and classification of neuroendocrine neoplasms of the digestive system. In: Bosman F, Carneiro F, Hruban R, Theise N. editors WHO Classification of Tumours of the Digestive System. Lyon: IARC Press; 2010: 13-4
- Bosman FT, Carneiro F, Hruban RH, Theise ND. World Health Organization Classification of Tumours of the Digestive System. 4th ed. Geneva, Switzerland: World Health Organization Press; 2010
- Lawrence B, Gustafsson BI, Chan A, Svejda B, Kidd M, Modlin IM. The epidemiology of gastroenteropancreatic neuroendocrine tumors. Endocrinol Metab Clin North Am 2011; 40: 1-18 vii
- Hauso O, Gustafsson BI, Kidd M, Waldum HL, Drozdov I, Chan AK. et al. Neuroendocrine tumor epidemiology: Contrasting Norway and North America. Cancer 2008; 113: 2655-64
- Ito T, Igarashi H, Nakamura K, Sasano H, Okusaka T, Takano K. et al. Epidemiological trends of pancreatic and gastrointestinal neuroendocrine tumors in Japan: A nationwide survey analysis. J Gastroenterol 2015; 50: 58-64
- Yao JC, Hassan M, Phan A, Dagohoy C, Leary C, Mares JE. et al. One hundred years after “carcinoid”: Epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol 2008; 26: 3063-72
- Amarapurkar DN, Juneja MP, Patel ND, Amarapurkar AD, Amarapurkar PD. A retrospective clinico-pathological analysis of neuroendocrine tumors of the gastrointestinal tract. Trop Gastroenterol 2010; 31: 101-4
- Palepu J, Shrikhande SV, Bhaduri D, Shah RC, Sirohi B, Chhabra V. et al. Trends in diagnosis of gastroenteropancreatic neuroendocrine tumors (GEP-NETs) in India: A report of multicenter data from a web-based registry. Indian J Gastroenterol 2017; 36: 445-51
- Tsai HJ, Wu CC, Tsai CR, Lin SF, Chen LT, Chang JS. The epidemiology of neuroendocrine tumors in Taiwan: A nation-wide cancer registry-based study. PLoS One 2013; 8: e62487
- Desjardins A. Technique de la pancreatectomie. Rev Chir Paris 1907; 35: 945
- Belachew M, Zimmermann JM. Evolution of a paradigm for laparoscopic adjustable gastric banding. Am J Surg 2002; 184: 21S-5S
- Steinmüller T, Kianmanesh R, Falconi M, Scarpa A, Taal B, Kwekkeboom DJ. et al. Consensus guidelines for the management of patients with liver metastases from digestive (neuro) endocrine tumors: Foregut, midgut, hindgut, and unknown primary. Neuroendocrinology 2008; 87: 47-62
- Klimstra DS, Modlin IR, Coppola D, Lloyd RV, Suster S. The pathologic classification of neuroendocrine tumors: A review of nomenclature, grading, and staging systems. Pancreas 2010; 39: 707-12
- Toouli J, Kow L, Ramos AC, Aigner F, Pattyn P, Galvão-Neto MP. et al. International multicenter study of safety and effectiveness of Swedish adjustable gastric band in 1-, 3-, and 5-year follow-up cohorts. Surg Obes Relat Dis 2009; 5: 598-609
- Sansone A, Lauretta R, Vottari S, Chiefari A, Barnabei A, Romanelli F. et al. Specific and non-specific biomarkers in neuroendocrine gastroenteropancreatic tumors. Cancers (Basel) 2019; 11: E1113
- Sundin A, Vullierme MP, Kaltsas G, Plöckinger U. Mallorca Consensus Conference participants, European Neuroendocrine Tumor Society. ENETS consensus guidelines for the standards of care in neuroendocrine tumors: Radiological examinations. Neuroendocrinology 2009; 90: 167-83
- Edge S, Byrd D, Compton C, Fritz AG, Greene F, Trotti A. editors AJCC Cancer Staging Manual. 7th ed. New York: Springer Verlag; 2009
- Whipple AO. The rationale of radical surgery for cancer of the pancreas and ampullary region. Ann Surg 1941; 114: 612-5
- Lloyd R, Osamura R, Kloppel G, Rosai J. WHO Classification of Tumours of Endocrine Organs. Lyon, France: IARC Press; 2017
- Megibow AJ. Update in imaging of cystic pancreatic masses for gastroenterologists. Clin Gastroenterol Hepatol 2008; 6: 1194-7
- Coffey XVII RC. Pancreato-enterostomy and pancreatectomy: A preliminary report. Ann Surg 1909; 50: 1238-64
- Xia BT, Fu B, Wang J, Kim Y, Ahmad SA, Dhar VK. et al. Does radiologic response correlate to pathologic response in patients undergoing neoadjuvant therapy for borderline resectable pancreatic malignancy?. J Surg Oncol 2017; 115: 376-83
- Vakalopoulos KA, Daams F, Wu Z, Timmermans L, Jeekel JJ, Kleinrensink GJ. et al. Tissue adhesives in gastrointestinal anastomosis: A systematic review. J Surg Res 2013; 180: 290-300
- Suker M, Beumer BR, Sadot E, Marthey L, Faris JE, Mellon EA. et al. FOLFIRINOX for locally advanced pancreatic cancer: A systematic review and patient-level meta-analysis. Lancet Oncol 2016; 17: 801-10
- Veldhuisen E, Vogel J, Busch O, Lienden K, Hanneke W. CA19-9 response combined with CT-imaging accurately predicts resectability of locally advanced pancreatic carcinoma following neoadjuvant chemotherapy. Pancreatology 2017; 17: S38-9
- Gaikwad V, Patkar S, Barreto SG, Sirohi B, Goel M, Shrikhande SV. Outcomes of 101 consecutive surgical resections of gastroenteropancreatic neuroendocrine tumours (GEPNETs) at tata memorial hospital: A referral bias for nonfunctional duodenopancreatic tumours and the need for greater awareness of GEPNETs as a distinct entity. Indian J Surg 2017; 79: 226-33
- Ramia JM, de la Plaza R, Adel F, Ramiro C, Arteaga V, Garcia-Parreño J. Wrapping in pancreatic surgery: A systematic review. ANZ J Surg 2014; 84: 921-4
- Zhang X, Dong X, Liu P, Yan Y, Wei Y, Zechner D. et al. Binding versus conventional pancreaticojejunostomy in preventing postoperative pancreatic fistula: A Systematic review and meta-analysis. Dig Surg 2017; 34: 265-80
- Gong J, He S, Cheng Y, Cheng N, Gong J, Zeng Z. Fibrin sealants for the prevention of postoperative pancreatic fistula following pancreatic surgery. Cochrane Database Syst Rev 2018; 6: CD009621
- Shrikhande SV, Sivasanker M, Vollmer CM, Friess H, Besselink MG, Fingerhut A. et al. Pancreatic anastomosis after pancreatoduodenectomy: A position statement by the international study group of pancreatic surgery (ISGPS). Surgery 2017; 161: 1221-34
- Ecker BL, McMillan MT, Asbun HJ, Ball CG, Bassi C, Beane JD. et al. Characterization and optimal management of high-risk pancreatic anastomoses during pancreatoduodenectomy. Ann Surg 2018; 267: 608-16
- Shojamanesh H, Gibril F, Louie A, Ojeaburu JV, Bashir S, Abou-Saif A. et al. Prospective study of the antitumor efficacy of long-term octreotide treatment in patients with progressive metastatic gastrinoma. Cancer 2002; 94: 331-43
- Rinke A, Müller HH, Schade-Brittinger C, Klose KJ, Barth P, Wied M. et al. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors: A report from the PROMID study group. J Clin Oncol 2009; 27: 4656-63
- Strosberg J, Wolin E, Chasen B, Kulke M, Bushnell D, Caplin M. et al. Health-related quality of life in patients with progressive midgut neuroendocrine tumors treated with177 Lu-dotatate in the phase III NETTER-1 trial. J Clin Oncol 2018; 36: 2578-84
- Kesavan M, Claringbold PG, Turner JH. Hematological toxicity of combined 177Lu-octreotate radiopeptide chemotherapy of gastroenteropancreatic neuroendocrine tumors in long-term follow-up. Neuroendocrinology 2014; 99: 108-17
- Caplin ME, Pavel M, Ćwikła JB, Phan AT, Raderer M, Sedláčková E. et al. Lanreotide in metastatic enteropancreatic neuroendocrine tumors. N Engl J Med 2014; 371: 224-33
- Hentic O, Hammel P, Couvelard A, Rebours V, Zappa M, Palazzo M. et al. FOLFIRI regimen: An effective second-line chemotherapy after failure of etoposide-platinum combination in patients with neuroendocrine carcinomas grade 3. Endocr Relat Cancer 2012; 19: 751-7
- Moertel CG, Lefkopoulo M, Lipsitz S, Hahn RG, Klaassen D. Streptozocin-doxorubicin, streptozocin-fluorouracil or chlorozotocin in the treatment of advanced islet-cell carcinoma. N Engl J Med 1992; 326: 519-23
- Raymond E, Dahan L, Raoul JL, Bang YJ, Borbath I, Lombard-Bohas C. et al. Sunitinib malate for the treatment of pancreatic neuroendocrine tumors. N Engl J Med 2011; 364: 501-13
- Sorbye H, Welin S, Langer SW, Vestermark LW, Holt N, Osterlund P. et al. Predictive and prognostic factors for treatment and survival in 305 patients with advanced gastrointestinal neuroendocrine carcinoma (WHO G3): The NORDIC NEC study. Ann Oncol 2013; 24: 152-60
- Strosberg JR, Fine RL, Choi J, Nasir A, Coppola D, Chen DT. et al. First-line chemotherapy with capecitabine and temozolomide in patients with metastatic pancreatic endocrine carcinomas. Cancer 2011; 117: 268-75
- Yao JC, Fazio N, Singh S, Buzzoni R, Carnaghi C, Wolin E. et al. Everolimus for the treatment of advanced, non-functional neuroendocrine tumours of the lung or gastrointestinal tract (RADIANT-4): A randomised, placebo-controlled, phase 3 study. Lancet 2016; 387: 968-77
- Yao JC, Shah MH, Ito T, Bohas CL, Wolin EM, Van Cutsem E. et al. Everolimus for advanced pancreatic neuroendocrine tumors. N Engl J Med 2011; 364: 514-23
- Iwasa S, Morizane C, Okusaka T, Ueno H, Ikeda M, Kondo S. et al. Cisplatin and etoposide as first-line chemotherapy for poorly differentiated neuroendocrine carcinoma of the hepatobiliary tract and pancreas. Jpn J Clin Oncol 2010; 40: 313-8
- Wang C, Yu J, Fan Y, Ma K, Ning J, Hu Y. et al. The clinical significance of PD-L1/PD-1 expression in gastroenteropancreatic neuroendocrine neoplasia. Ann Clin Lab Sci 2019; 49: 448-56


 PDF
PDF  Views
Views  Share
Share

