Pattern of Non-Hodgkin Lymphoma in a Tertiary Care Center in Northeast India Using Morphology and Immunohistochemistry
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2019; 40(04): 595-597
DOI: DOI: 10.4103/ijmpo.ijmpo_129_18
Sir,
Lymphoma is a neoplasm with clonal expansion of lymphoid cells that share the histologic pattern and immunohistochemistry (IHC) of their normal counterpart. They can arise in lymph nodes or in extranodal sites. There is a marked geographic variation in lymphoma. It is higher in the developed Western world and lower in Asia and Africa, except endemic Burkitt lymphoma and some T-cell lymphomas.[1] A limited number of studies on non-Hodgkin lymphoma (NHL) have been carried out in Northeast India. The current study was carried out to diagnose cases of NHL using both morphology and IHC. A prospective study over a 18-month duration was carried out from July 2016 to December 2017 to study the pattern and prevalence of lymphoma cases presenting to our tertiary care center.
Sections from the paraffin-embedded tissues were stained using hematoxylin and eosin stain. Morphology of the cells was studied, and the necessary immunohistochemical markers were advised. The basic panel for lymphoma at our institute is CD45, CD20, and CD3, along with CD30, CD15, ALK, EMA, MUM1, BCl2, BCl6, CD10, CD5, CD23, Cyclin D1, TdT, and Ki67. Diagnosis was made after morphological and immunohistochemical correlation. Biochemical and radiological findings were recorded.
A total of 151 cases were studied, and NHL comprised 86% (130 cases) of the total cases. Of the total NHL cases, 76% (95 cases) were B-cell NHL and 24% (30 cases) were T-cell NHL [Table 1]. In a study by Boffetta et al., a higher proportion of B-cell NHL such as diffuse large B-cell lymphoma (DLBCL) and follicular lymphoma is seen in America compared to the increased prevalence of T-cell NHL in Asian countries.[2] Asians have a higher incidence of T-cell lymphoma compared to the Western population, probably due to a lesser number of certain B-cell lymphomas.[3] In India, a study by Naresh et al. found B-cell lymphoma to comprise 79.1% of the NHLs, whereas T-cell lymphomas formed 16.2% of the total.[4]
Table 1 Age and sex distribution of NHL
Among 130 NHL cases, 94 (72%) were male and 36 (28%) were female in our study.
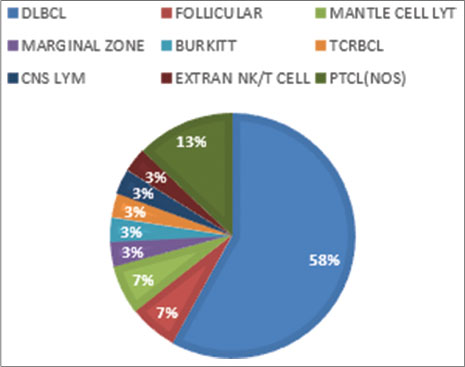
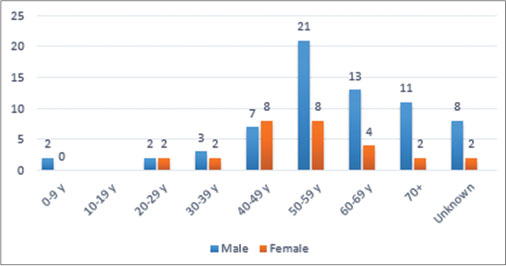
NHLs have a varied age distribution. It is a disease most common in the middle-aged and elderly. Lymphoblastic lymphoma is common in children and adolescents (three cases). In our study, we observed that DLBCL had a varied age range from 5 years to 93 years, while PTCL was common in the middle-aged population. Burkitt lymphoma is common in children. The median age for NHL was 53.5 years. The median age for T-cell NHL was found to be 44 years, and that for B-cell NHL, it was 55 years [Figure 1] and [Figure 2].
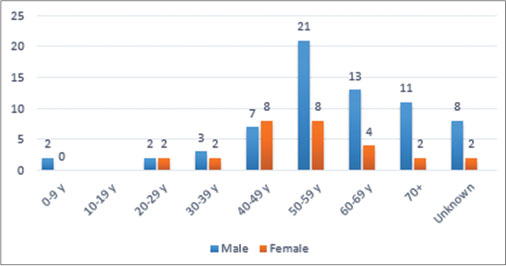
| Fig. 1 Age distribution of B-cell non-Hodgkin lymphoma
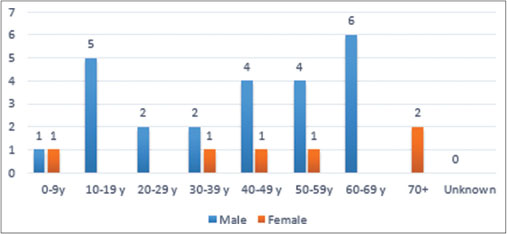
| Fig. 2 Age distribution of T-cell non-Hodgkin lymphoma
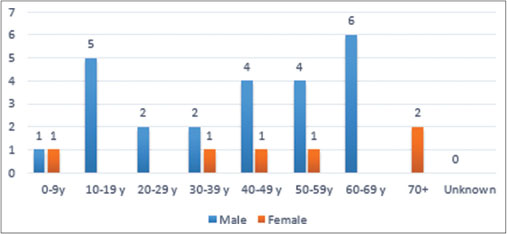
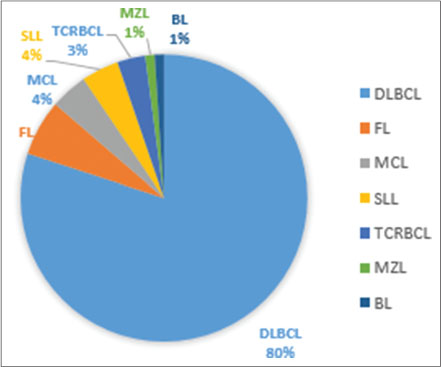
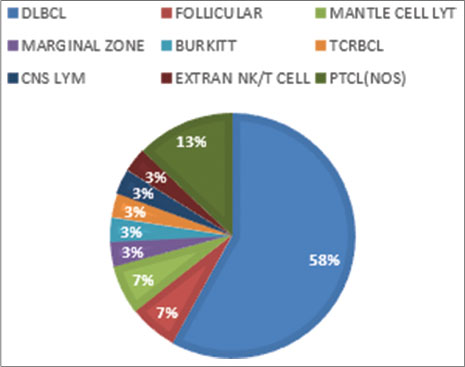
Among NHLs, according to the International non–Hodgkin’s Lymphoma Study Group Series, the most common was DLBCL with 31% cases, followed by 22% of follicular lymphoma. All types of T-cell processes, including natural killer cell disorders, made up only 12% of the cases.[5] According to Naresh et al., DLBCL was the most common subtype (34% of all NHLs) followed by follicular lymphoma.[4] In our study, five cases of NHL could not be subclassified as they were lost to follow-up. B-cell type accounted for 95 cases, whereas 30 cases were of T-cell subtype. DLBCL was the most common subtype of B-cell NHL, comprising 76 cases (80%), followed by follicular lymphoma which comprised of 6 cases (7%). Among T-cell NHLs, peripheral T-cell Lymphoma (PTCL [NOS]) was the most common with 19 cases (63%) followed by anaplastic large cell lymphoma (17%) and T-lymphoblastic lymphoma (17%) [Figure 3] and [Figure 4].
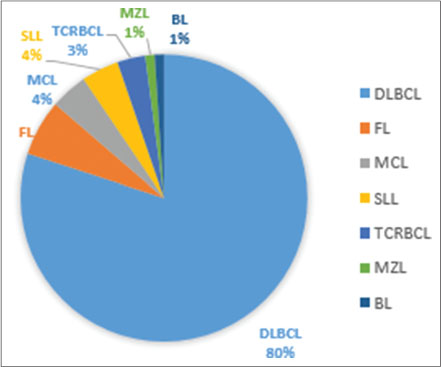
| Fig. 3 Subtypes of B-cell non-Hodgkin lymphoma
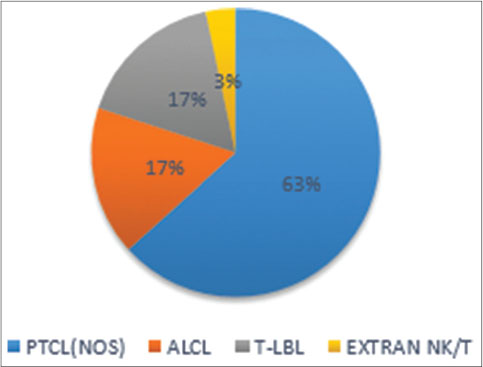
| Fig. 4 Subtypes of T-cell non-Hodgkin lymphoma
Nodal presentation is common; however, 31 cases (20.5%) were found to have a primarily extranodal presentation [Table 2] and [Figure 5]. Eighteen cases were of extranodal DLBCL subtype, two cases were mantle cell lymphoma, two were follicular lymphoma, and one was T-cell-rich B-cell lymphoma. One case of marginal zone lymphoma was from the parotid gland. One case of Burkitt Lymphoma was also detected in the gingivobuccal sulcus. Five cases were extranodal T-cell NHL, PTCL (NOS) subtype. The gastrointestinal tract was found to be the most common site of extranodal disease (11 cases) followed by testis and tonsils (four each).
| Fig. 5 Extranodal lymphoma
Cyclophosphamide, doxorubicin, vincristine, and prednisone regimen with or without rituximab is used in the management of NHLs in our setup.
Publication History
Received: 07 June 2018
Accepted: 12 July 2019
Article published online:
03 June 2021© 2020. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/).
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Sir,
Lymphoma is a neoplasm with clonal expansion of lymphoid cells that share the histologic pattern and immunohistochemistry (IHC) of their normal counterpart. They can arise in lymph nodes or in extranodal sites. There is a marked geographic variation in lymphoma. It is higher in the developed Western world and lower in Asia and Africa, except endemic Burkitt lymphoma and some T-cell lymphomas.[1] A limited number of studies on non-Hodgkin lymphoma (NHL) have been carried out in Northeast India. The current study was carried out to diagnose cases of NHL using both morphology and IHC. A prospective study over a 18-month duration was carried out from July 2016 to December 2017 to study the pattern and prevalence of lymphoma cases presenting to our tertiary care center.
Sections from the paraffin-embedded tissues were stained using hematoxylin and eosin stain. Morphology of the cells was studied, and the necessary immunohistochemical markers were advised. The basic panel for lymphoma at our institute is CD45, CD20, and CD3, along with CD30, CD15, ALK, EMA, MUM1, BCl2, BCl6, CD10, CD5, CD23, Cyclin D1, TdT, and Ki67. Diagnosis was made after morphological and immunohistochemical correlation. Biochemical and radiological findings were recorded.
A total of 151 cases were studied, and NHL comprised 86% (130 cases) of the total cases. Of the total NHL cases, 76% (95 cases) were B-cell NHL and 24% (30 cases) were T-cell NHL [Table 1]. In a study by Boffetta et al., a higher proportion of B-cell NHL such as diffuse large B-cell lymphoma (DLBCL) and follicular lymphoma is seen in America compared to the increased prevalence of T-cell NHL in Asian countries.[2] Asians have a higher incidence of T-cell lymphoma compared to the Western population, probably due to a lesser number of certain B-cell lymphomas.[3] In India, a study by Naresh et al. found B-cell lymphoma to comprise 79.1% of the NHLs, whereas T-cell lymphomas formed 16.2% of the total.[4]
Table 1 Age and sex distribution of NHL
Among 130 NHL cases, 94 (72%) were male and 36 (28%) were female in our study.
NHLs have a varied age distribution. It is a disease most common in the middle-aged and elderly. Lymphoblastic lymphoma is common in children and adolescents (three cases). In our study, we observed that DLBCL had a varied age range from 5 years to 93 years, while PTCL was common in the middle-aged population. Burkitt lymphoma is common in children. The median age for NHL was 53.5 years. The median age for T-cell NHL was found to be 44 years, and that for B-cell NHL, it was 55 years [Figure 1] and [Figure 2].
| Fig. 1 Age distribution of B-cell non-Hodgkin lymphoma
| Fig. 2 Age distribution of T-cell non-Hodgkin lymphoma
Among NHLs, according to the International non–Hodgkin’s Lymphoma Study Group Series, the most common was DLBCL with 31% cases, followed by 22% of follicular lymphoma. All types of T-cell processes, including natural killer cell disorders, made up only 12% of the cases.[5] According to Naresh et al., DLBCL was the most common subtype (34% of all NHLs) followed by follicular lymphoma.[4] In our study, five cases of NHL could not be subclassified as they were lost to follow-up. B-cell type accounted for 95 cases, whereas 30 cases were of T-cell subtype. DLBCL was the most common subtype of B-cell NHL, comprising 76 cases (80%), followed by follicular lymphoma which comprised of 6 cases (7%). Among T-cell NHLs, peripheral T-cell Lymphoma (PTCL [NOS]) was the most common with 19 cases (63%) followed by anaplastic large cell lymphoma (17%) and T-lymphoblastic lymphoma (17%) [Figure 3] and [Figure 4].
| Fig. 3 Subtypes of B-cell non-Hodgkin lymphoma
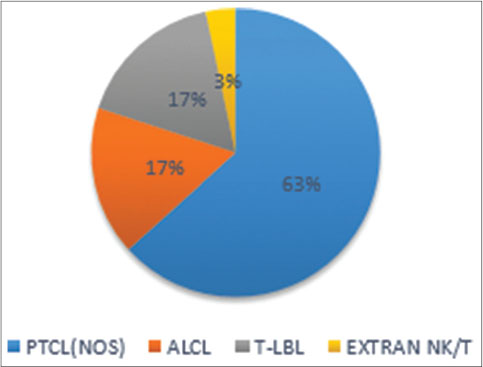
| Fig. 4 Subtypes of T-cell non-Hodgkin lymphoma
Nodal presentation is common; however, 31 cases (20.5%) were found to have a primarily extranodal presentation [Table 2] and [Figure 5]. Eighteen cases were of extranodal DLBCL subtype, two cases were mantle cell lymphoma, two were follicular lymphoma, and one was T-cell-rich B-cell lymphoma. One case of marginal zone lymphoma was from the parotid gland. One case of Burkitt Lymphoma was also detected in the gingivobuccal sulcus. Five cases were extranodal T-cell NHL, PTCL (NOS) subtype. The gastrointestinal tract was found to be the most common site of extranodal disease (11 cases) followed by testis and tonsils (four each).
| Fig. 5 Extranodal lymphoma
Cyclophosphamide, doxorubicin, vincristine, and prednisone regimen with or without rituximab is used in the management of NHLs in our setup.
Conflict of Interest
There are no conflicts of interest.
Acknowledgment
The authors are grateful to the Director, Dr. B. Borooah Cancer Institute, for allowing us to publish this article.
References
- 1 Huh J. Epidemiologic overview of malignant lymphoma. Korean J Hematol 2012; 47: 92-104
- 2 Boffetta P. Epidemiology of adult NHL. Ann Oncology 2011; 22: iv27-31
- 3 Ioachim HL, Medeiros LJ. editors Nomenclature and classification of lymphomas. In: Ioachim’s Lymph Node Pathology. 4th ed. Philadelphia, PA: JB Lippincott; 2008: 301
- 4 Naresh KN, Srinivas V, Soman CS. Distribution of various subtypes of non-Hodgkin’s lymphoma in India: A study of 2773 lymphomas using R.E.A.L. And WHO classifications. Ann Oncol 2000; 11 (01) Suppl 63-7
- 5 A clinical evaluation of the international lymphoma study group classification of non-Hodgkin’s lymphoma. The non-Hodgkin’s lymphoma classification project. Blood 1997; 89: 3909-18
Address for correspondence
Dr. Debanwita MahantaDepartment of Pathology, Dr. B. Borooah Cancer InstituteGopinath Nagar, Guwahati - 781 016, AssamIndiaEmail: mdebanwita@yahoo.comPublication History
Received: 07 June 2018
Accepted: 12 July 2019
Article published online:
03 June 2021© 2020. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/).
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
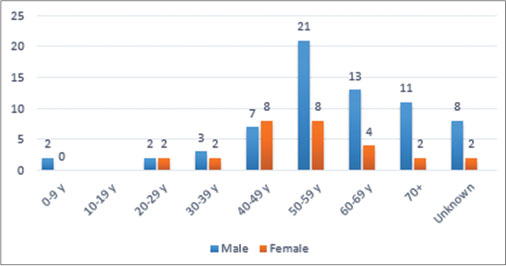
| Fig. 1 Age distribution of B-cell non-Hodgkin lymphoma
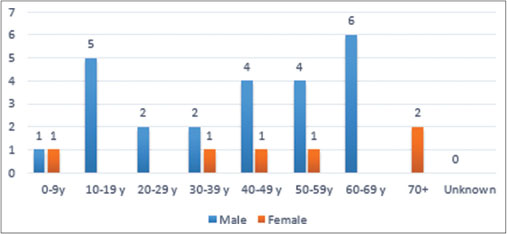
| Fig. 2 Age distribution of T-cell non-Hodgkin lymphoma
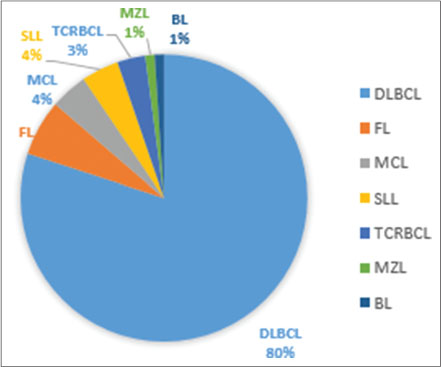
| Fig. 3 Subtypes of B-cell non-Hodgkin lymphoma
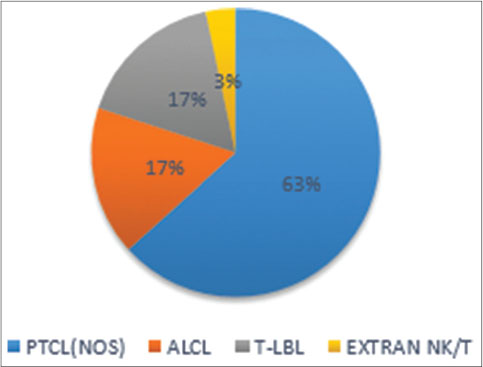
| Fig. 4 Subtypes of T-cell non-Hodgkin lymphoma
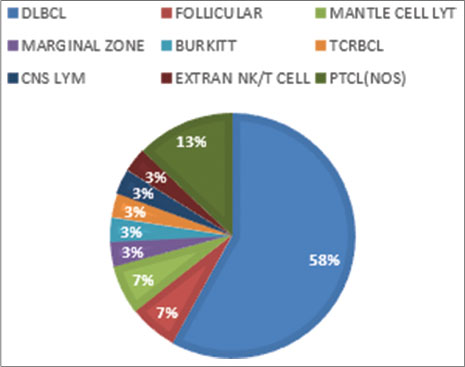
| Fig. 5 Extranodal lymphoma
References
- 1 Huh J. Epidemiologic overview of malignant lymphoma. Korean J Hematol 2012; 47: 92-104
- 2 Boffetta P. Epidemiology of adult NHL. Ann Oncology 2011; 22: iv27-31
- 3 Ioachim HL, Medeiros LJ. editors Nomenclature and classification of lymphomas. In: Ioachim’s Lymph Node Pathology. 4th ed. Philadelphia, PA: JB Lippincott; 2008: 301
- 4 Naresh KN, Srinivas V, Soman CS. Distribution of various subtypes of non-Hodgkin’s lymphoma in India: A study of 2773 lymphomas using R.E.A.L. And WHO classifications. Ann Oncol 2000; 11 (01) Suppl 63-7
- 5 A clinical evaluation of the international lymphoma study group classification of non-Hodgkin’s lymphoma. The non-Hodgkin’s lymphoma classification project. Blood 1997; 89: 3909-18


 PDF
PDF  Views
Views  Share
Share

