Primary Intraosseous Malignant Peripheral Nerve Sheath Tumor of Metacarpal Bones of the Hand in a Patient Without Neurofibromatosis 1: Report of a Rare Case
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2017; 38(02): 232-235
DOI: DOI: 10.4103/ijmpo.ijmpo_5_17
Abstract
Malignant peripheral nerve sheath tumor (MPNST) usually arises in peripheral nerve sheath cells. The intraosseous location of MPNST is rare. Mandible is the most common site of bony involvement. Involvement of bones of the hand is quite unusual. We report a case of MPNST involving metacarpal bones of the left hand treated with surgery followed by adjuvant radiation and chemotherapy and review the pertinent literature.
Publication History
Article published online:
06 July 2021
© 2017. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Malignant peripheral nerve sheath tumor (MPNST) usually arises in peripheral nerve sheath cells. The intraosseous location of MPNST is rare. Mandible is the most common site of bony involvement. Involvement of bones of the hand is quite unusual. We report a case of MPNST involving metacarpal bones of the left hand treated with surgery followed by adjuvant radiation and chemotherapy and review the pertinent literature.
Introduction
Malignant peripheral nerve sheath tumor (MPNST) or malignant schwannoma is a malignant tumor arising from peripheral nerve sheath cells. The incidence of MPNST is suggested to be 0.0001%, and this tumor entity comprises 5%–10% of all soft-tissue tumors. Up to 50% of MPNSTs arise in patients with neurofibromatosis-1 (NF-1).[1] They usually arise in the soft-tissue and their origin from bones is rare. Mandible is the most commonly reported site of bony involvement.[2] There are isolated case reports of MPNST involving maxilla, spine, sternum, and long bones of extremities. Origin from small bones of hand and foot is exceptionally rare. There is one case report of the involvement of distal phalanx of the fifth toe.[3] To the best of our knowledge, there is no reported case of intraosseous MPNST of hand in medical literature to date. We herein report a case of primary intraosseous MPNST of hand in a 24-year-old male without any stigmata of NF-1.
Case Report
A 24-year-old male presented at a different center with a 1½-year history of gradually increasing swelling over dorsum of the left hand. He had no personal or family history of NF-1. X-ray of the left hand showed a lytic expansile lesion at the base of the third metacarpal bone. Contrast-enhanced magnetic resonance imaging (MRI) of the left hand revealed a 6.7 cm × 3.4 cm × 3.0 cm expansile destructive lesion involving the entire third metacarpal bone. The proximal and distal articular surfaces were free [Figure 1]. Biopsy showed pleomorphic round cell tumor with the possibility of Ewing's sarcoma in view of focal positivity of CD-99. Metastatic workup in the form of computerized tomography scan of chest, whole body bone scan, and bone marrow aspirate and biopsy was essentially normal.
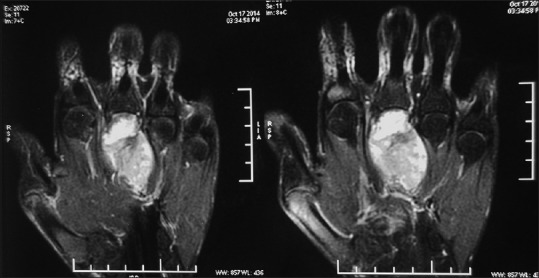
| Figure 1:Contrast-enhanced magnetic resonance imaging of the left hand showing a diffusely enhancing 6.7 cm × 3.4 cm × 3.0 cm expansile destructive lesion involving the entire third metacarpal bone sparing the proximal and distal articular surfaces
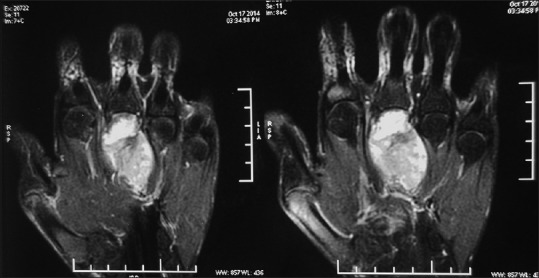
Four cycles of induction chemotherapy with vincristine, adriamycin, and cyclophosphamide (VAC) alternating with ifosfamide and etoposide (IE) regimen were administered as per the INT-0091 protocol.[4] A repeat MRI of the left hand showed an increase in the size of tumor to 7.3 cm × 3.8 cm × 3.7 cm. The tumor was involving the third metacarpal bone with extension into proximal and distal epiphysis. There was involvement of the third metacarpophalangeal joint, base of the second metacarpal bone, and the interosseous muscles [Figure 2].

| Figure 2:Repeat magnetic resonance imaging of the left hand after induction chemotherapy showing a 7.3 cm × 3.8 cm × 3.7 cm tumor involving the third metacarpal bone with extension into proximal and distal epiphysis, third metacarpophalangeal joint, base of the second metacarpal bone, and the interosseous muscles
In view of progressive disease, the patient was subsequently referred to our center for further management. He underwent excision of the tumor with nonvascular fibular grafting and prosthesis implant in the department of orthopedics. The fibula was articulated to the proximal phalanx using an artificial metacarpophalangeal joint. Postoperative histopathology revealed an encapsulated tumor of size 8.5 cm × 5.0 cm × 3.5 cm, with moderate-to-severe pleomorphism, increased mitosis, and focal necrosis. The tumor was very close to the resection margin (<1>Figure 3].
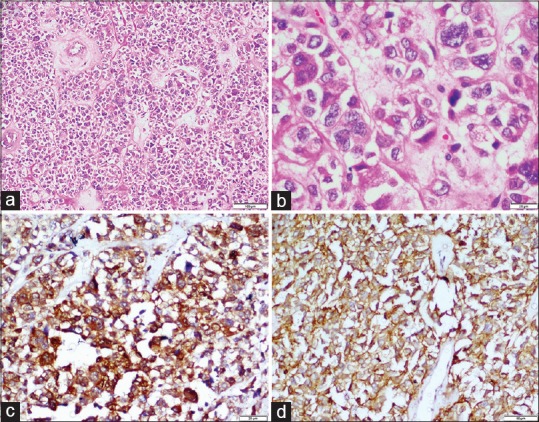
| Figure 3:Malignant epithelioid tumor cells in vague lobular arrangement (a, H and E, ×100). Tumor cells have large pleomorphic, hyperchromatic nuclei, clumped chromatin, irregular thick nuclear membrane, and moderate amount of eosinophilic cytoplasm (b, H and E, ×400). Tumor cells are strongly immunoreactive to neuron-specific enolase (c, ×200) and CD56 (d, ×200)
Adjuvant radiotherapy with a dose of 60 Gray in 30 fractions over 6 weeks was planned in view of large tumor size (>5 cm), close margin (<1 href="https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5582569/figure/F4/" target="figure" class="fig-table-link figpopup" rid-figpopup="F4" rid-ob="ob-F4" co-legend-rid="lgnd_F4" xss=removed>Figure 4]. Dose was prescribed at a depth of 3.5 cm. The patient was treated on telecobalt (Cobalt-60) Theratron 780 C machine. The patient tolerated the planned treatment well with grade 1 skin reaction.
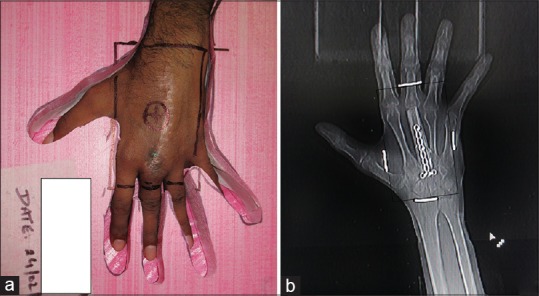
| Figure 4:Photograph of the radiation portal encompassing the postoperative scar (a) and the tumor bed (b) with a margin of 2 cm; the patient was simulated in swimmer's hand position using a customized styrofoam cutout for immobilization
Subsequently, the patient received four cycles of adjuvant chemotherapy with doxorubicin 25 mg/m2, day 1–3, and ifosfamide 1800 mg/m2, day 1–5, with mesna uroprotection (ifosfamide and adriamycin [IA]) regimen every 3 weeks in view of high-grade histology. On last follow-up visit, after 2 months of completion of adjuvant chemotherapy, the patient is clinically disease free.
Discussion
Intraosseous peripheral nerve sheath tumors are unusual and are usually benign. In a study at the Mayo Clinic, out of 3987 primary bone tumors, only six were intraosseous schwannomas.[5] MPNST is a malignant counterpart of schwannoma and mostly arises in soft tissue. It can arise de novo from myelinating Schwann cells of the nerve sheath or by malignant transformation in preexisting schwannoma. Mostly, it arises in nerves with long courses such as alveolar nerve, sciatic nerve, and nerves of the brachial plexus.
Primary intraosseous MPNST is very rare due to low density of sensory nerve fibers in bone. There are three mechanisms, which have been postulated for osseous involvement in MPNST.[6] Tumor may originally arise from the bone or it can arise from the soft tissue with subsequent invasion of the adjacent bone or involvement of the bone by infiltration through a nutrient foramen. Involvement of small bones of digits is exceptionally rare. There is only one case report of MPNST arising from the distal phalanx of the fifth toe.[3] Malignant sarcomas of the hand are very rare and constitute only 1–2% of hand tumors. Clemens et al. reported a case of nonosseous MPNST arising from the intermuscular planes of the first web space of the hand.[7] The tumor was involving the radial digital nerve. Rarity of the condition imposes considerable diagnostic dilemma.[7] Wood et al. reported a case of malignant schwannoma arising from the median nerve misdiagnosed as carpal tunnel syndrome.[8] In both the aforementioned cases, there was no intraosseous involvement by MPNST.[7,8] In the illustrative case, the tumor was initially misdiagnosed as Ewing's sarcoma and it progressed on induction chemotherapy with alternating VAC-IE regimen.
Preoperative clinical diagnosis is challenging particularly outside the NF-1 context. Differential diagnosis includes osteolytic lesions of bone such as aneurysmal bone cyst, malignant melanoma, clear cell sarcoma, lymphoma, plasmacytoma, and metastasis. Immunohistochemistry plays a seminal role in differentiating MPNST from other tumors. In a systematic review from the French Sarcoma Group Database, 18% of cases, initially diagnosed as MPNST, were reclassified after pathology review, IHC analysis, and molecular analysis.[9] Spindle cell MPNST was the most commonly encountered histologic subtype (71.8%). Only four (3.2%) cases of epithelioid MPNST were identified in this review.[9]
Gross total excision of tumor with clear margins is the goal of surgical treatment. Adverse prognostic factors include tumor size >5 cm, high-grade histology, positive or close margin status, and presence of NF-1 disease. Patients with these factors merit adjuvant treatment. In a French study of 160 patients with MPNST, positive margin (R1/R2 resection) and lack of adjuvant radiation therapy were independent predictors of local recurrence.[9] MPNSTs are considered high-grade tumors and are known for local recurrence as well as systemic metastasis to lung, liver, and bone. Kendi et al. reported a case of left ulnar MPNST in a 29-year-old male who developed local recurrence and pulmonary metastasis in the absence of adjuvant treatment.[10] MPNST involving bones of the digits is exceptionally rare. Iwama et al. reported a case of MPNST of the distal phalanx of the right fifth toe in a 76-year-old male treated with surgery alone without any adjuvant treatment. After 1 year of follow-up, the patient developed local recurrence as well as pulmonary metastasis.[3] Until recently, the role of chemotherapy in such tumors was not well established. In an updated meta-analysis of randomized controlled trials of adjuvant chemotherapy for localized resectable soft-tissue sarcoma, the use of adjuvant doxorubicin and ifosfamide significantly decreased local recurrence, distant recurrence, and death.[11] In a pooled analysis of individual patient data from the two largest adjuvant trials of chemotherapy in patients with localized high-grade soft-tissue sarcoma performed by the European Organisation for Research and Treatment of Cancer, use of adjuvant doxorubicin-based chemotherapy was associated with significant overall survival and relapse-free survival benefit in patients undergoing incomplete resection.[12] Considering this body of evidence, our patient received adjuvant radiation therapy and chemotherapy with IA regimen in view of large tumor size, high-grade histology, and close surgical margin.
Primary intraosseous MPNST of the hand is extremely rare, and the epithelioid subtype of MPNST is even rarer. On account of this rarity, it often poses vexing diagnostic challenge. Immunohistochemistry plays a pivotal role in establishing the correct diagnosis. The primary treatment aim should be gross total excision of the tumor with clear margins. Adjuvant radiotherapy should be given in patients with high-risk features, and the role of adjuvant chemotherapy needs to be carefully considered.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Moon SJ, Lee JK, Seo BR, Kim JH, Kim SH, Lee KH, et al. An intraosseous malignant peripheral nerve sheath tumor of the cervical spine: A case report and review of the literature. Spine (Phila Pa 1976) 2008;33:E712-6.
- Terry DG, Sauser DD, Gordon MD. Intraosseous malignant peripheral nerve sheath tumor in a patient with neurofibromatosis. Skeletal Radiol 1998;27:346-9.
- Iwama Y, Kunisada M, Goto H, Ohno Y, Yamashita J, Funasaka Y, et al. Malignant peripheral nerve sheath tumor of the distal phalanx of the fifth toe: A case report. Acta Radiol Short Rep 2014;3:2047981613516033.
- Grier HE, Krailo MD, Tarbell NJ, Link MP, Fryer CJ, Pritchard DJ, et al. Addition of ifosfamide and etoposide to standard chemotherapy for Ewing's sarcoma and primitive neuroectodermal tumor of bone. N Engl J Med 2003;348:694-701.
- Wirth WA, Bray CB Jr. Intra-osseous neurilemoma. Case report and review of thirty-one cases from the literature. J Bone Joint Surg Am 1977;59:252-5.
- Sham ME, Ghorpade, Shetty A, Hari S, Vinay. Malignant peripheral nerve cell tumour. J Maxillofac Oral Surg 2010;9:68-71.
- Clemens MW, Murthy A, Przygodzki RM. Malignant peripheral nerve sheath tumor of the hand. Plast Reconstr Surg 2009;123:83e-5e.
- Wood MK, Erdmann MW, Davies DM. Malignant schwannoma mistakenly diagnosed as carpal tunnel syndrome. J Hand Surg Br 1993;18:187-8.
- Le Guellec S, Decouvelaere AV, Filleron T, Valo I, Charon-Barra C, Robin YM, et al. Malignant peripheral nerve sheath tumor is a challenging diagnosis: A systematic pathology review, immunohistochemistry, and molecular analysis in 160 patients from the French Sarcoma Group Database. Am J Surg Pathol 2016;40:896-908.
- Kendi TK, Erakar A, Yildiz HY, Saglik Y, Erekul S. Intraosseous malignant peripheral nerve sheath tumor with local recurrence, lung metastases and death. Skeletal Radiol 2004;33:223-5.
- Pervaiz N, Colterjohn N, Farrokhyar F, Tozer R, Figueredo A, Ghert M. A systematic meta-analysis of randomized controlled trials of adjuvant chemotherapy for localized resectable soft-tissue sarcoma. Cancer 2008;113:573-81.
- Le Cesne A, Ouali M, Leahy MG, Santoro A, Hoekstra HJ, Hohenberger P, et al. Doxorubicin-based adjuvant chemotherapy in soft tissue sarcoma: Pooled analysis of two STBSG-EORTC phase III clinical trials. Ann Oncol 2014;25:2425-32.
| Figure 1:Contrast-enhanced magnetic resonance imaging of the left hand showing a diffusely enhancing 6.7 cm × 3.4 cm × 3.0 cm expansile destructive lesion involving the entire third metacarpal bone sparing the proximal and distal articular surfaces

| Figure 2:Repeat magnetic resonance imaging of the left hand after induction chemotherapy showing a 7.3 cm × 3.8 cm × 3.7 cm tumor involving the third metacarpal bone with extension into proximal and distal epiphysis, third metacarpophalangeal joint, base of the second metacarpal bone, and the interosseous muscles
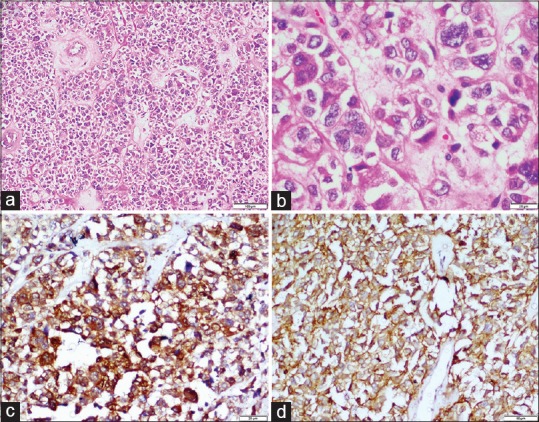
| Figure 3:Malignant epithelioid tumor cells in vague lobular arrangement (a, H and E, ×100). Tumor cells have large pleomorphic, hyperchromatic nuclei, clumped chromatin, irregular thick nuclear membrane, and moderate amount of eosinophilic cytoplasm (b, H and E, ×400). Tumor cells are strongly immunoreactive to neuron-specific enolase (c, ×200) and CD56 (d, ×200)
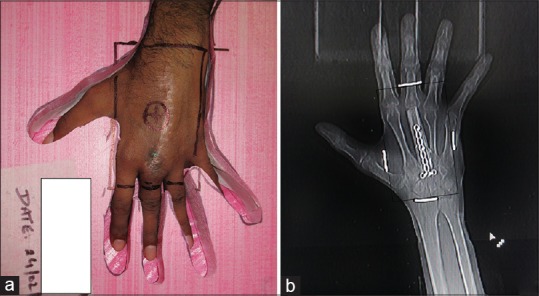
| Figure 4:Photograph of the radiation portal encompassing the postoperative scar (a) and the tumor bed (b) with a margin of 2 cm; the patient was simulated in swimmer's hand position using a customized styrofoam cutout for immobilization
References
- Moon SJ, Lee JK, Seo BR, Kim JH, Kim SH, Lee KH, et al. An intraosseous malignant peripheral nerve sheath tumor of the cervical spine: A case report and review of the literature. Spine (Phila Pa 1976) 2008;33:E712-6.
- Terry DG, Sauser DD, Gordon MD. Intraosseous malignant peripheral nerve sheath tumor in a patient with neurofibromatosis. Skeletal Radiol 1998;27:346-9.
- Iwama Y, Kunisada M, Goto H, Ohno Y, Yamashita J, Funasaka Y, et al. Malignant peripheral nerve sheath tumor of the distal phalanx of the fifth toe: A case report. Acta Radiol Short Rep 2014;3:2047981613516033.
- Grier HE, Krailo MD, Tarbell NJ, Link MP, Fryer CJ, Pritchard DJ, et al. Addition of ifosfamide and etoposide to standard chemotherapy for Ewing's sarcoma and primitive neuroectodermal tumor of bone. N Engl J Med 2003;348:694-701.
- Wirth WA, Bray CB Jr. Intra-osseous neurilemoma. Case report and review of thirty-one cases from the literature. J Bone Joint Surg Am 1977;59:252-5.
- Sham ME, Ghorpade, Shetty A, Hari S, Vinay. Malignant peripheral nerve cell tumour. J Maxillofac Oral Surg 2010;9:68-71.
- Clemens MW, Murthy A, Przygodzki RM. Malignant peripheral nerve sheath tumor of the hand. Plast Reconstr Surg 2009;123:83e-5e.
- Wood MK, Erdmann MW, Davies DM. Malignant schwannoma mistakenly diagnosed as carpal tunnel syndrome. J Hand Surg Br 1993;18:187-8.
- Le Guellec S, Decouvelaere AV, Filleron T, Valo I, Charon-Barra C, Robin YM, et al. Malignant peripheral nerve sheath tumor is a challenging diagnosis: A systematic pathology review, immunohistochemistry, and molecular analysis in 160 patients from the French Sarcoma Group Database. Am J Surg Pathol 2016;40:896-908.
- Kendi TK, Erakar A, Yildiz HY, Saglik Y, Erekul S. Intraosseous malignant peripheral nerve sheath tumor with local recurrence, lung metastases and death. Skeletal Radiol 2004;33:223-5.
- Pervaiz N, Colterjohn N, Farrokhyar F, Tozer R, Figueredo A, Ghert M. A systematic meta-analysis of randomized controlled trials of adjuvant chemotherapy for localized resectable soft-tissue sarcoma. Cancer 2008;113:573-81.
- Le Cesne A, Ouali M, Leahy MG, Santoro A, Hoekstra HJ, Hohenberger P, et al. Doxorubicin-based adjuvant chemotherapy in soft tissue sarcoma: Pooled analysis of two STBSG-EORTC phase III clinical trials. Ann Oncol 2014;25:2425-32.


 PDF
PDF  Views
Views  Share
Share

