Peculiarities of Yolk Sac Tumor in Head and Neck: A Case Report and Literature Review
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2018; 39(02): 260-262
DOI: DOI: 10.4103/ijmpo.ijmpo_135_17
Abstract
Yolk sac tumor (YST) is the most common malignant germ cell tumor of head and neck region, constituting around 1% of all malignant germ cells. The rarity of the tumor has led to a relatively sparse collective description of clinical and prognostic factors of such a tumor affecting head and neck region. In this case report with review of the literature, we have highlighted certain peculiar features of YSTs affecting the head and neck region. They seem to commonly affect female children. These tumors seem to fare poorly in children of <1>
Publication History
Article published online:
23 June 2021
© 2018. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Yolk sac tumor (YST) is the most common malignant germ cell tumor of head and neck region, constituting around 1% of all malignant germ cells. The rarity of the tumor has led to a relatively sparse collective description of clinical and prognostic factors of such a tumor affecting head and neck region. In this case report with review of the literature, we have highlighted certain peculiar features of YSTs affecting the head and neck region. They seem to commonly affect female children. These tumors seem to fare poorly in children of <1>
Introduction
Yolk sac tumor (YST) also known as “endodermal sinus tumor” is the most common malignant germ cell tumor involving gonads. Although rare, these tumors are also known to arise from an extragonadal site including the head and neck region. While sharing a report of a large YST of temporal region in a 3-year-old boy, we are highlighting certain peculiarities of YST in the head and neck region.
Case Report
A 3-year-old boy presented with a painless, progressive swelling in the right temporal region for the
past 1 year. The swelling of 15 cm × 10 cm was involving temporal region, infratemporal fossa, and parotid region,
giving the appearance of a conjoint second head as shown radiologically in [Figure 1]. Open biopsy from the lesion showed mixed germ cell tumor consisting of teratoma and
YST. Whole-body positron emission tomography ruled out metastasis. He was given five cycles of cisplatin, bleomycin,
and etoposide combination chemotherapy, for which tumor responded significantly with 90% reduction in volume as
shown radiologically in [Figure 2]. Although the residual tumor was excised, the pathological examination of surgical
specimen did not show any residual tumor. The patient was kept under close follow-up, and he is disease free at 2
years postsurgery with serum alpha-fetoprotein levels of 0.88 ng/ml (normal range: 0.89–8.78 ng/ml) and beta-hCG
levels of 1.20 mIU/ml (normal range: <5>
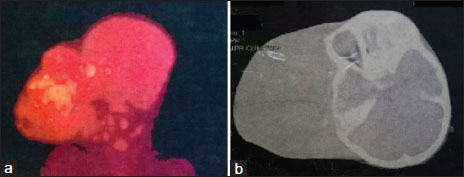
| Figure 1:Pretreatment radiological images: (a) positron emission tomography and (b) plain computer tomography, both showing huge tumor giving the appearance of conjoint head
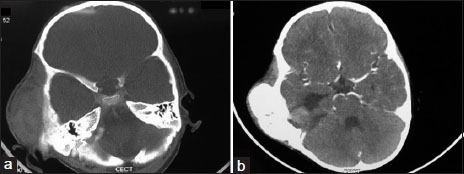
| Figure.2:Postchemotherapy radiological images: (a) plain computer tomography, (b) contrast enhanced computer tomography, both demonstrating significant reduction of tumor bulk following chemotherapy
Discussion
As per the MAKEI (Maligne Keimzelltumoren) group, the largest group to have prospectively studied the germ cell tumors of head and neck region, the YST in head and neck constitutes 1% of malignant germ cell tumors of the body.[1] [Table 1] depicts the most of the reported cases of YSTs involving head and neck region in the past 20 years.
|
Author |
Year |
Age (years) |
Sex |
Site |
Side |
Treatment |
Prognosis |
|---|---|---|---|---|---|---|---|
|
*Duration not available. NA – Not available; PPS – Parapharyngeal space; S – Surgical excision; CT – Chemotherapy; RT – Radiotherapy; DF – Disease-free |
|||||||
|
Kusumakumari et al.[2] |
1997 |
6 mn |
Female |
Orbit |
Left |
S |
Progression |
|
1.5 |
Male |
Palate |
NA |
S |
NA |
||
|
1 |
Female |
Skull base |
Right |
CT |
Progression |
||
|
Bresters et al.[3] |
2003 |
3 |
Female |
Sino-orbital |
Right |
CT + S + RT |
Progression |
|
Mishra et al.[4] |
2007 |
59 |
Male |
Sinonasal |
Right |
CT + S + RT |
DF at 1 year |
|
Kiratli et al.[5] |
2008 |
2yr 5mn |
Female |
Orbit |
Left |
S + CT |
DF at 9 years |
|
Fujino et al.[6] |
2009 |
4 |
Male |
Orbit |
Right |
CT + S |
DF at 1.5 year |
|
Furtado et al.[7] |
2011 |
10 |
Female |
Thyroid |
Right |
CT |
DF* |
|
Zhang et al.[8] |
2013 |
1yr 4mn |
Female |
Floor of mouth |
Bilateral |
S |
Progression |
|
Hauser et al.[9] |
2013 |
2 |
Female |
PPS |
Left |
CT + S |
DF at 1 year |
|
Arumugam et al.[10] |
2016 |
3 |
Female |
Skull base |
Bilateral |
S + CT |
DF* |
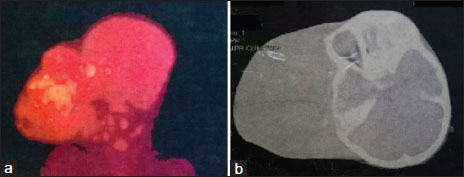
| Figure 1:Pretreatment radiological images: (a) positron emission tomography and (b) plain computer tomography, both showing huge tumor giving the appearance of conjoint head
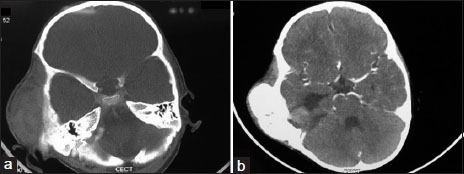
| Figure.2:Postchemotherapy radiological images: (a) plain computer tomography, (b) contrast enhanced computer tomography, both demonstrating significant reduction of tumor bulk following chemotherapy
References
- Bernbeck B, Schneider DT, Bernbeck B, Koch S, Teske C, Lentrodt J. et al. Germ cell tumors of the head and neck: Report from the MAKEI study group. Pediatr Blood Cancer 2009; 52: 223-6
- Kusumakumari P, Geetha N, Chellam VG, Nair MK. Endodermal sinus tumors in the head and neck region. Med Pediatr Oncol 1997; 29: 303-7
- Bresters D, Zwaan CM, Veerman AJ, Leemans CR, Westerveld GJ, van der LindenJC. et al. A three-year-old girl with a yolk sac tumor in the orbit/maxillary sinus. Med Pediatr Oncol 2003; 40: 70-1
- Mishra A, El-Naggar AK, DeMonte F, Hanna EY. et al. Endodermal sinus tumor of the paranasal sinuses. Head Neck 2008; 30: 539-43
- Kiratli H, Erkan BalciK, Güler G. Primary orbital endodermal sinus tumor (yolk sac tumor). J AAPOS 2008; 12: 623-5
- Fujino T, Okamura A, Hatsukawa Y, Nakayama K, Inoue M, Nakayama M. et al. A case of intraocular yolk sac tumor in a child and its pathogenesis. J AAPOS 2009; 13: 613-5
- Furtado LV, Leventaki V, Layfield LJ, Lowichik A, Muntz HR, Pysher TJ. et al. Yolk sac tumor of the thyroid gland: A case report. Pediatr Dev Pathol 2011; 14: 475-9
- Zhang Q, Huang Y, Bao CY, Li LJ. Yolk sac tumour involving floor of mouth: Case report. Br J Oral Maxillofac Surg 2013; 51: e67-9
- Hauser LJ, Chiang T, Ramakrishnan VR, Lovell MA, Kelley PE. Parapharyngeal and skull base yolk sac tumor: A case report with lessons in diagnosis and management. Int J Pediatr Otorhinolaryngol 2014; 78: 203-6
- ;Arumugam D, Thandavarayan P, Chidambaram L, Boj S, Marudasalam S. Primary nasopharngeal yolk sac tumor: A Case report. J Clin Diagn Res 2016; 10: ED06-7


 PDF
PDF  Views
Views  Share
Share

