Pathognomonic Features in Lipoma of the Tongue
CC BY 4.0 · Indian J Med Paediatr Oncol 2025; 46(05): 503-504
DOI: DOI: 10.1055/s-0045-1809966
Case Summary
A 55-year-old female patient presented with swelling in the right side of her tongue gradually increasing in size over the past 15 days. Otherwise, she was asymptomatic.
The patient was a habitual betel nut chewer.
On local examination, a 2 × 2 cm globular swelling was noted in the right lateral border of the tongue. No other lesions were noted. No palpable cervical lymphadenopathy.
A contrast-enhanced computed tomography (CT) scan of the neck showed an 11 (anteroposterior) × 16 (transverse) × 12 (craniocaudal) mm, well-defined fat density lesion in the anterior third of the tongue (along the right lateral border) with no obvious enhancement. The rest of her tongue was normal. No notable cervical lymphadenopathy was observed. The lesion was excised from the patient under local anesthesia. The patient is currently on follow-up and doing well.

| Fig 1 : Preoperative image showing a mass and intraoperative image showing an ovoid encapsulated yellow soft tissue mass with smooth external surface in the right lateral border of tongue.
It is difficult to make a clinical diagnosis of oral lipoma because of the possibility of diagnosis of various benign tumors including mucocele, encapsulated abscess, lipoma, neuroma, rhabdomyoma, neurofibroma, fibroma, or salivary gland tumor.
Macroscopically, the lesion measured 2 ×1.5 × 1 cm. The lesion was an encapsulated yellow soft tissue, ovoid, and with a smooth external surface ([Fig. 1]).
Microscopically, a thin fibrous capsule is seen. The tumor shows lobular architecture separated by variably thick fibrovascular septa.[1] These tumor cells are mature adipocytes with small eccentrically placed nuclei where the nuclei are often compressed ([Fig. 2]) with no notable inflammation, or cellular atypia, lipoblasts, or features of malignancy. Thus, final diagnosis was histopathologically confirmed as lipoma.
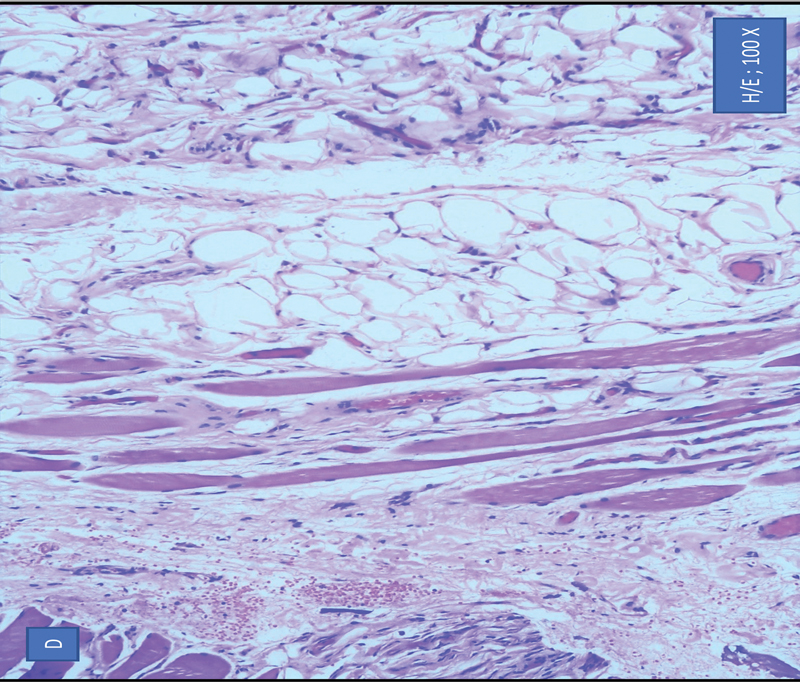
| Figure 2: Microscopically the sections showing sheets and lobules of benign adipocytes separated by variably thick fibrovascular septa. Focally, the adipocytes are seen to infiltrate around skeletal muscle tissue.
Author's Contributions
M.N. conceptualised the study, reviewed the manuscript and he is the guarantor. R.B. designed the study, defined intellectual content, performed literature review, prepared and edited the manuscript. R.M and V.C.K. reviewed the manuscript.
Publication History
Article published online:
07 July 2025
© 2025. The Author(s). This is an open access article published by Thieme under the terms of the Creative Commons Attribution License, permitting unrestricted use, distribution, and reproduction so long as the original work is properly cited. (https://creativecommons.org/licenses/by/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
- Isolated Plexiform Neurofibroma of the TongueAbhishek Sharma, J Lab Physicians, 2013
- Diagnosis and Management of an Isolated Pediatric Plexiform Neurofibroma Involving the Hepatic and Celiac Plexus Using Multimodality Approach: Problem Solving w...Merel M. Scheurkogel, European Journal of Pediatric Surgery Reports
- Benign Synovial Tumors and Proliferative ProcessesHillary W. Garner, Seminars in Musculoskeletal Radiology
- Benign Synovial Tumors and Proliferative ProcessesHillary W. Garner, Seminars in Musculoskeletal Radiology
- CNS Lipoma in Patients with Epidermal Nevus SyndromeV. Mall, Neuropediatrics, 2000
- Macroglossia – Not Always AL Amyloidosis<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- HDAC3 Is Required for Pathognomonic Features of Langerhans Cell Histiocytes<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- Donor B-Cell Alloantibody Deposition and Germinal Center Formation Are Required for the Development of Murine Chronic Gvhd and Bronchiolitis Obliterans<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- Morphological changes in a case of SARS-CoV-2 infection<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- Atypical CML: diagnosis and treatment<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
Case Summary
A 55-year-old female patient presented with swelling in the right side of her tongue gradually increasing in size over the past 15 days. Otherwise, she was asymptomatic.
The patient was a habitual betel nut chewer.
On local examination, a 2 × 2 cm globular swelling was noted in the right lateral border of the tongue. No other lesions were noted. No palpable cervical lymphadenopathy.
A contrast-enhanced computed tomography (CT) scan of the neck showed an 11 (anteroposterior) × 16 (transverse) × 12 (craniocaudal) mm, well-defined fat density lesion in the anterior third of the tongue (along the right lateral border) with no obvious enhancement. The rest of her tongue was normal. No notable cervical lymphadenopathy was observed. The lesion was excised from the patient under local anesthesia. The patient is currently on follow-up and doing well.

| Fig 1 : Preoperative image showing a mass and intraoperative image showing an ovoid encapsulated yellow soft tissue mass with smooth external surface in the right lateral border of tongue.
It is difficult to make a clinical diagnosis of oral lipoma because of the possibility of diagnosis of various benign tumors including mucocele, encapsulated abscess, lipoma, neuroma, rhabdomyoma, neurofibroma, fibroma, or salivary gland tumor.
Macroscopically, the lesion measured 2 ×1.5 × 1 cm. The lesion was an encapsulated yellow soft tissue, ovoid, and with a smooth external surface ([Fig. 1]).
Microscopically, a thin fibrous capsule is seen. The tumor shows lobular architecture separated by variably thick fibrovascular septa.[1] These tumor cells are mature adipocytes with small eccentrically placed nuclei where the nuclei are often compressed ([Fig. 2]) with no notable inflammation, or cellular atypia, lipoblasts, or features of malignancy. Thus, final diagnosis was histopathologically confirmed as lipoma.
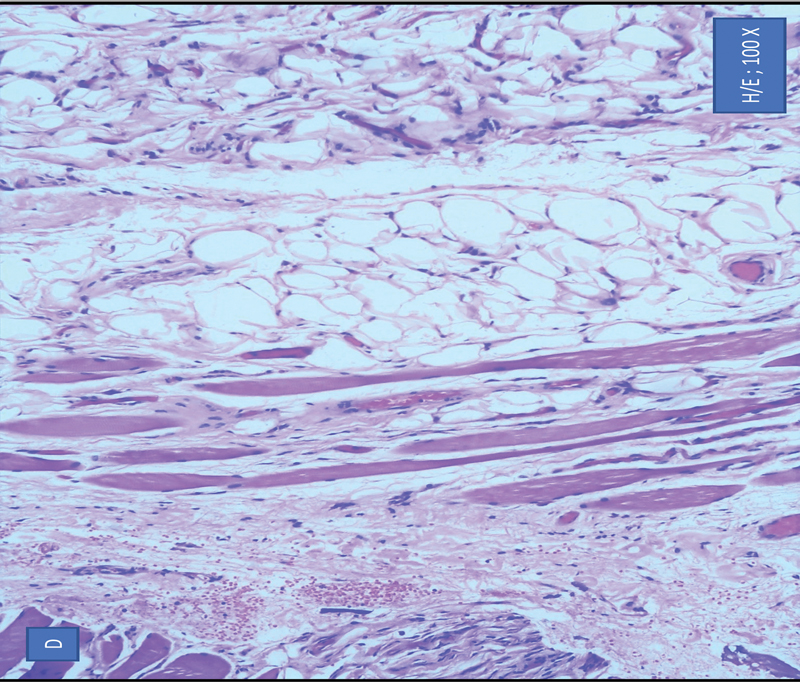
| Figure 2: Microscopically the sections showing sheets and lobules of benign adipocytes separated by variably thick fibrovascular septa. Focally, the adipocytes are seen to infiltrate around skeletal muscle tissue.
Discussion
The common mesenchymal tumors of the soft tissue are benign lipomas. The vestibule, floor of the mouth, tongue, lip, palate, buccal mucosa, and major salivary glands are additional potential locations for occurrence.[2] [3] It is estimated that between 1 and 4.4%-of all benign oral lesions develop in the oral cavity, with tongue lipomas most frequently occurring in the superficial submucosal connective tissue. Thus, showing the relatively rare occurrence of tongue lipomas.[4]
Lipomas are more frequently seen in adults in the age group of 40 years; they can occur in all age groups with an equal gender predilection.[4]
Although the etiology of lipomas is still unknown, various potential etiologies are heredity, hormones, trauma, infection, chronic irritation, infarction, and fat degeneration.[5]
Lipomas usually are asymptomatic and slow growing.
Lipoma or classical lipoma has histopathologically benign variations including angiolipoma, angiomyolipoma, myolipoma, fibrolipoma, chondroid lipoma, chondrolipoma, osteolipoma, intramuscular lipoma, myelolipoma, sialolipoma, spindle cell/pleomorphic lipoma, hamartomatous lesions, diffuse lipomatous proliferations, and hibernoma.[6]
Imaging modalities such as ultrasound, CT scan, or magnetic resonance imaging (MRI) may be performed to aid the diagnosis of lipoma.
The low mass density of lipomas can be indicated in a CT scan alongside differentiated infiltrating lipoma and well-encapsulated lipomas. For a greater soft tissue definition, MRI is preferred. An MRI shows vastly improved definition of lingual tumor boundaries in pre-operative settings. The vicinities of these tumors to large vessels, tumor vascularity, etc., are better visualized in MRI.[7] However, the gold standard for diagnosis continues to be histopathological examination. The tumor appears in histopathological examination as adult fat cells subdivided into lobules by fibrous connective tissue septa.[8] Capillaries being compressed by the surrounding adipocytes is depictive of tumor vasculature. Lipomas are considered to have excellent prognosis and recurrence is not common after complete excision. Hence complete surgical resection is considered to be the cornerstone of treatment. Due to its benign nature and very low recurrence rate, the lesion does not need any additional adjuvant therapy after complete resection.
Conflict of Interest
None declared.
Author's Contributions
M.N. conceptualised the study, reviewed the manuscript and he is the guarantor. R.B. designed the study, defined intellectual content, performed literature review, prepared and edited the manuscript. R.M and V.C.K. reviewed the manuscript.
References
-
Chandak S, Pandilwar PK, Chandak T, Mundhada R. Huge lipoma of tongue. Contemp Clin Dent 2012; 3 (04) 507-509
- Roux M. On exostoses: their character. Am J Dent Sci 1848; 9 (01) 133-134
- Raj AA, Shetty PM, Yadav SK. Lipoma of the floor of the mouth: report of an unusually large lesion. J Maxillofac Oral Surg 2014; 13 (03) 328-331
- Fregnani ER, Pires FR, Falzoni R, Lopes MA, Vargas PA. Lipomas of the oral cavity: clinical findings, histological classification and proliferative activity of 46 cases. Int J Oral Maxillofac Surg 2003; 32 (01) 49-53
- Srinivasan K, Hariharan N, Parthiban P, Shyamala R. Lipoma of tongue - a rare site for a rare site for a common tumour. Indian J Otolaryngol Head Neck Surg 2007; 59 (01) 83-84
- Juliasse LE, Nonaka CF, Pinto LP, Freitas RdeA, Miguel MC. Lipomas of the oral cavity: clinical and histopathologic study of 41 cases in a Brazilian population. Eur Arch Otorhinolaryngol 2010; 267 (03) 459-465
- Brightman VJ. Diseases of the tongue. In: Lynch MA, Brightman VJ, Greenberg MS. eds Burket's Oral Medicine. 9th ed.. Philadelphia, PA: JB Lippincott Co.; 1994: 240-298
- Egido-Moreno S, Lozano-Porras AB, Mishra S, Allegue-Allegue M, Marí-Roig A, López-López J. Intraoral lipomas: review of literature and report of two clinical cases. J Clin Exp Dent 2016; 8 (05) e597-e603
Address for correspondence
Publication History
Article published online:
07 July 2025
© 2025. The Author(s). This is an open access article published by Thieme under the terms of the Creative Commons Attribution License, permitting unrestricted use, distribution, and reproduction so long as the original work is properly cited. (https://creativecommons.org/licenses/by/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
- Isolated Plexiform Neurofibroma of the TongueAbhishek Sharma, J Lab Physicians, 2013
- Diagnosis and Management of an Isolated Pediatric Plexiform Neurofibroma Involving the Hepatic and Celiac Plexus Using Multimodality Approach: Problem Solving w...Merel M. Scheurkogel, European Journal of Pediatric Surgery Reports
- Benign Synovial Tumors and Proliferative ProcessesHillary W. Garner, Seminars in Musculoskeletal Radiology
- CNS Lipoma in Patients with Epidermal Nevus SyndromeV. Mall, Neuropediatrics, 2000
- Benign Synovial Tumors and Proliferative ProcessesHillary W. Garner, Seminars in Musculoskeletal Radiology
- Noninvasive Diagnostic Technique for Nonalcoholic Fatty Liver Disease Based on Features of Tongue Images<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- Classifying Chinese Medicine Constitution Using Multimodal Deep-Learning Model<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- Treatment outcomes of real-time intraoral sonography-guided implantation technique of 198Au grain brachytherapy for T1 and T2 tongue cancer<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- A newly developed patient fixation system using a dedicated mouthpiece and dental impression materials for head and neck radiotherapy: a preliminary study<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">
- Ferroelectricity in biological building blocks: Slipping on a banana peel?<svg viewBox="0 0 24 24" fill="none" xmlns="http://www.w3.org/2000/svg">

| Fig 1 : Preoperative image showing a mass and intraoperative image showing an ovoid encapsulated yellow soft tissue mass with smooth external surface in the right lateral border of tongue.
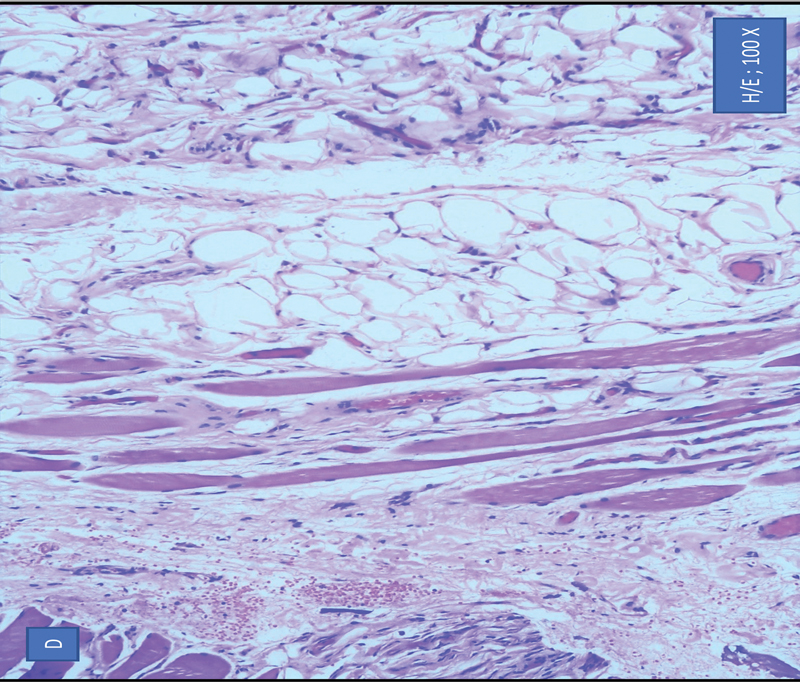
| Figure 2: Microscopically the sections showing sheets and lobules of benign adipocytes separated by variably thick fibrovascular septa. Focally, the adipocytes are seen to infiltrate around skeletal muscle tissue.
References
-
Chandak S, Pandilwar PK, Chandak T, Mundhada R. Huge lipoma of tongue. Contemp Clin Dent 2012; 3 (04) 507-509
- Roux M. On exostoses: their character. Am J Dent Sci 1848; 9 (01) 133-134
- Raj AA, Shetty PM, Yadav SK. Lipoma of the floor of the mouth: report of an unusually large lesion. J Maxillofac Oral Surg 2014; 13 (03) 328-331
- Fregnani ER, Pires FR, Falzoni R, Lopes MA, Vargas PA. Lipomas of the oral cavity: clinical findings, histological classification and proliferative activity of 46 cases. Int J Oral Maxillofac Surg 2003; 32 (01) 49-53
- Srinivasan K, Hariharan N, Parthiban P, Shyamala R. Lipoma of tongue - a rare site for a rare site for a common tumour. Indian J Otolaryngol Head Neck Surg 2007; 59 (01) 83-84
- Juliasse LE, Nonaka CF, Pinto LP, Freitas RdeA, Miguel MC. Lipomas of the oral cavity: clinical and histopathologic study of 41 cases in a Brazilian population. Eur Arch Otorhinolaryngol 2010; 267 (03) 459-465
- Brightman VJ. Diseases of the tongue. In: Lynch MA, Brightman VJ, Greenberg MS. eds Burket's Oral Medicine. 9th ed.. Philadelphia, PA: JB Lippincott Co.; 1994: 240-298
- Egido-Moreno S, Lozano-Porras AB, Mishra S, Allegue-Allegue M, Marí-Roig A, López-López J. Intraoral lipomas: review of literature and report of two clinical cases. J Clin Exp Dent 2016; 8 (05) e597-e603


 PDF
PDF  Views
Views  Share
Share

