Multiple Myeloma Presenting as Thyroid Plasmacytoma
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2017; 38(04): 552-554
DOI: DOI: 10.4103/ijmpo.ijmpo_43_16
Abstract
Thyroid gland and thyroid cartilage infiltration in multiple myeloma (MM) are rare. Here, we discuss a patient who presented with hoarseness of voice and was found to have a hypodense lesion in right lobe of thyroid involving thyroid and cricoid cartilage. Fine-needle aspiration cytology with immunohistochemistry revealed extramedullary plasmacytoma of thyroid. MM was ruled out initially by serum protein electrophoresis, immunofixation, and bone marrow biopsy. Later, lytic lesions were found in multiple bones on radiation planning scan and he was finally diagnosed as case of MM with thyroid involvement. Treatment strategies of MM and thyroid plasmacytoma are also discussed briefly.
Publication History
Article published online:
04 July 2021
© 2017. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used forcommercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Thyroid gland and thyroid cartilage infiltration in multiple myeloma (MM) are rare. Here, we discuss a patient who presented with hoarseness of voice and was found to have a hypodense lesion in right lobe of thyroid involving thyroid and cricoid cartilage. Fine-needle aspiration cytology with immunohistochemistry revealed extramedullary plasmacytoma of thyroid. MM was ruled out initially by serum protein electrophoresis, immunofixation, and bone marrow biopsy. Later, lytic lesions were found in multiple bones on radiation planning scan and he was finally diagnosed as case of MM with thyroid involvement. Treatment strategies of MM and thyroid plasmacytoma are also discussed briefly.
Introduction
Plasma cell neoplasm is characterized by clonal proliferation of immunoglobulin producing terminally differentiated B-cells. The spectrum ranges from asymptomatic proliferation of tumor cells without end organ damage to multiple organ system involvement as seen in multiple myeloma (MM). These cells usually secrete antibodies which may be detected in urine or blood, thus forming a characteristic monoclonal band (M-band). Recently, three more components for diagnosis of MM are being considered, namely, clonal bone marrow plasma cells ≥60%, involved: uninvolved serum free-light chain ratio ≥100 and >1 focal lesion on magnetic resonance imaging, with each focal lesion ≥5 mm.[1]
These plasma cells may also form discrete/solitary mass of neoplastic plasma cells in bone known as solitary bone plasmacytoma (SBP) or in one of the various extramedullary sites known as extramedullary plasmacytoma (EMP).
Thyroid involvement in plasma cell malignancies is extremely rare.[2] Here, we report a case of MM, presenting initially as thyroid EMP.
Case Report
A 57-year-old diabetic male presented with complaint of hoarseness of voice for 2 months; there were no other symptoms. On examination, there was early stridor, with a mobile swelling on the right side of neck anteriorly, moving with deglutition. The patient was euthyroid clinically. Contrast-enhanced computed tomography (CECT) neck and chest showed a hypodense lesion in right lobe of thyroid going into right true vocal cord and false vocal cord, destroying thyroid, and cricoid cartilage. A clinical diagnosis of thyroid malignancy was made, but cartilage involvement was unusual. Fine-needle aspiration cytology (FNAC) from swelling showed predominantly plasma cell population and lymphoid cells pointing toward plasma cell neoplasm; however, a remote possibility of medullary carcinoma thyroid was also kept. Serum calcitonin was within normal limits. In view of FNAC report, the patient was evaluated for MM. Single urine protein electrophoresis reading (done on sample collected on spot) did not show any M-band. 24 h urine protein electrophoresis was not done. Serum protein electrophoresis showed M-band in gamma region (0.56 g/dl). Serum immunofixation showed lambda light chain restriction and 2 M-bands–IgG (0.56 g/dl) and IgA (no discernible light chain). Serum kappa and lambda free-light chain were 56.40 mg/L and 48.10 mg/L, respectively (Range: kappa - 3.3–19.4 mg/L and lambda - 5.71–26.30 mg/L). The kappa/lambda ratio was 1.17 (Range: 0.26–1.65). Blood counts and biochemistry were normal. Serum globulin was 3.8 g/dl (range 2–3.5 g/dl) and serum calcium was 9.3 mg/dl (range 8.5–10.2 mg/dl). Serum lactate dehydrogenase was 672 U/L (Range: 240–480 U/L).
Bone marrow examination showed normocellular marrow spaces with adequate representation of all three hematopoietic lineage elements. There were 10% plasma cells with no nodular aggregates.
18-Flourodeoxyglucose (FDG) positron emission tomography-CT scan showed an ill-defined nonavid to subtly FDG-avid enhancing soft tissue mass [Figure 1] arising from right lobe of thyroid gland ~3.3 cm × 4.4 cm × 6.7 cm with destruction of adjacent thyroid cartilage and narrowing of airway. Few subcentimetric nonavid to subtly FDG-avid bilateral level IB, II and right Level IV and VI lymph nodes were present.
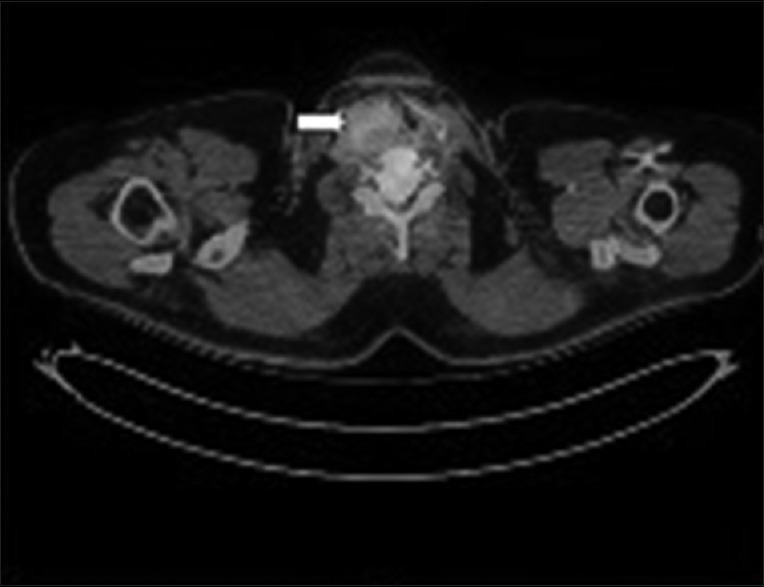
| Figure 1:Shows an fluorodeoxyglucose-avid enhancing mass arising from right lobe of thyroid (white arrow) causing thyroid cartilage destruction with narrowing of the airway
As blood investigations were inconclusive, a differential of plasmacytoma/MM with thyroid involvement versus medullary or anaplastic carcinoma of thyroid with monoclonal gammopathy of undetermined significance was kept and an open biopsy was advised. However, the patient refused for open biopsy.
Repeat FNAC was done from thyroid nodule with immunohistochemistry (IHC) performed on cell blocks prepared from the same. On microscopy, features were suggestive of infiltration by plasma cell neoplasm. On IHC, 60% of cells were bright CD38 positive and CD138 was dimly positive. CD45 was positive. Kappa marker was suggestive of cyto-kappa restriction. 40% of cells were positive for CD3. Cells were negative for CD20, CD23, CD10, and CD34. These findings suggested plasma cell neoplasm. Thus, a diagnosis of EMP of thyroid was made. As surgical treatment of this patient required thyroidectomy and laryngectomy due to thyroid cartilage involvement, he was planned for external beam radiotherapy (EBRT), to preserve voice without compromising outcome.
CECT was done for EBRT planning. To our surprise, it showed lytic lesions in skull and ribs.
Thus, patient's diagnosis got changed from EMP to MM with thyroid involvement. He was subsequently planned for chemotherapy, and EBRT was withheld.
Discussion
EMP represents approximately 3% of all plasma cell neoplasms. EMP occurs in head and neck area in 80%–90%-cases.[3]
In cases with inapparent end organ damage, it becomes difficult to distinguish SBP/EMP from MM. This differentiation is crucial because of difference in management of these two entities. While the treatment of choice for plasmacytoma is surgery or EBRT, chemotherapy with or without autologous stem cell transplant remains the mainstay of treatment for MM.[4]
Localization of hematologic malignancies to thyroid is rare. Rubin et al.[5] reviewed 40 cases of EMP involving thyroid gland and found that EMP in thyroid gland had regional lymph node involvement in 43% of tumors, 50% of patients were hypothyroid at diagnosis, and 63% had chronic lymphocytic thyroiditis (Hashimoto's Thyroiditis).
The gold standard diagnostic test for diagnosis of EMP is tissue biopsy. There are few reports regarding diagnosing them with FNAC. Bourtsos et al.[6] reported thyroid plasmacytoma that was initially misinterpreted as medullary carcinoma due to the presence of amyloid substance in the aspirate. The authors[6] suggested that EMP should be considered in the differential of any neck mass that yields cells associated with amyloid/amyloid-like material. In our patient, normal calcitonin, FNAC, and IHC ruled out other neoplasms of thyroid.
After a diagnosis is made, course of treatment is decided in a multimodality setting. In a case report by Mitchell et al.,[7] approach to treatment was systemic therapy for MM and local treatment for EMP of thyroid.
Hence, for control of local disease, surgical excision or EBRT is required. EBRT is preferred when organ function loss (e.g., dysphonia/swallowing/aspiration problems) is contemplated postsurgery.[8] In the review by Rubin et al.,[5] treatment modalities included surgery alone in 40%, surgery and radiotherapy in 44%, and radiotherapy alone in 14% of cases. There was no difference in outcome between different groups.
Another interesting finding in our patient was thyroid cartilage infiltration, which is rare in MM.[9] The two mechanisms suggested for cartilaginous involvement in MM are direct extension from adjacent plasmacytoma or metaplasia of cartilage to bone with the formation of marrow cavity, in which plasma cell proliferation takes place.[10] In our patient, cartilage involvement was likely due to direct extension from thyroid.
As discussed, our patient was finally diagnosed with MM with thyroid cartilage destruction. This patient was subsequently started on chemotherapy based on bortezomib, cyclophosphamide, and dexamethasone.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Rajkumar SV, Dimopoulos MA, Palumbo A, Blade J, Merlini G, Mateos MV, et al. International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol 2014;15:e538-48.
- Chaganti S, Gurunathan R, McNaboe E. Solitary extramedullary plasmacytoma of the thyroid gland: A case report and review of literature. Internet J Head Neck Surg 2006;2. [DOI: 10.5580/15ad].
- Galieni P, Cavo M, Pulsoni A, Avvisati G, Bigazzi C, Neri S, et al. Clinical outcome of extramedullary plasmacytoma. Haematologica 2000;85:47-51.
- Soutar R, Lucraft H, Jackson G, Reece A, Bird J, Low E, et al. Guidelines on the diagnosis and management of solitary plasmacytoma of bone and solitary extramedullary plasmacytoma. Br J Haematol 2004;124:717-26.
- Rubin J, Johnson JT, Killeen R, Barnes L. Extramedullary plasmacytoma of the thyroid associated with a serum monoclonal gammopathy. Arch Otolaryngol Head Neck Surg 1990;116:855-9.
- Bourtsos EP, Bedrossian CW, De Frias DV, Nayar R. Thyroid plasmacytoma mimicking medullary carcinoma: A potential pitfall in aspiration cytology. Diagn Cytopathol 2000;23:354-8.
- Mitchell HK, Garas G, Mazarakis N, McGlashan J. Extramedullary relapse of multiple myeloma in the thyroid cartilage. BMJ Case Rep 2013;2013. pii: bcr2013200689.
- Sasaki R, Yasuda K, Abe E, Uchida N, Kawashima M, Uno T, et al. Multi-institutional analysis of solitary extramedullary plasmacytoma of the head and neck treated with curative radiotherapy. Int J Radiat Oncol Biol Phys 2012;82:626-34.
- Van Dyke CW, Masaryk TJ, Lavertu P. Multiple myeloma involving the thyroid cartilage. AJNR Am J Neuroradiol 1996;17:570-2.
- Sosna J, Slasky BS, Paltiel O, Pizov G, Libson E. Multiple myeloma involving the thyroid cartilage: Case report. AJNR Am J Neuroradiol 2002;23:316-8.
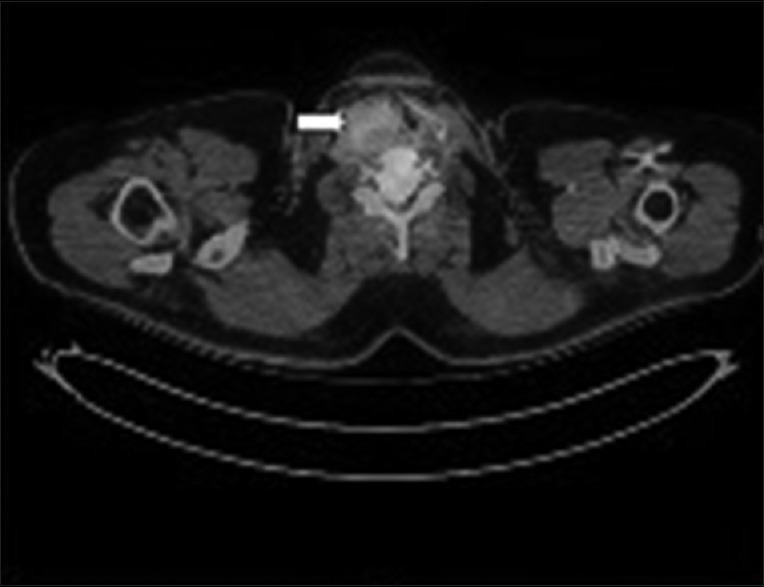
| Figure 1:Shows an fluorodeoxyglucose-avid enhancing mass arising from right lobe of thyroid (white arrow) causing thyroid cartilage destruction with narrowing of the airway
References
- Rajkumar SV, Dimopoulos MA, Palumbo A, Blade J, Merlini G, Mateos MV, et al. International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol 2014;15:e538-48.
- Chaganti S, Gurunathan R, McNaboe E. Solitary extramedullary plasmacytoma of the thyroid gland: A case report and review of literature. Internet J Head Neck Surg 2006;2. [DOI: 10.5580/15ad].
- Galieni P, Cavo M, Pulsoni A, Avvisati G, Bigazzi C, Neri S, et al. Clinical outcome of extramedullary plasmacytoma. Haematologica 2000;85:47-51.
- Soutar R, Lucraft H, Jackson G, Reece A, Bird J, Low E, et al. Guidelines on the diagnosis and management of solitary plasmacytoma of bone and solitary extramedullary plasmacytoma. Br J Haematol 2004;124:717-26.
- Rubin J, Johnson JT, Killeen R, Barnes L. Extramedullary plasmacytoma of the thyroid associated with a serum monoclonal gammopathy. Arch Otolaryngol Head Neck Surg 1990;116:855-9.
- Bourtsos EP, Bedrossian CW, De Frias DV, Nayar R. Thyroid plasmacytoma mimicking medullary carcinoma: A potential pitfall in aspiration cytology. Diagn Cytopathol 2000;23:354-8.
- Mitchell HK, Garas G, Mazarakis N, McGlashan J. Extramedullary relapse of multiple myeloma in the thyroid cartilage. BMJ Case Rep 2013;2013. pii: bcr2013200689.
- Sasaki R, Yasuda K, Abe E, Uchida N, Kawashima M, Uno T, et al. Multi-institutional analysis of solitary extramedullary plasmacytoma of the head and neck treated with curative radiotherapy. Int J Radiat Oncol Biol Phys 2012;82:626-34.
- Van Dyke CW, Masaryk TJ, Lavertu P. Multiple myeloma involving the thyroid cartilage. AJNR Am J Neuroradiol 1996;17:570-2.
- Sosna J, Slasky BS, Paltiel O, Pizov G, Libson E. Multiple myeloma involving the thyroid cartilage: Case report. AJNR Am J Neuroradiol 2002;23:316-8.


 PDF
PDF  Views
Views  Share
Share

