Protection behaviors for cytotoxic drugs in oncology nurses of chemotherapy centers in Shiraz hospitals, South of Iran
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2016; 37(04): 227-231
DOI: DOI: 10.4103/0971-5851.195748
Abstract
Context: The use of antineoplastic agents for the treatment of cancer is an increasingly common practice in hospitals. As a result, workers involved with handling antineoplastic drugs may be accidentally exposed to these agents, placing them at potential risk for long-term adverse effects. This study aimed to determine the occupational protection status of clinical nursing staff exposed to cytotoxic drugs. Subjects and Methods: The study was designed as an analytic descriptive survey. The research settings took place in six centers of chemotherapy in Shiraz, Iran. The participants were 86 nurses who worked in oncology units and administered cytotoxic drugs. Data were collected using a questionnaire and a checklist which was developed by the investigators to determine occupational protection status of clinical nursing staff exposed to cytotoxic drugs. Percentage calculations and the independent samples t-test were used to see the general distribution and analysis of data. To statistically analyze of the data, SPSS software (version 16) was applied. Results: The mean age of participants was 30.52 ± 6.50 years and 66.27% of the nurses worked on inpatient oncology wards. The mean practice score was 21.1 ± 3.76 that ranged from 12.5 to 31. The independent samples t-test showed the outpatient nurses were weaker in practice (17.2 ± 2.52) in comparison with university hospitals (23.35 ± 3.02, P< 0.001). Occupational protection status of clinical nursing staff exposed to cytotoxic drugs especially during administration and disposal of medicines was poor and rarely trained with this subject and was observed under the standard conditions. Conclusions: There is deficiency in the understanding and related protection practices of clinical nursing staff vocationally exposed to cytotoxic drugs. It is recommended that all clinical nursing staff should receive full occupational protection training about these matters and the authorities provide standard conditions of oncology wards.
Publication History
Article published online:
12 July 2021
© 2016. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Context:
The use of antineoplastic agents for the treatment of cancer is an increasingly common practice in hospitals. As a result, workers involved with handling antineoplastic drugs may be accidentally exposed to these agents, placing them at potential risk for long-term adverse effects. This study aimed to determine the occupational protection status of clinical nursing staff exposed to cytotoxic drugs.
Subjects and Methods:
The study was designed as an analytic descriptive survey. The research settings took place in six centers of chemotherapy in Shiraz, Iran. The participants were 86 nurses who worked in oncology units and administered cytotoxic drugs. Data were collected using a questionnaire and a checklist which was developed by the investigators to determine occupational protection status of clinical nursing staff exposed to cytotoxic drugs. Percentage calculations and the independent samples t-test were used to see the general distribution and analysis of data. To statistically analyze of the data, SPSS software (version 16) was applied.
Results:
The mean age of participants was 30.52 ± 6.50 years and 66.27% of the nurses worked on inpatient oncology wards. The mean practice score was 21.1 ± 3.76 that ranged from 12.5 to 31. The independent samples t-test showed the outpatient nurses were weaker in practice (17.2 ± 2.52) in comparison with university hospitals (23.35 ± 3.02, P < 0.001). Occupational protection status of clinical nursing staff exposed to cytotoxic drugs especially during administration and disposal of medicines was poor and rarely trained with this subject and was observed under the standard conditions.
Conclusions:
There is deficiency in the understanding and related protection practices of clinical nursing staff vocationally exposed to cytotoxic drugs. It is recommended that all clinical nursing staff should receive full occupational protection training about these matters and the authorities provide standard conditions of oncology wards.
INTRODUCTION
Due to the increased incidence of cancer, the production and use of antitumor drugs is on the rise. Majority of antitumor drugs, cytotoxic, which may cause cancer, mutations, and other effects.[1] Several studies revealed side-effects of these drugs on health workers, For instance, the increasing chance of chromosomal damages,[2,3,4,5] the decrease in the immune system,[6] increasing possibility of infertility and abortion,[7,8] premature labor,[9] low birth weight,[10] irritation of the eyes, skin and mucosa and allergic reactions due to skin contacts, vomiting, headache and dizziness, hair loss, and liver damages are the mentioned side-effects.[8,11] As a result, increased concern of handling these drugs by the pharmacy team, nurses, and physicians.
Till date, the challenge of protecting workers’ health is persisting and expanding, with an increasing number of publications demonstrating that contamination of cytotoxic drugs is still present on work surfaces after cleaning procedures are concluded.[12,13,14,15]
The traditional approach to workers’ health protection from exposure to cytotoxic drugs was pioneered in the 1970s and 1980s, when special guidelines and protective measures were introduced; e.g. the Canadian Society of Hospital Pharmacists issued the very first guideline for the handling of cytotoxic drugs in 1981.[16] In the following decades, numerous guidelines were published in several countries.[17,18,19]
In this paper, we investigated the occupational protection status of Shiraz University of Medical Sciences hospitals nursing staff when handling cytotoxic drugs and range of skin and mucosal contamination with cytotoxic drugs, expecting to provide some clues for improving occupational protection ability and reducing the related injury in nursing staff.
SUBJECTS AND METHODS
This study was designed as an analytic descriptive survey. The research population was comprised all nurses who work in oncology units of all three hospitals and four clinics in Fars province that is the most important centers for chemotherapy, in the South of Iran. All oncology wards had a population of 130 nurses including 90 qualified nurses (participating in all preparation, administration, and disposal of cytotoxic drugs process) for participation. Eighty-six nurses were willing to participate in this study. No sampling method was used. A questionnaire and checklist was used for data collection. The questionnaire and checklist were provided through the review of the literature. This questionnaire contains 19 items including four closed ended questions about demographics, 12 closed-ended, and three open-ended questions to determine working conditions of nurses. Before using the questionnaire in this research, it was shown to five specialists for their opinions about its validity and ability to obtain information to answer the research questions. After recommended changes had been made, it was given to 15 oncology nurses in one hospital as a pilot test. Based on the oncology nurses’ recommendations, it was further revised before it was used in this research.
To study the nurses’ practice, the checklist was used. This checklist has been used in Hazrati et al.'s study.[20] In this study, only the protective aspects that should be practiced by staff during medication preparation, administration, and disposal were evaluated. Therefore, five experts in this field revised it and some protective remarks were added to the checklist and the none-protective remarks were eliminated. The checklist included fifty practical cases in three fields of preparing (25 cases), administrating (12 cases), and disposing of cytotoxic drugs (13 cases), all having the same value as 1. The total score was fifty. For reliability of the checklist, interobserver reliability test was used; the obtained correlation coefficient was 0.94.
For ethical considerations, they told the nurses this is an approved project. The aim of this study and the procedures were explained to them to obtain their cooperation. Written informed consent was obtained from them to ensure willingness to engage in the study. The researcher maintained anonymity and confidentiality of nurses. Nurses were allowed to choose whether to participate or not, and they had the right to withdraw from the study at any time without penalty. The questionnaire was completed by all nurses (n = 86), they filled the question forms more or less 30 min during their free times and returned them to the researcher. The high response rate may be a result of the researchers’ careful follow-up as well as the nurses’ feeling encouraged to have their voices heard about the problems they face.
To evaluate the performance of nurses, researcher went to their work place without prior notice and observed (with the checklist) their function during the preparation, administration and disposal of cytotoxic drugs. For an exact observation, the personnel's practice in two opposite shifts was observed and mean of the two observations was considered as the performance for each individual. This process lasted a month and a half. Finally data obtained by the investigators were transferred to the computer. To statistically analysis of the data, SPSS software (version 18, SPSS Inc., Chicago, IL, USA) was applied. Percentage calculations and the independent samples t-test were used to see the general distribution and analysis of data. Percentage calculations and the independent samples t-test were used to see the general distribution and analysis of data.
RESULTS
In the examination of the participated oncology nurses’ individual characteristics, it was determined that their mean age was 30.52 ± 6.50 years, Most of them were female (98.8%), all of them had a bachelor's degree in nursing, More than half of them (53.5%) had work experience in oncology units between 1 and 5 years.
All of the oncology nurses took 30 days of annual leave. There were no clear guidelines for safe handling of cytotoxic drugs during pregnancy and lactation. Just in pregnancy, they did not participate in preparation of cytotoxic drugs but they administered and disposed these drugs. There was no change than before in their work conditions in breast-feeding.
About the percentage of skin or mucosal exposures to cytotoxic drugs, majority of nurses (65.1%) have been exposed. Minimum number of exposure was 1 time and maximum was 20 times. The maximum exposure range (30.2%) was between 1 and 4 times.
In this study, 66.27% of the nurses worked on inpatient oncology wards and 33.73% in outpatient treatment units. In the participating hospitals, all of the nurses prepared cytotoxic drugs by themselves.
Almost all of the nurses (91.7%) stated that before working in an oncology unit, they did not receive any education about methods of protection; however, eight nurses (9.3%) stated that they had taken a short course about of it. They stated these teachings are not enough and all nurses desired to learn about safety standards with cytotoxic agents. Favorite nurse's training methods were workshop (n = 59, 68.6%), lecture (n = 9, 10.5%), electronic learning (n = 8, 9.3%), module (n = 7, 8.1%), and informal learning in workplace (3, 3.5%), respectively.
Although the majority (69.23%) of the nurses who worked in oncology units and who administered chemotherapy did not receive, higher salary than nurses did working in other units did. All of them stated that they were not given any extra specific payment for their unit.
When nurses were accidentally contaminated with cytotoxic drugs during preparation they frequently did nothing other than normal cleaning, took care to wash off the drug from the area contaminated. In addition, when the environment where cytotoxic drugs were prepared was contaminated, they used similar procedures as stated above of doing nothing different and normal cleaning and there was no emergency spills kits to use. Disposal of wastes was done together with other medical waste.
Findings showed the mean practice score was 21.1 ± 3.76. Minimum score was 12.5 and maximum was 31. The independent samples t-test showed the outpatient nurses were weaker in practice (17.2 ± 2.52) in comparison with university hospitals (23.35 ± 3.02, P < 0.001).
The findings showed that for preparation of cytotoxic drugs biologic safety cabinet Class I was used in all hospitals and clinics. Fifteen nurses (17.44%) prepared drug in open space. In 52.9% of canters, biologic safety cabinet was in separate room, in other canters was found in the patient rooms.
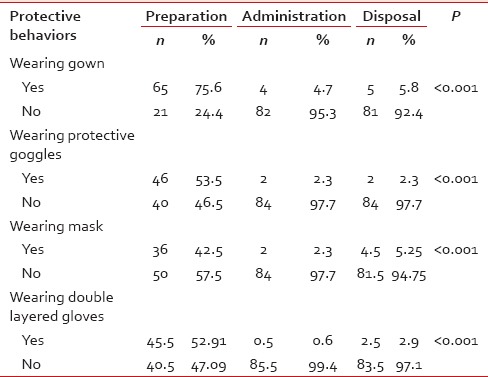
The mean of two observations of nurse's practice in two opposite shifts about the use of personal protective equipment such as gown, mask, goggles, and gloves in preparation, administration and disposal of cytotoxic drugs were as follows [Table 1].
Table 1
The status of protective behaviors in preparing, administration and disposal of cytotoxic drugs (n=86)
DISCUSSION
In this research, the occupational protection status of clinical nursing staff exposed to cytotoxic drugs in chemotherapy center of Shiraz University of Medical Sciences was examined. Generally, it was determined that the working conditions of oncology nurses are more negative than nurses working in other areas.
When the length of employment of nurses working in oncology units was examined, it was determined that in general, nurses started to work in oncology units after they had 3 and 4 years of experience (53.5%). Almost 20.9% (n = 18) of the oncology nurses began their work in oncology ward without having work experience in other wards. This finding is consistent with other research such as Karadag et al. in which the mean job experience of the nurses was 8.6 years and experience in oncology units was 4.9 years.[21]
The research was conducted by the European Oncology Nurses Society (EONS) to determine the status of oncology nurses in Europe, 20 out of 22 countries responded. They reported that the nurses’ mean age was 43, they had 21 years of professional experience, the level of education in 13 countries was diploma and academic education in seven countries.[22]
Cytotoxic drugs are prepared by nurses themselves. The reason for this may be that these hospitals do not have a clinical pharmacist on staff. In addition according to national legislation, drugs are prepared by nurses and because there is no specific legislation about cytotoxic drugs, nurses are under obligation to prepare them. In research conducted by Baykal et al. with 171 oncology nurses throughout Turkey similar results were found as the majority of the nurses (78.9%) prepared cytotoxic drugs by themselves and only 13.5% stated that the drugs were prepared in the pharmacy.[23] But Verity et al. study showed that in English, the preparation of drugs by pharmacists was performed.[24]
All of the oncology nurses took 30 days of annual leave. The research was conducted by the EONS to determine the status of oncology nurses in Europe determined they took 2–6 weeks of annual leave.[22]
In this research, similar to results from the studies by Baykal et al. and Yanqin et al., lack of continuing education was a problem.[23,25] In this study, the nurses who prepared and administered cytotoxic drugs had not been given education on safety standards with cytotoxic drugs (90.7%). This is a statistically significant deficiency for protecting the health of nurses. However, it is an International Labor Organization recommendation that employees need to have knowledge and abilities appropriate for their working area and it is clearly necessary for nurses to be better prepared through the education.[26] In study of Yanqin et al. in China, with the aim of protecting nurses (n = 168) during the exposure to cytotoxic drugs showed that of the 108 (64.8%) of nurses had received training about job security. Only 50 (30.3%) of them had received special training in preparation of these drugs.[25]
In terms of performance, almost half of the nurses during medication preparation used basic protective equipment including gowns, masks, goggles, and gloves. Use of this equipment during the administration and disposal of medicines was insufficient. In the research study conducted by Yanqin et al. revealed all of nurses used mask 168 (100%), 81 (48.8%) wore double gloves and 6 (3.6%) used gowns and goggles, when prepared these drugs.[25]
In the other research conducted by Baykal et al., the nurses were asked what kind of protective measures they used, the majority of them (94.7%) stated that they wore gloves, followed by masks (89.5%), gowns (52.0%), and goggles (18.7%). Cytotoxic drugs were prepared by 40.4% of the nurses under a hood (biological safety cabin), by 37.4% in the nurses’ office, and by 15.8% in the room which is also used for tea breaks, meals, and for other purposes.[23]
In this study, it was found that the majority of oncology nurses (65.1%) had skin or mucous membrane exposure while handling cytotoxic drugs. The absorption of these drugs is likely to be higher than this value. Because inhalation is one of the important absorbable forms of these drugs, was not considered, because nurses did not feel it. On the other hand, studies from several countries have demonstrated surface contamination of biological safety cabinets, countertops, cabinets, and floors within the drug preparation area.[13,27,28] However, this study was determined when accidental spills occur during the preparation of cytotoxic drugs and the environment or the person becomes contaminated that no special cleaning was done by the majority of the nurses, they just rinsed off as they would for normal cleaning. In the studies by Valanis et al. and Baykal et al., most nurses stated that they put on gloves to clean spills. They did not use appropriate methods of cleaning areas that were contaminated by cytotoxic drugs and did not adequately protect themselves against contamination.[23,29] However, various studies, the positive role of protective equipment (gloves, gowns, masks and eye protection) have been shown to reduce occupational exposure to these drugs.[8,9]
CONCLUSION AND RECOMMENDATION
In summary, cytotoxic drugs have been widely used clinically, the rules of occupational protection are still under improvement in Iran. In addition, nursing staff exposed to anti-tumor drugs do not generally attach enough importance to self-protection. To raise the self-protection consciousness and ability of nursing staff exposed to anti-tumor drugs, hospitals should build a perfect monitoring system, set standard training programs, and introduce protective facilities, so that the hazards could be limited to the least.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors wish to express their gratitude to all health experts who collaborated in data collection in the selected centers.


 PDF
PDF  Views
Views  Share
Share

