Protean Neuroophthalmic Presentations of Common Childhood Malignancies—A Report of Two Cases
CC BY 4.0 · Indian J Med Paediatr Oncol 2023; 44(03): 360-364
DOI: DOI: 10.1055/s-0043-1761610
Abstract
Common pediatric malignancies often surprise clinicians with unusual presentations. In this narrative, we report two patients with common childhood cancer having unique neuroophthalmic characteristics. In the first case, we have a child with a common childhood solid tumor presenting with blindness without proptosis, while the second case is of a child with a common hematological malignancy presenting with unilateral proptosis without visual impairment. The report highlights that common childhood cancers may present with neuroophthalmic symptoms on rare occasions, creating a diagnostic conundrum.
Declaration of Patient Consent
The authors certify that they have obtained consent from the parents for the publication of images and clinical information of the child in the journal. The parents understand that the child's name and initials will not be published and due efforts will be made to conceal the identity.
Publication History
Article published online:
12 May 2023
© 2023. The Author(s). This is an open access article published by Thieme under the terms of the Creative Commons Attribution License, permitting unrestricted use, distribution, and reproduction so long as the original work is properly cited. (https://creativecommons.org/licenses/by/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Common pediatric malignancies often surprise clinicians with unusual presentations. In this narrative, we report two patients with common childhood cancer having unique neuroophthalmic characteristics. In the first case, we have a child with a common childhood solid tumor presenting with blindness without proptosis, while the second case is of a child with a common hematological malignancy presenting with unilateral proptosis without visual impairment. The report highlights that common childhood cancers may present with neuroophthalmic symptoms on rare occasions, creating a diagnostic conundrum.
neuroophthalmic symptoms Introduction
Childhood malignancies may present with nonspecific and overlapping clinical features, making it difficult to differentiate them from each other clinically. They often puzzle clinicians and pose interesting diagnostic challenges.[1] [2] [3] [4] [5] [6] [7] We describe two unique neuroophthalmological presentations of common childhood malignancies in this report.
Case 1
A 6-year-old boy presented with a 2-week history of headache and painless, progressive binocular vision loss. There was a preceding history of intermittent fever for 2 months, nocturnal bone pains, and recent-onset anemia, requiring a transfusion. He had severe bilateral visual impairment at presentation, with only the perception of light present. There was no obvious proptosis or raccoon eye. Fundoscopy revealed bilateral blurring of disk margins without optic atrophy. Severe pallor, generalized bony tenderness, and hepatomegaly were present on examination. Sutural diastasis was noted at sagittal and coronal sutures. The constellation of clinical presentation and the examination findings raised suspicion of acute leukemia or metastatic neuroblastoma.
Skull radiograph revealed remarkable sutural diastasis ([Fig. 1A]). A contrast-enhanced magnetic resonance imaging (CE-MRI) of the brain and orbit unveiled multiple intracranial, extradural collections over bilateral frontoparietal and occipital areas ([Fig. 1B]). Soft-tissue depositions over the orbital apices causing bilateral optic nerve compression were also evident, explaining the binocular blindness. A bone marrow (BM) aspiration and bilateral trephine demonstrated clusters of small, round, blue tumor cells ([Fig. 1C]), with immunohistochemistry indicating a positivity for neuron-specific enolase, CD 56, and CD 81 ([Fig. 1D]), confirming the presence of metastatic neuroblastoma in the BM. Computed tomography and a DOTATATE positron emission tomography scan were done for staging, showing a left suprarenal mass (size: 15 × 12 mm), with extensive metastasis to bones, BM, and cranial meninges over fronto–parieto–occipital regions. Treatment for high-risk neuroblastoma was initiated with the rapid COJEC protocol.[8] [9] There was an improvement in the systemic symptoms. However, the vision loss did not recover. A reassessment was performed after eight cycles of induction chemotherapy, demonstrating extensive BM disease. After a detailed discussion with the family, a decision to proceed with palliative care was taken.
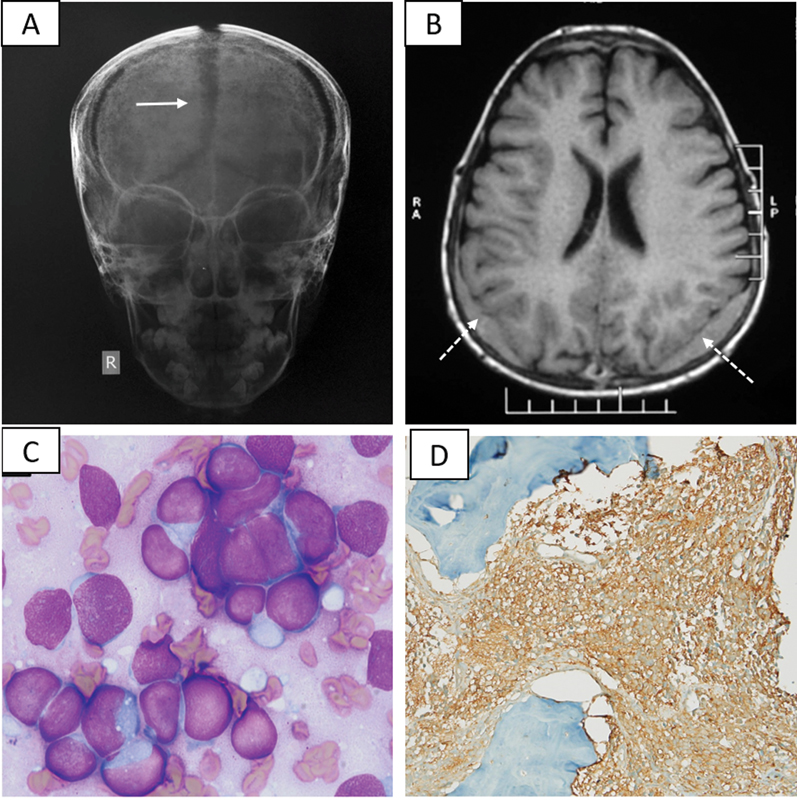
| Fig 1 :(A) Antero-posterior view of the skull radiograph showing remarkable sutural diastasis (white arrow), (B) axial section of T1-weighted MRI of the brain illustrating extradural soft tissue deposits along bilateral parieto-occipital regions (white dotted arrows), (C) bone marrow aspirate smear showing infiltration by blastoid atypical cells, and (D) immunohistochemistry demonstrating positivity for neuronspecific enolase
Case 2
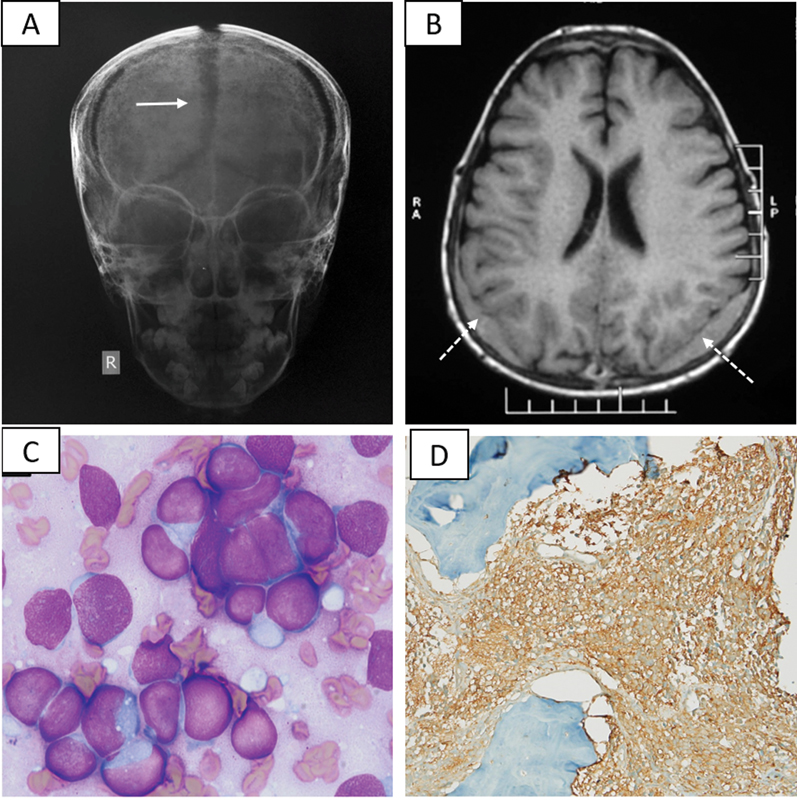
A 3-year-old boy presented with proptosis involving the left eye for 1 month without pain, visual impairment, or systemic symptoms. Physical examination was unremarkable, except for nonaxial proptosis with esotropia and periocular fullness in the left eye ([Fig. 2A]). A CE-MRI of the brain and orbit was performed and demonstrated a homogeneously enhancing soft tissue mass involving the basisphenoid with extension into the left orbit ([Fig. 2B]). Dura-based, multifocal, nodular, enhancing soft-tissue deposits along the left frontoparietal convexity were also apparent. Clinicoradiological possibilities of metastatic neuroblastoma and parameningeal rhabdomyosarcoma were considered. Abdominal ultrasonography and chest radiograph were normal. The tumor was at a difficult site to access for a biopsy. While a complete blood count was normal at the baseline, a repeat evaluation after 7 days revealed evolving cytopenias with a hemoglobin of 95 g/L, total leukocyte count of 4.17 × 109 /L, differential leukocyte count of polymorphs: 23%, lymphocytes: 60%, monocytes: 16%, and a platelet count of 165 × 109 /L. Subsequent BM aspiration revealed findings consistent with acute leukemia ([Fig. 2C]). Flow cytometry confirmed the presence of T cell acute lymphoblastic leukemia (ALL). Cerebrospinal fluid was paucicellular (three cells/µL), and cytospin did not detect leukemic infiltration. However, the child was considered “central nervous system (CNS)-positive” due to the MRI findings suggestive of leptomeningeal carcinomatosis. Induction chemotherapy was initiated for high-risk T cell ALL as per the Indian Childhood Collaborative Leukaemia Group protocol.[10] The proptosis resolved 2 weeks into treatment. Reassessment by BM, MRI brain, and 18-fluorodeoxyglucose-positron emission tomography confirmed remission at the end of consolidation. The child will subsequently receive CNS radiotherapy as a part of the treatment protocol.

| Figure 2:(A) Proptosis of the left eye, (B) sagittal section of T1-weighted CE-MRI of brain illustrating enhancing sheet of soft tissue at the basisphenoid with extension to the orbit (black arrow), (C) bone marrow aspirate smear showing blasts (May–Grunwald–Giemsa stain; 1,000x), (D) the blast cells were MPO negative (myeloperoxidase stain; 1,000x). CE-MRI, contrast-enhanced magnetic resonance imaging.
Discussion
Childhood cancers can have protean presentations. Extracranial malignancies may infiltrate the brain or the orbit and may be the initial manifestation of the disease.[11] [12] [13] [14] [15] [16] The unique presenting features of the cases in the current report are binocular painless visual loss in the absence of proptosis or raccoon's eye in a child with metastatic neuroblastoma, unilateral proptosis being the sole manifestation of T cell ALL in a young boy.
While malignancy was correctly suspected in both cases, the initial possibilities that were considered were different from the final diagnosis. Tissue diagnosis was rendered difficult due to the CNS location of the mass lesions, with BM aspiration and trephine clinching the diagnosis.
Orbital involvement is frequent in patients with metastatic neuroblastoma; raccoon's eye and proptosis are well-recognized manifestations. However, a presentation with visual loss without proptosis, as seen in case 2, is a rarity. [Table 1] summarizes the limited reports of orbital metastasis of neuroblastoma presenting with blindness without proptosis.[11] [12] [13] [17] [18] Treatment modalities to salvage vision have included steroids, decompressive surgery, and initiation of chemotherapy to treat the primary disease. The vision remained compromised in the majority of the reported cases, and the role of either steroids or surgery in salvaging the vision is not clear. Orbital metastasis of neuroblastoma confers a poor outcome, partially explained by a higher association with MYCN amplification.[19] [20] [21]
|
S No. |
Author, year of publication, country |
Number of patients |
Age |
Duration of blindness; visual acuity at diagnosis |
Site of optic nerve compression by metastatic tumor |
Treatment |
Visual outcome; final acuity |
Oncologic outcome |
|---|---|---|---|---|---|---|---|---|
|
1. |
Roy et al[17], 2021, India |
1 |
3 y and 9 mo |
2 wk; perception of light only |
Optic canal; bilateral |
High-dose dexamethasone, rapid COJEC chemotherapy |
No improvement |
On therapy |
|
2. |
Sivakumar et al [18], 2006, USA |
1 |
4 y |
2 wk; 20/200 |
Optic canal; bilateral |
Not included |
Not included |
Not included |
|
3. |
McGirt et al[11], 2005, USA |
1 |
33 mo |
4 d; no perception of light |
Optic foramen; bilateral |
High-dose methylprednisolone, decompressive surgery |
Partial improvement; finger counting, recognizing faces and printed book characters |
Not included |
|
4. |
Lau et al[12], 2004, USA |
1 |
2 y |
Several days; no perception of light |
Intracranial course; bilateral |
High-dose steroid |
Partial improvement; right eye-20/400 , left eye-hand movements |
In clinical remission |
|
5. |
Varma et al[13], 2003, United Kingdom |
1 |
2.5 y |
3 wk; hand movement perceived |
Orbital apices; bilateral |
Pulse methylprednisolone |
Right eye-partial improvement; 6/60, left eye-no improvement |
Not included |
|
6. |
Current report |
1 |
6 y |
2 wk; no perception of light |
Orbital apices; bilateral |
Rapid COJEC chemotherapy |
No improvement |
Refractory disease |
|
S No. |
Author, year of publication, Country |
Number of the patient(s) |
Age |
Ophthalmic features |
Radiology |
Oncologic diagnosis |
Mode of diagnosis |
Outcome |
|---|---|---|---|---|---|---|---|---|
|
1. |
Wang et al[22], 2020, China |
1 |
4 y |
Unilateral proptosis |
Orbital extraconal mass |
Hypodiploid B-cell ALL |
Bone marrow study |
Well on therapy |
|
2. |
Sathitsamitphong et al[23], 2019, Thailand |
1 |
3 y |
Unilateral proptosis |
Orbital mass with intracranial extension |
B-cell ALL |
Bone marrow study |
In remission; on therapy |
|
3. |
Sivaperumal et al[24], 2018, India |
1 |
5 y |
Bilateral proptosis |
Not included |
B-cell ALL |
Bone marrow study |
In remission; on therapy |
|
4. |
Ramamoorthy et al[25], 2016, India |
1 |
4 y |
Unilateral proptosis |
Retrobulbar mass with intracranial extension |
B-cell ALL |
Biopsy from the orbital mass and bone marrow study |
Well on therapy |
|
5. |
Thakker et al[26], 2006, India |
1 |
8 mo |
Right eye tearing, lid swelling, proptosis |
Large, homogeneous orbital mass causing axial displacement of the globe and expansion of the orbit |
B-cell ALL |
Bone marrow study |
Alive and well 14 mo posttreatment |
|
6. |
Current report |
1 |
3 y |
Unilateral proptosis |
Mass over basisphenoid with extension into the left orbit |
T-cell ALL |
Bone marrow study |
Doing well on therapy |
References
- Gökçe M, Aytaç S, Ünal Ş, Altan İ, Gümrük F, Çetin M. Acute megakaryoblastic leukemia with t(1;22) mimicking neuroblastoma in an infant. Turk J Haematol 2015; 32 (01) 64-67
- Kawasaki Y, Makimoto M, Nomura K. et al. Neonatal acute megakaryoblastic leukemia mimicking congenital neuroblastoma. Clin Case Rep 2015; 3 (03) 145-149
- Wang YM, Mo JQ, Kuo DJ, Wong V. MLL rearranged acute lymphoblastic leukaemia presenting as a maxillary sinus mass with a discordant immunophenotypic profile from the bone marrow. BMJ Case Rep 2019; 12 (02) e227400
- Ünal Ş, Kuşkonmaz B, Balcı YI. et al. An unusual presentation of pediatric acute lymphoblastic leukemia with parotid gland involvement and dactylitis. Turk J Haematol 2010; 27 (02) 117-119
- Sadawaite S, Jijina F, Nair CK, Seth S, Ghosh K. An unusual presentation of pediatric acute lymphoblastic leukemia. Indian J Hematol Blood Transfus 2008; 24 (02) 59-62
- Gallagher BL, Vibhakar R, Kao S, Cooper CS. Bilateral testicular masses: an unusual presentation of neuroblastoma. Urology 2006; 68 (03) 672.e15-672.e17
- Mittal D, Mandelia A, Bajpai M, Agarwala S. Adrenal neuroblastoma with metastatic mandibular mass: an unusual presentation. J Cancer Res Ther 2015; 11 (03) 645
- Ladenstein R, Pötschger U, Valteau-Couanet D. et al. Interleukin 2 with anti-GD2 antibody ch14.18/CHO (dinutuximab beta) in patients with high-risk neuroblastoma (HR-NBL1/SIOPEN): a multicentre, randomised, phase 3 trial. Lancet Oncol 2018; 19 (12) 1617-1629
- Jain R, Hans R, Totadri S. et al. Autologous stem cell transplant for high-risk neuroblastoma: achieving cure with low-cost adaptations. Pediatr Blood Cancer 2020; 67 (06) e28273
- Das N, Banavali S, Bakhshi S. et al. Protocol for ICiCLe-ALL-14 (InPOG-ALL-15-01): a prospective, risk stratified, randomised, multicentre, open label, controlled therapeutic trial for newly diagnosed childhood acute lymphoblastic leukaemia in India. Trials 2022; 23 (01) 102
- McGirt MJ, Cowan Jr JA, Gala V, Garton HJ, Muraszko KM, Thompson BG. Surgical reversal of prolonged blindness from a metastatic neuroblastoma. Childs Nerv Syst 2005; 21 (07) 583-586
- Lau JJC, Trobe JD, Ruiz RE. et al. Metastatic neuroblastoma presenting with binocular blindness from intracranial compression of the optic nerves. J Neuroophthalmol 2004; 24 (02) 119-124
- Varma D, George N, Livingston J, Negi A, Willshaw HE. Acute visual loss as an early manifestation of metastatic neuroblastoma. Eye (Lond) 2003; 17 (02) 250-252
- Belgaumi AF, Kauffman WM, Jenkins JJ. et al. Blindness in children with neuroblastoma. Cancer 1997; 80 (10) 1997-2004
- Taylor CW, Taylor RE, Kinsey SE. Leukemic infiltration of the orbit: report of three cases and literature review. Pediatr Hematol Oncol 2005; 22 (05) 415-422
- Bidar M, Wilson MW, Laquis SJ. et al. Clinical and imaging characteristics of orbital leukemic tumors. Ophthal Plast Reconstr Surg 2007; 23 (02) 87-93
- Roy PS, Chhabra P, Jain R, Gupta P, Sodhi KS, Bansal D. Metastatic, bilateral adrenal neuroblastoma presenting with blindness without proptosis. J Pediatr Hematol Oncol 2021; 43 (08) e1250-e1252
- Sivakumar S, Poulik J, Sivaswamy L. Monocular blindness as presentation manifestation of neuroblastoma. Neurohospitalist 2016; 6 (01) 41
- Smith SJ, Diehl NN, Smith BD, Mohney BG. Incidence, ocular manifestations, and survival in children with neuroblastoma: a population-based study. Am J Ophthalmol 2010; 149 (04) 677-682.e2
- Harreld JH, Bratton EM, Federico SM. et al. Orbital metastasis is associated with decreased survival in stage M neuroblastoma. Pediatr Blood Cancer 2016; 63 (04) 627-633
- DuBois SG, Kalika Y, Lukens JN. et al. Metastatic sites in stage IV and IVS neuroblastoma correlate with age, tumor biology, and survival. J Pediatr Hematol Oncol 1999; 21 (03) 181-189
- Wang L, Ashraf DC, Kinde B, Ohgami RS, Kumar J, Kersten RC. Hypodiploid B-lymphoblastic leukemia presenting as an isolated orbital mass prior to systemic involvement: a case report and review of the literature. Diagnostics (Basel) 2020; 11 (01) 25
- Sathitsamitphong L, Natesirinilkul R, Choeyprasert W, Charoenkwan P. Unusual presentation with orbital mass in a child with precursor B-cell acute lymphoblastic leukemia. Case Rep Hematol 2019; 2019: 8264689
- Sivaperumal PR, Latha SM, Narayani S, Scott J. Bilateral proptosis in a child: a rare presentation of acute lymphoblastic leukemia. J Ophthalmic Vis Res 2018; 13 (04) 511-513
- Ramamoorthy J, Jain R, Trehan A, Saxena AK, Ahluwalia J. Orbital mass in a child with acute lymphoblastic leukemia: a case report and review of the literature. J Pediatr Hematol Oncol 2016; 38 (08) 646-648
- Thakker MM, Rubin PAD, Chang E. Pre-B-cell acute lymphoblastic leukemia presenting as an orbital mass in an 8-month-old. Ophthalmology 2006; 113 (02) 343-346
Address for correspondence
Richa Jain, DMPediatric Hematology-Oncology Unit, Department of Pediatrics, Advanced Pediatrics Centre, Postgraduate Institute of Medical Education and ResearchChandigarh 160012IndiaEmail: docrichajain@gmail.comPublication History
Article published online:
12 May 2023© 2023. The Author(s). This is an open access article published by Thieme under the terms of the Creative Commons Attribution License, permitting unrestricted use, distribution, and reproduction so long as the original work is properly cited. (https://creativecommons.org/licenses/by/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
| Fig 1 :(A) Antero-posterior view of the skull radiograph showing remarkable sutural diastasis (white arrow), (B) axial section of T1-weighted MRI of the brain illustrating extradural soft tissue deposits along bilateral parieto-occipital regions (white dotted arrows), (C) bone marrow aspirate smear showing infiltration by blastoid atypical cells, and (D) immunohistochemistry demonstrating positivity for neuronspecific enolase

| Figure 2:(A) Proptosis of the left eye, (B) sagittal section of T1-weighted CE-MRI of brain illustrating enhancing sheet of soft tissue at the basisphenoid with extension to the orbit (black arrow), (C) bone marrow aspirate smear showing blasts (May–Grunwald–Giemsa stain; 1,000x), (D) the blast cells were MPO negative (myeloperoxidase stain; 1,000x). CE-MRI, contrast-enhanced magnetic resonance imaging.
References
- Gökçe M, Aytaç S, Ünal Ş, Altan İ, Gümrük F, Çetin M. Acute megakaryoblastic leukemia with t(1;22) mimicking neuroblastoma in an infant. Turk J Haematol 2015; 32 (01) 64-67
- Kawasaki Y, Makimoto M, Nomura K. et al. Neonatal acute megakaryoblastic leukemia mimicking congenital neuroblastoma. Clin Case Rep 2015; 3 (03) 145-149
- Wang YM, Mo JQ, Kuo DJ, Wong V. MLL rearranged acute lymphoblastic leukaemia presenting as a maxillary sinus mass with a discordant immunophenotypic profile from the bone marrow. BMJ Case Rep 2019; 12 (02) e227400
- Ünal Ş, Kuşkonmaz B, Balcı YI. et al. An unusual presentation of pediatric acute lymphoblastic leukemia with parotid gland involvement and dactylitis. Turk J Haematol 2010; 27 (02) 117-119
- Sadawaite S, Jijina F, Nair CK, Seth S, Ghosh K. An unusual presentation of pediatric acute lymphoblastic leukemia. Indian J Hematol Blood Transfus 2008; 24 (02) 59-62
- Gallagher BL, Vibhakar R, Kao S, Cooper CS. Bilateral testicular masses: an unusual presentation of neuroblastoma. Urology 2006; 68 (03) 672.e15-672.e17
- Mittal D, Mandelia A, Bajpai M, Agarwala S. Adrenal neuroblastoma with metastatic mandibular mass: an unusual presentation. J Cancer Res Ther 2015; 11 (03) 645
- Ladenstein R, Pötschger U, Valteau-Couanet D. et al. Interleukin 2 with anti-GD2 antibody ch14.18/CHO (dinutuximab beta) in patients with high-risk neuroblastoma (HR-NBL1/SIOPEN): a multicentre, randomised, phase 3 trial. Lancet Oncol 2018; 19 (12) 1617-1629
- Jain R, Hans R, Totadri S. et al. Autologous stem cell transplant for high-risk neuroblastoma: achieving cure with low-cost adaptations. Pediatr Blood Cancer 2020; 67 (06) e28273
- Das N, Banavali S, Bakhshi S. et al. Protocol for ICiCLe-ALL-14 (InPOG-ALL-15-01): a prospective, risk stratified, randomised, multicentre, open label, controlled therapeutic trial for newly diagnosed childhood acute lymphoblastic leukaemia in India. Trials 2022; 23 (01) 102
- McGirt MJ, Cowan Jr JA, Gala V, Garton HJ, Muraszko KM, Thompson BG. Surgical reversal of prolonged blindness from a metastatic neuroblastoma. Childs Nerv Syst 2005; 21 (07) 583-586
- Lau JJC, Trobe JD, Ruiz RE. et al. Metastatic neuroblastoma presenting with binocular blindness from intracranial compression of the optic nerves. J Neuroophthalmol 2004; 24 (02) 119-124
- Varma D, George N, Livingston J, Negi A, Willshaw HE. Acute visual loss as an early manifestation of metastatic neuroblastoma. Eye (Lond) 2003; 17 (02) 250-252
- Belgaumi AF, Kauffman WM, Jenkins JJ. et al. Blindness in children with neuroblastoma. Cancer 1997; 80 (10) 1997-2004
- Taylor CW, Taylor RE, Kinsey SE. Leukemic infiltration of the orbit: report of three cases and literature review. Pediatr Hematol Oncol 2005; 22 (05) 415-422
- Bidar M, Wilson MW, Laquis SJ. et al. Clinical and imaging characteristics of orbital leukemic tumors. Ophthal Plast Reconstr Surg 2007; 23 (02) 87-93
- Roy PS, Chhabra P, Jain R, Gupta P, Sodhi KS, Bansal D. Metastatic, bilateral adrenal neuroblastoma presenting with blindness without proptosis. J Pediatr Hematol Oncol 2021; 43 (08) e1250-e1252
- Sivakumar S, Poulik J, Sivaswamy L. Monocular blindness as presentation manifestation of neuroblastoma. Neurohospitalist 2016; 6 (01) 41
- Smith SJ, Diehl NN, Smith BD, Mohney BG. Incidence, ocular manifestations, and survival in children with neuroblastoma: a population-based study. Am J Ophthalmol 2010; 149 (04) 677-682.e2
- Harreld JH, Bratton EM, Federico SM. et al. Orbital metastasis is associated with decreased survival in stage M neuroblastoma. Pediatr Blood Cancer 2016; 63 (04) 627-633
- DuBois SG, Kalika Y, Lukens JN. et al. Metastatic sites in stage IV and IVS neuroblastoma correlate with age, tumor biology, and survival. J Pediatr Hematol Oncol 1999; 21 (03) 181-189
- Wang L, Ashraf DC, Kinde B, Ohgami RS, Kumar J, Kersten RC. Hypodiploid B-lymphoblastic leukemia presenting as an isolated orbital mass prior to systemic involvement: a case report and review of the literature. Diagnostics (Basel) 2020; 11 (01) 25
- Sathitsamitphong L, Natesirinilkul R, Choeyprasert W, Charoenkwan P. Unusual presentation with orbital mass in a child with precursor B-cell acute lymphoblastic leukemia. Case Rep Hematol 2019; 2019: 8264689
- Sivaperumal PR, Latha SM, Narayani S, Scott J. Bilateral proptosis in a child: a rare presentation of acute lymphoblastic leukemia. J Ophthalmic Vis Res 2018; 13 (04) 511-513
- Ramamoorthy J, Jain R, Trehan A, Saxena AK, Ahluwalia J. Orbital mass in a child with acute lymphoblastic leukemia: a case report and review of the literature. J Pediatr Hematol Oncol 2016; 38 (08) 646-648
- Thakker MM, Rubin PAD, Chang E. Pre-B-cell acute lymphoblastic leukemia presenting as an orbital mass in an 8-month-old. Ophthalmology 2006; 113 (02) 343-346


 PDF
PDF  Views
Views  Share
Share

