Knowledge, attitudes and practice toward cervical cancer screening among Sikkimese nursing staff in India
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2015; 36(02): 105-110
DOI: DOI: 10.4103/0971-5851.158840
Abstract
Objectives: To assess baseline knowledge of cancer cervix, screening and practice of Pap smear screening among Sikkimese staff nurses in India. Materials and Methods: Between April 2012 and February 2013, a predesigned, pretested, self -administered multiple responses questionnaire survey was conducted among staff nurses′ working in various hospitals of Sikkim. Questionnaire contained information about their demographics, knowledge of cervical cancer, its risk factors, screening methods, attitudes toward cervical cancer screening and practice of Pap smear amongst themselves. Results: Overall, 90.4% nurses responded that they were aware of cancer cervix. Three quarter of the staff nurses were not aware of commonest site being cancer cervix in women. Of the 320 participants, who had heard of cancer cervix, 253 (79.1%) were aware of cancer cervix screening. Pap smear screening should start at 21 years or 3 years after sexual debut was known to only one-third of the nursing staff. Age was found to be a significant predictor of awareness of Pap smear screening among nursing staff. Awareness was significantly more prevalent among older staff (P < 0.007). Married nursing staffs were significantly more likely to be aware of screening methods, and nursing staff of Christian and Buddhist religion were 1.25 times and 2.03 times more likely to aware of screening methods than Hindu religion respectively. Only 16.6% nurses, who were aware of a Pap smear (11.9% of the total sample), had ever undergone a Pap smear test. Most common reason offered for not undergoing Pap smear test were, they felt they were not at risk (41%), uncomfortable pelvic examination (25%) and fear of a bad result (16.6%). Conclusion: Knowledge of cancer cervix, screening and practice of Pap smear was low among Sikkimese nursing staff in India. There is an urgent need for re-orientation course for working nurses and integration of cervical cancer prevention issues in the nurses′ existing curriculum in India and other developing countries.
Publication History
Article published online:
12 July 2021
© 2015. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Objectives:
To assess baseline knowledge of cancer cervix, screening and practice of Pap smear screening among Sikkimese staff nurses in India.
Materials and Methods:
Between April 2012 and February 2013, a predesigned, pretested, self -administered multiple responses questionnaire survey was conducted among staff nurses’ working in various hospitals of Sikkim. Questionnaire contained information about their demographics, knowledge of cervical cancer, its risk factors, screening methods, attitudes toward cervical cancer screening and practice of Pap smear amongst themselves.
Results:
Overall, 90.4% nurses responded that they were aware of cancer cervix. Three quarter of the staff nurses were not aware of commonest site being cancer cervix in women. Of the 320 participants, who had heard of cancer cervix, 253 (79.1%) were aware of cancer cervix screening. Pap smear screening should start at 21 years or 3 years after sexual debut was known to only one-third of the nursing staff. Age was found to be a significant predictor of awareness of Pap smear screening among nursing staff. Awareness was significantly more prevalent among older staff (P < 0.007). Married nursing staffs were significantly more likely to be aware of screening methods, and nursing staff of Christian and Buddhist religion were 1.25 times and 2.03 times more likely to aware of screening methods than Hindu religion respectively. Only 16.6% nurses, who were aware of a Pap smear (11.9% of the total sample), had ever undergone a Pap smear test. Most common reason offered for not undergoing Pap smear test were, they felt they were not at risk (41%), uncomfortable pelvic examination (25%) and fear of a bad result (16.6%).
Conclusion:
Knowledge of cancer cervix, screening and practice of Pap smear was low among Sikkimese nursing staff in India. There is an urgent need for re-orientation course for working nurses and integration of cervical cancer prevention issues in the nurses’ existing curriculum in India and other developing countries.
INTRODUCTION
Worldwide, cervical cancer is the second most common (12%) cancer in women, however, in developing countries; it is the most common cancer among women.[1] With 528,000 new cases detected every year, cervical cancer is most notable among lower resource countries of sub-Saharan Africa. It is also the fourth most common cause of cancer death in women worldwide with 266,000 deaths in 2012. Almost 70% of the global burden falls in areas with lower levels of development.[2] India bears about one fifth of the world's burden of cervical cancer, and >100,000 new cases are detected every year in India, which causes 20% of all female deaths in India.[2,3] According to 3 year report (2009-2011) of population based cancer registries in India, cancer cervix continues to be leading site of cancer in India and Sikkim, and two-thirds of the cases are reported in advanced stage.[4]
The key to reducing cervical cancer morbidity and mortality is early detection and treatment of cervical precancerous lesions. Among all malignant tumors, cervical cancer is the one that can be most effectively controlled by organized screening programs.[5] An organized screening program can reduce incidence and mortality by 80% as shown in developed countries.[6] Despite being effective, most of the women in developing and under-developed countries do not have access to Pap smear screening. The major problem is low participation in the screening program.[7,8]
In India also, both early detection and screening remains a major area of concern coupled with poor literacy and low level of awareness amongst Indian women. Because of low doctor patient ratio in India, nursing staff are the major workforce in rural public health centers and Sub centers of India. The staff nurses are responsible, as primary gate keepers for giving information about cervical cancer and creating and conducting Pap smear screening tests among rural Indian women.[9]
To have a successful cancer control program, nursing staff must be aware of facts about cervical cancer and screening tests themselves. Furthermore, negative attitude toward and inaccurate knowledge of cervical cancer and screening methods among health care providers especially among nurses can pose substantial barriers to cervical control program in India and other developing countries. Moreover, if nurses themselves undergo screening tests regularly, they can be role models for other females in carrying out cervical cancer screening tests.
It is with this in mind, the aim of this study was to assess knowledge of cancer cervix, screening methods, attitude toward and practice of Pap smear screening among nursing staff working in Sikkim.
MATERIALS AND METHODS
Sikkim is a small state of Indian union located in the eastern Himalayas. The population of Sikkim is different in their culture, religion, customs and traditions from other states of India. The three different communities living in Sikkim-the Nepalis, Bhutias and Lepchas, constitute a homogeneous blend. There are two referral hospitals in Sikkim, Central Referral Hospital-teaching hospital of Sikkim Manipal Institute of Medical Sciences (SMIMS), and the Sir Thutob Namgyal Memorial Hospital at Gangtok, four district hospitals, 24 primary health centers and 147 sub centers in Sikkim. These hospitals provide comprehensive health care to the population of different communities of Sikkim.
It was a cross-sectional study conducted between April 2012 and February 2013. The study was approved by SMIMS institutional ethics committee. Initially major hospitals nursing staff (including trainee nursing staff, that is, nursing students, who were in their final year internship and yet to obtain their full registration) were invited in a group in a big hall and explained about the nature and purpose of the research. The staff nurses who agreed to participate were given a consent form along with a predesigned, pretested, self-administered multiple response questionnaires with both closed and open ended questions. The staff nurses, who could not come in groups and those who were working small hospitals; to them, an invitation letter along with consent form and questionnaire was sent in a sealed envelope to participate. Those who agreed to participate were requested to fill the questionnaire along with consent form and send back to the principal author.
The questionnaire items consisted of various basic facts about cervical cancer and screening, attitude of nursing staff toward screening, and about their practice habits. The questionnaire items were standard items that are very much important in practical aspects. Some items were modified, and some were adapted from review articles and added to the questionnaire by the principal investigator to suit the context of the study.
The data collected were thoroughly screened and entered into MS-excel (Microsoft, Redmond, WA, USA) spread sheets for analysis. The procedures involved were transcription, preliminary data inspection, and interpretation. The data were analyzed by computer software Instat Graph Pad version 3 (GraphPad Software, La Jolla, CA, USA). Descriptive statistics Chi-square tests were done, and the significance of tests was decided at P = 0.05. Data were analyzed using both univariate and multivariate analysis/binary logistic regression.
RESULTS
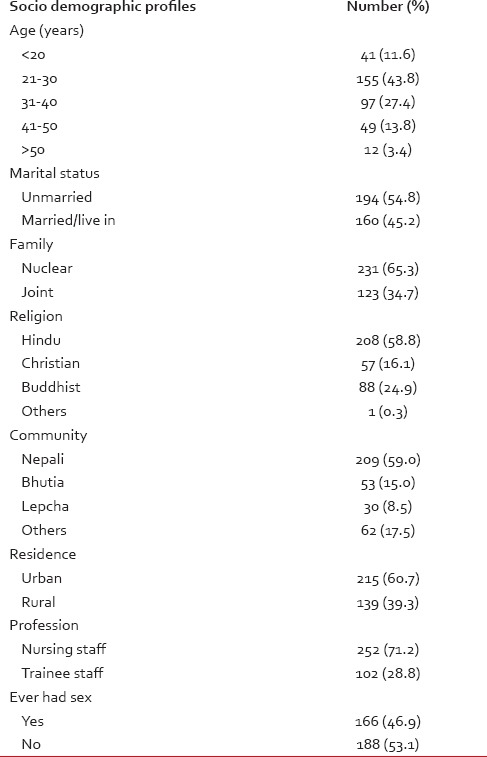
A total of 396 questionnaires were distributed during the study period of which 354 nursing staff returned the questionnaire in completed form with a response rate of 89.4%. Majority of the nursing staff were between 21 and 40 years of age, married, Hindu and belonged to Nepali community. Among the participants, 28.8% were trainee staff. Table 1 presents their socio-demographic characteristics.
Table 1
Socio demographic characteristics of 354 nursing staffs from the state of Sikkim, India who participated in the survey
To the question “are you aware of cancer cervix” 320 of 354 nursing staff (90.4%) responded that they knew about it. Those who were aware of cancer cervix proceeded with further questions about cancer cervix. Table 2 shows the detailed knowledge of the participants who had heard of cancer cervix. Three-quarter of the nursing staff were not aware that commonest site of cancer cervix is ectocervix. Although almost half of the participants were aware of cervical intraepithelial neoplasia (CIN), they had poor knowledge about association of CIN with cancer cervix. Most common risk factors identified by participants were multiple sex partners (52%), early age of coitus (35%) and multiple births (24%). Most common symptom responded by participants were offensive foul-smelling vaginal discharge (63%). Only half of the participants knew that the treatment of cancer cervix is radiotherapy or surgery.
Table 2
Detailed knowledge among 320 nursing staff who ever heard of cancer cervix
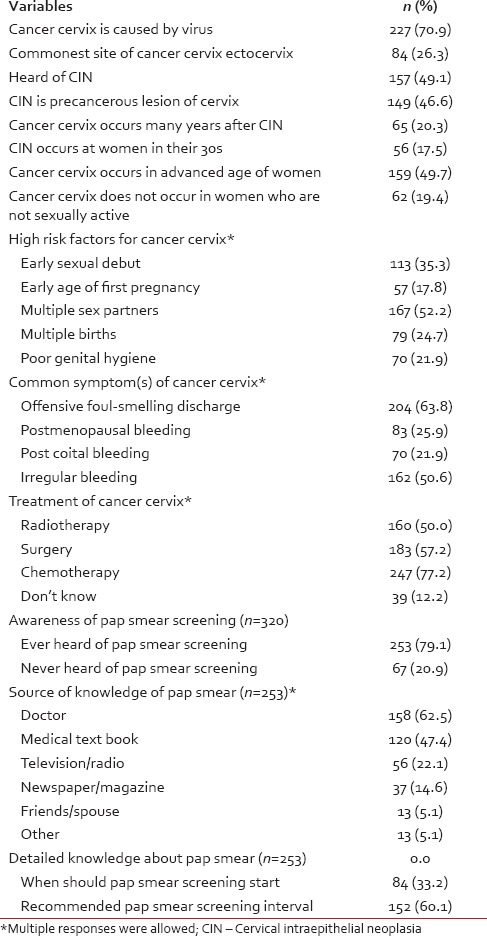
Of the 320 participants those who heard of cancer cervix, 253 (79.1%) were aware of cancer cervix screening or a Pap smear screening [Table 2]. Of these 62.5% (n = 158) responded that they had heard about it from doctors. Other source of knowledge were medical text book 47.4% (n = 120), television, radio or internet 22.1% (n = 56), print media 14.6% (n = 37) and friends, spouse and colleagues 5.1% (n = 13). Table 3 presents detailed knowledge of and attitudes toward Pap smear screening of the participant nursing staff. That Pap smear screening should start at 21 years or 3 years after sexual debut was known by one-third nursing staff, while recommended Pap smear interval of 3 years were known to 60% of the staff [Table 2]. Only 61% staff nurses were willing to attend Pap smear screening.
Table 3
Unadjusted associations between participant's socio demographic characteristics and awareness of pap smear screening and results of multivariate binary logistic regression analysis to determine factors independently associated with awareness of pap smear screening among the participants
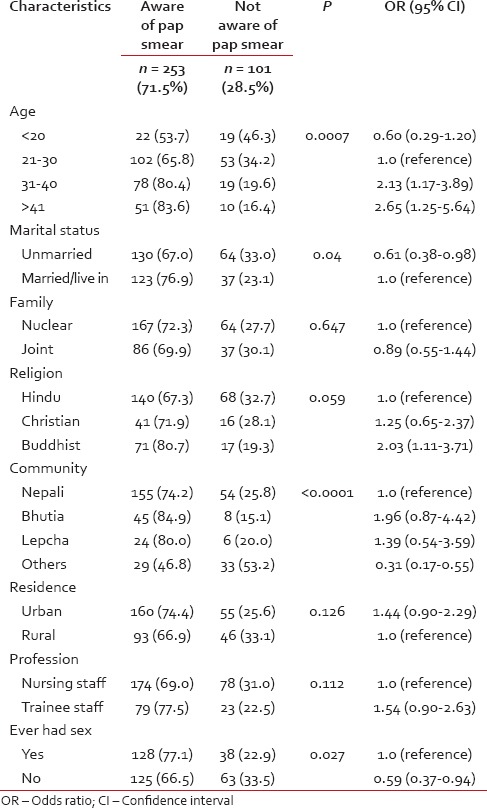
[Table 3] presents the unadjusted associations between participants’ socio-demographic characteristics and awareness of Pap smear and results of multivariate analysis of selected independent variables and their associations with awareness of Pap smear. Age was found to be a significant predictor of awareness of Pap smear screening among nursing staff. Awareness was significantly more prevalent among older staff (P < 0.007) and awareness increased with advancing age. Married nursing staff were significantly more likely to be aware of screening, and nursing staff of Christian and Buddhist religion were 1.25 times and 2.03 times more likely to be aware of screening methods than Hindu religion respectively. When the nursing staff was categorized by community, 85% Bhutia staff were aware of Pap smear that made them most aware of Pap smear screening. Bhutia staff was 1.96 times, and Lepcha staff was 1.39 times more likely to be aware of Pap smear. Sexually active staffs were significantly more aware of Pap smear screening [Table 3].
Only 16.6% (n = 42) of the 253 nursing staff who were aware of Pap smear had actually undergone a Pap test. Of these three-fourth (76%) staff underwent test only once, 21.4% twice, while only one (2.4%) staff underwent the test thrice. Thirty one percentage (n = 13) nursing staff were not satisfied with the test [Table 4].
Only 16.6% (n = 42) of the 253 nursing staff who were aware of Pap smear had actually undergone a Pap test. Of these three-fourth (76%) staff underwent test only once, 21.4% twice, while only one (2.4%) staff underwent the test thrice. Thirty one percentage (n = 13) nursing staff were not satisfied with the test [Table 4].
Table 4
Practice of pap smear among 253 nursing staffs who were aware of pap smear screening test
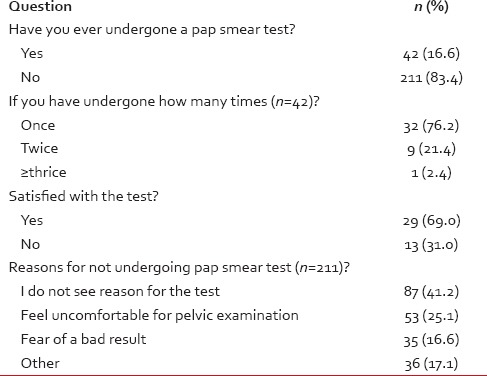
Among the participant staff nurses, who were aware of Pap smear test 83.4% (n = 211) had never undergone a test. The most common reason offered were-they felt that they were not at risk (41%). Twenty five percentage (n = 53) nurses offered uncomfortable pelvic examination as the reason for not undergoing the test, while 16.6% (n = 35) never underwent Pap smear for fear of a bad result [Table 4].
DISCUSSION
The findings of the present study show that knowledge of cancer cervix and Pap smear screening is low among the participant nursing staff. This study also shows that awareness about cancer cervix and Pap smear screening is lower among Sikkimese nursing staff than staff from high income countries,[10] but slightly higher than that had been reported from other Indian states.[11]
An important finding is the low level of awareness of cancer cervix and Pap smear screening among younger nursing staff. When 80


 PDF
PDF  Views
Views  Share
Share

