Pulmonary Oncology—Scope of the Pulmonologist
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2022; 43(01): 029-033
DOI: DOI: 10.1055/s-0042-1742653
Abstract
The International Agency for Research on Cancer GLOBOCAN project has predicted that India's cancer burden will nearly double in the next 20 years, from slightly more than a million new cases in 2012 to more than 1·7 million by 2035. In India, chronic respiratory diseases have emerged as a leading health care burden with chronic obstructive pulmonary disease (COPD) being the second leading cause of deaths and disability-adjusted life years. Patients with COPD are 6.35 times more likely to develop lung cancer. The deadly dual epidemic of “chronic respiratory diseases and cancer” warrants not only prevention but also creating an increased awareness among oncologists as well as pulmonologists to enable early diagnosis and treatment. It would be incorrect to assume that the scope of a pulmonologist in oncology is just diagnosing and treating lung cancer or prescribing chemotherapy for lung cancer. There is a larger world full of opportunities beyond that, and we look at the pulmonologist as a member of a multidisciplinary oncology team working together with the surgical, radiation, and medical oncologist and ancillary specialties to address all the issues highlighted earlier that are faced in oncology practice. The current exposure to pulmonary oncology and related complications during postgraduate training for respiratory medicine in India is limited. It is necessary not only to educate the pulmonologist on their role in an oncology setup but also to increase the awareness across all oncology specialties regarding the pulmonologist's contribution in management of the cancer patient. In this review, written based on our experience gained in our pulmonology service in our tertiary oncology center, we have tried to portray the wide role of the pulmonologist in oncology. We have realized that what is lacking is the basic awareness regarding the above potential, both among pulmonologists and oncologists. Our mission is to take this message across specialists in India, highlighting how we can work synergistically in the fight against cancer.
Publication History
Article published online:
21 February 2022
© 2022. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
The International Agency for Research on Cancer GLOBOCAN project has predicted that India's cancer burden will nearly double in the next 20 years, from slightly more than a million new cases in 2012 to more than 1·7 million by 2035. In India, chronic respiratory diseases have emerged as a leading health care burden with chronic obstructive pulmonary disease (COPD) being the second leading cause of deaths and disability-adjusted life years. Patients with COPD are 6.35 times more likely to develop lung cancer. The deadly dual epidemic of “chronic respiratory diseases and cancer” warrants not only prevention but also creating an increased awareness among oncologists as well as pulmonologists to enable early diagnosis and treatment. It would be incorrect to assume that the scope of a pulmonologist in oncology is just diagnosing and treating lung cancer or prescribing chemotherapy for lung cancer. There is a larger world full of opportunities beyond that, and we look at the pulmonologist as a member of a multidisciplinary oncology team working together with the surgical, radiation, and medical oncologist and ancillary specialties to address all the issues highlighted earlier that are faced in oncology practice. The current exposure to pulmonary oncology and related complications during postgraduate training for respiratory medicine in India is limited. It is necessary not only to educate the pulmonologist on their role in an oncology setup but also to increase the awareness across all oncology specialties regarding the pulmonologist's contribution in management of the cancer patient. In this review, written based on our experience gained in our pulmonology service in our tertiary oncology center, we have tried to portray the wide role of the pulmonologist in oncology. We have realized that what is lacking is the basic awareness regarding the above potential, both among pulmonologists and oncologists. Our mission is to take this message across specialists in India, highlighting how we can work synergistically in the fight against cancer.
GLOBOCAN 2020 estimates that the global cancer burden has risen to 19.3 million cases and 10 million cancer deaths in 2020. The global burden of disease is expected to be 28.4 million cases in 2040, around 47%-rise from 2020. With an estimated 2.2 million new lung cancer cases and 1.8 million deaths, lung cancer is the second most frequently diagnosed cancer and the leading cause of cancer death in 2020. These cases represent ∼1 in 10 (11.4%) cancers diagnosed and 1 in 5 (18.0%) deaths.[1] In our country, chronic respiratory diseases have emerged as a leading health care burden with chronic obstructive pulmonary disease (COPD) being the second leading cause of deaths and disability adjusted life years.[2] Patients with COPD are 6.35 times more likely to develop lung cancer.[3] The deadly dual epidemic of “chronic respiratory diseases and cancer” not only warrants prevention but also is essential for creating an increased awareness among oncologists as well as pulmonologists to enable early diagnosis and treatment.
The low ratio of oncologists to cancer patients in India has been emphasized with the estimate of around one oncologist for 2,000 cancer patients.[4] A study by Mathew estimated that in India, there are ∼1,500 clinical oncologists and the ratio of new cancer cases per clinical oncologist is 677.[5] The current exposure to pulmonary oncology and related complications during postgraduate training for respiratory medicine in India is limited. Many of the dedicated oncology institutions and regional cancer centers in India do not have inbuilt specialist pulmonology services to address multiple respiratory issues in these patients. Over the past decade, we have been able to initiate and develop specialist pulmonary medicine services at our tertiary oncology center. Our consultations have exponentially increased from single digits a decade ago to more than 10,000 a year. Thus, it is necessary not only to educate the pulmonologist on their role in an oncology setup but also to increase the awareness across all oncology specialties regarding the pulmonologist's contribution in management of the cancer patient ([Fig. 1]).
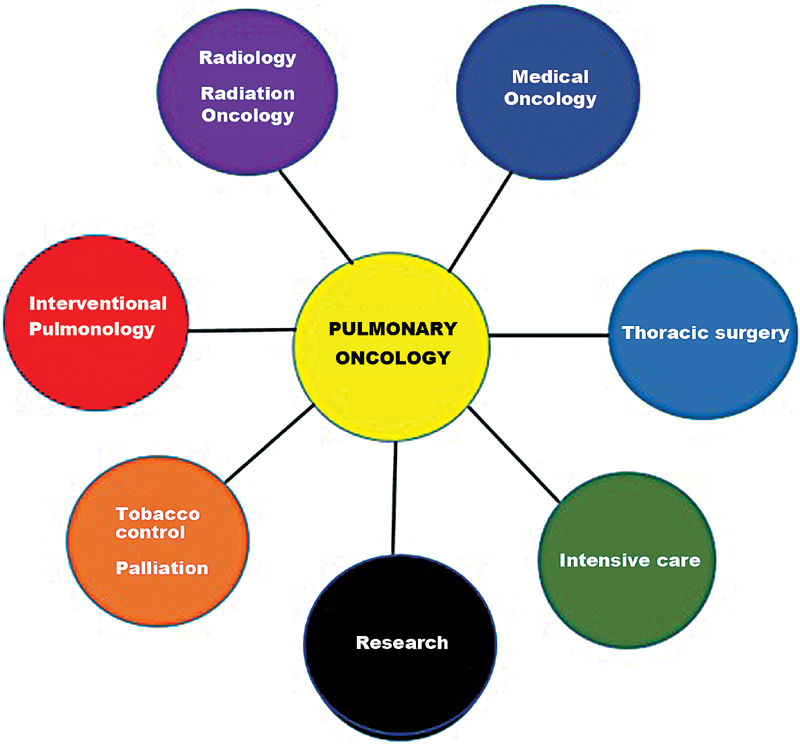
| Fig. 1Scope of the pulmonologist in pulmonary oncology.
To address these issues, we have initiated, since 2019, a unique training program for the pulmonologist, a 2-year “Fellowship in Pulmonary Oncology” at our tertiary cancer center. It is the first such curriculum-driven and university-approved training fellowship in oncology-related pulmonology in India. This program is a multidisciplinary training initiative of the “Thoracic Oncology Disease Management Group” of our center, and we have more than 50 applicants vying for a single post. This fellowship strives to give a unique training experience to the postgraduate pulmonologist trainee as evidenced from the spectrum of clinical challenges mentioned later.
From our experience gained over the past many years working as a multidisciplinary team member of our oncology multispecialty colleagues, we see the role of a pulmonologist in oncology in the following areas:
-
1. Evaluating patient's respiratory symptoms or radiological abnormalities and cancer mimics: Patients diagnosed with cancer are often referred to our institution from all over the country, based on imaging or cytology reports. But after our evaluation, patients often turn out to have cancer mimicking conditions such as allergic bronchopulmonary aspergillosis (ABPA), tuberculosis (TB), chronic lung abscess, cryptogenic organizing pneumonia, sarcoid, antinuclear cytoplasmic antibody-associated vasculitis, pulmonary embolism or central airway disease, aspergilloma or fungal infections, etc. Undiagnosed mediastinal lymphadenopathy in a TB-endemic country like ours often poses a diagnostic dilemma. It requires further evaluation with endobronchial ultrasound (EBUS) or image-guided biopsy. We have been seeing a large number of such patients, and it is a worrisome trend as lack of awareness and access to specialized centers delays diagnosis, management, and overall prognosis of treatable diseases.
-
2. Pulmonary comorbidities in cancer patients: In our practice, we often see coexistent TB, asthma, COPD, idiopathic pulmonary fibrosis (IPF), hypersensitivity pneumonitis, ABPA, connective tissue disease, etc. which might not have been detected until the time of cancer diagnosis. The presence of comorbidities affects the decisions related to cancer treatment, quality of life, and cancer prognosis with 1.1- to 5.8-fold higher risk of mortality.[6] Hence, recognition and management of these comorbidities are as important as management of the cancer and will impact outcomes.
Data suggest COPD prevalence of around 40 to 80%-in patients with lung cancer.[7] [8] [9] Patients with poor lung functions are unable to undergo potentially curative surgery. Smoking is a risk factor for both interstitial lung disease (ILD) and lung cancer. IPF is associated with a high incidence of lung cancer (relative risk of 7–14).[10] [11] [12] [13] Incidence of ILD is ∼2.2 to 3.9%-in patients with non-small cell lung cancer.[14] [15] [16] [17] Preexisting ILD is also a risk factor for development of drug-induced ILD, radiation pneumonitis, as well as an increased risk of acute exacerbation of ILD during cancer treatment.[18] [19] [20] [21] [22] [23]
-
3. Diagnosis and staging of lung cancer: Knowledge of the diagnosis and staging of lung cancer are extremely important for the pulmonologist as they are the first point of contact for most lung cancer patients. This would involve being well versed with the TNM classification as well as role of ancillary investigations such as positron emission tomography–computed tomography and magnetic resonance imaging of the brain followed by their cautious and logical interpretation. Mediastinal staging is essential prior to making therapy decisions.
Here too, the pulmonologist is playing a wider role with EBUS-guided transbronchial needle aspiration and transesophageal bronchoscopic ultrasound-guided fine needle aspiration. Most postgraduate pulmonology training programs in India provide limited exposure and experience in oncology-related problems.
Formal and accredited training for prescription of chemotherapy for lung cancer is lacking in present pulmonology postgraduate programs of our country, except for a few specialized centers. Therefore, at present, chemotherapy for lung cancer is best left to the medical oncologist. However, in future, specialized certified medical oncology training at regional oncology centers might give sufficient exposure to mandate the pulmonologist prescribing chemotherapy. This initiative will bridge the gap between patient and limited service accessibility. In our experience at our tertiary oncology center, there is a much larger role for the pulmonologist in oncology as part of a multidisciplinary team rather than limiting ourselves to a specialized niche of managing lung cancer with chemotherapy.
-
4. Preoperative pulmonary evaluation for major lung resection surgery: Preoperative evaluation for lung resection includes calculation of predicted postoperative lung functions, functional exercise testing (6-minute walk test, shuttle walk tests, and cardiopulmonary exercise test). Prehabilitation, that is, pulmonary rehabilitation pericancer therapy across the spectrum of surgery, chemotherapy, radiotherapy, and palliative care is an extremely important task of the pulmonologist and the physiotherapist. But it is seldom given its due importance or place in cancer therapy by oncologists due to lack of awareness of the same.[24] Preoperative optimization of lung function with appropriate medications and a pulmonary rehabilitation plan prior to cancer therapy improve functional capacity and impact therapy decisions and outcomes. Rehabilitation is also done for the cancer patient undergoing chemotherapy or radiotherapy. The preoperative respiratory evaluation is not limited to thoracic surgeries but has huge impact on outcomes of upper abdominal surgeries such as Whipple's surgery or major plastic head–neck reconstructive surgeries. The goal would be to ensure best outcomes so that even borderline performance status, patient's treatment, and health can be optimized and rendered fit for surgery wherever indicated.
-
5. Respiratory failure in critically ill cancer patients in the intensive care unit (ICU): Inputs from the pulmonologist to the intensivist go a long way in managing cancer patients in the ICU. They may present with respiratory failure or pulmonary lesions or develop pleural complications such as empyema and postoperative or postchemotherapy bronchopleural fistula.
-
6. Diagnosis and management of pulmonary complications of cancer therapies: The early recognition of chemotherapy-related lung toxicity especially with newer chemotherapy medications and biologicals, as well as recognition of late-onset toxicity related to radiotherapy is essential. Here, an early interaction between the oncologist and pulmonologist is crucial for definitive management. This would also include management of complications such as acute exacerbation of ILD, infections in immunocompromised host, respiratory failure, acute respiratory distress syndrome, and empyema.
-
7. Pulmonary lesions in immunosuppressed host: Recognition, diagnosis, management, and differentiation between infective and noninfective causes of lung infiltrates in the immune-suppressed patient with cancer therapy are an important area where a pulmonologist's opinion is frequently sought. TB including drug-resistant TB is a major problem, apart from the other causes of pulmonary lesions such as invasive fungal or viral infections. TB also delays the initiation of cancer treatment.[25] [26] [27] [28]
-
8. Tobacco cessation, management of pain, palliative care, and end of life issues: This is an area which needs to be stressed upon more as preventive activities help in reducing cancer burden, and the pulmonologist should take the lead. Lung cancer screening as part of public health program is a debatable issue in the Indian scenario.
With the convergence of the role of palliative care in cancer and increasing awareness of its role in advanced chronic respiratory disease, it is imperative that the pulmonologist be well versed with this field. As the patient's access to these services and opioid medications are limited, and with respiratory symptoms being the common event in advanced cancer, these patients frequently present to the pulmonologist. Palliative care itself will be a niche area for the pulmonologist in the future.
-
9. Multidisciplinary tumor boards: Tumor boards facilitate specialists from all cancer-related disciplines to interact and give case-based inputs thus enhancing patient care. The Tata Memorial Centre, a tertiary oncology center based in Mumbai, India has been in the forefront to set up the National Cancer Grid (NCG). The NCG is an initiative of government of India funded through the Department of Atomic Energy. It currently has 183 cancer centers, research institutes, patient groups, charitable organizations, and professional societies, which treat more than 700,000 new patients with cancer annually, ∼60%-of all India's cancer patients. All institutions dealing with oncology cases are encouraged by the NCG to join the network, and their oncology teams interact with each other via the telemedicine platform thus ensuring evidence-based care to the patient.
-
10. Interventional pulmonology (IP) as an indispensable need in thoracic oncology: These techniques have revolutionized pulmonary oncology in their use, right from diagnosis to palliative management of central airways obstruction and indwelling pleural catheters. The IP armamentarium consists of (and is not limited to) the following procedures ([Table 1]).
|
Diagnostic |
Therapeutic |
|---|---|
|
Flexible bronchoscopy: 1. Bronchoalveolar lavage (BAL), 2. Endobronchial biopsy (EBB), 3. Transbronchial lung biopsy (TBLB) 4. Advance bronchoscopic imaging: Narrow band imaging/Confocal microendoscopy/Auto-fluroscence bronchoscopy |
Central airway disease (tumors, strictures): 1. Airway strictures: Balloon dilatation 2. Tumor debulking: Rigid bronchoscopy coring/Micro-debridement/Argon plasma coagulation (APC)/Laser (Nd:YAG, CO2),/Electrocautery/Cryotherapy debulking 3. Airway Stent 4. Photodynamic therapy (PDT) 5. HDR- brachytherapy |
|
Mediastinal lymph node and masses: 1. Conventional transbronchial needle aspiration (C-TBNA) 2. Endobronchial ultrasound guided transbronchial needle aspiration (EBUS-TBNA) |
Fiducial marker placement: 1. Fiducial marker placement for localization for surgical resection 2. Fiducial marker placement to assist stereotactic body radiation therapy (SBRT) for inoperable patients with resectable stage I lung CA |
|
Peripheral pulmonary lesions/nodules: 1. Radial endobronchial ultrasound guided TBLB (R-EBUS-TBLB) 2. Virtual and Electromagnetic navigation bronchoscopy |
Pleural disease in oncology: 1. Medical Pleuroscopy, Thoracoscopic pleurodesis 2. Indwelling pleural catheters |
|
Diffuse parenchymal disease and masses: Cryo-lung biopsy |
Bronchoscopic management of peripheral lung lesions: Radiofrequency ablation |
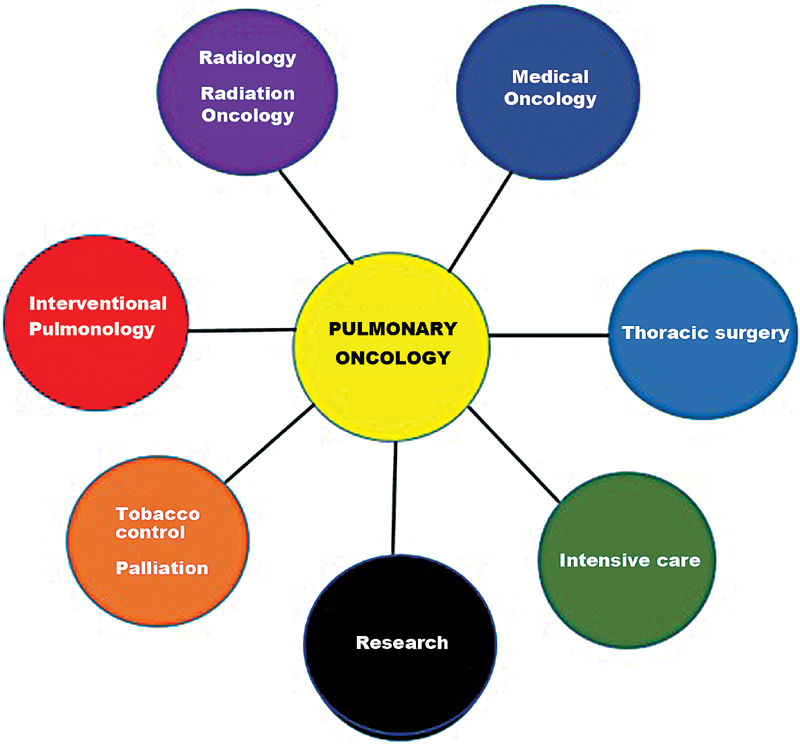
| Fig. 1Scope of the pulmonologist in pulmonary oncology.
References
- Sung H, Ferlay J, Siegel RL. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021; 71 (03) 209-249
- India State-Level Disease Burden Initiative CRD Collaborators. The burden of chronic respiratory diseases and their heterogeneity across the states of India: the Global Burden of Disease Study 1990-2016. Lancet Glob Health 2018; 6 (12) e1363-e1374
- India State-Level Disease Burden Initiative Cancer Collaborators. The burden of cancers and their variations across the states of India: the Global Burden of Disease Study 1990-2016. [published correction appears in Lancet Oncol 2018 Oct 3;] Lancet Oncol 2018; 19 (10) 1289-1306
- Noronha V, Tsomo U, Jamshed A. et al. A fresh look at oncology facts on south central Asia and SAARC countries. South Asian J Cancer 2012; 1 (01) 1-4
- Mathew A. Global survey of clinical oncology workforce. J Glob Oncol 2018; 4: 1-12
- Søgaard M, Thomsen RW, Bossen KS, Sørensen HT, Nørgaard M. The impact of comorbidity on cancer survival: a review. Clin Epidemiol 2013; 5 (Suppl. 01) 3-29
- Gottlieb M, Marsaa K, Godtfredsen NS, Mellemgaard A. Prevalence and management of pulmonary comorbidity in patients with lung and head and neck cancer. Acta Oncol 2015; 54 (05) 767-771
- Mohan A, Mohan C, Pathak AK, Pandey RM, Guleria R. Impact of chronic obstructive pulmonary disease on respiratory status and quality of life in newly diagnosed patients with lung cancer. Respirology 2007; 12 (02) 240-247
- Brenner DR, McLaughlin JR, Hung RJ. Previous lung diseases and lung cancer risk: a systematic review and meta-analysis. PLoS One 2011; 6 (03) e17479
- Le Jeune I, Gribbin J, West J, Smith C, Cullinan P, Hubbard R. The incidence of cancer in patients with idiopathic pulmonary fibrosis and sarcoidosis in the UK. Respir Med 2007; 101 (12) 2534-2540
- Hubbard R, Venn A, Lewis S, Britton J. Lung cancer and cryptogenic fibrosing alveolitis. A population-based cohort study. Am J Respir Crit Care Med 2000; 161 (01) 5-8
- Harris JM, Johnston ID, Rudd R, Taylor AJ, Cullinan P. Cryptogenic fibrosing alveolitis and lung cancer: the BTS study. Thorax 2010; 65 (01) 70-76
- Turner-Warwick M, Lebowitz M, Burrows B, Johnson A. Cryptogenic fibrosing alveolitis and lung cancer. Thorax 1980; 35 (07) 496-499
- Chiyo M, Sekine Y, Iwata T. et al. Impact of interstitial lung disease on surgical morbidity and mortality for lung cancer: analyses of short-term and long-term outcomes. J Thorac Cardiovasc Surg 2003; 126 (04) 1141-1146
- Miyazaki K, Satoh H, Kurishima K. et al. Impact of interstitial lung disease on survival for patients with non-small cell lung cancer. Anticancer Res 2009; 29 (07) 2671-2674
- Kumar P, Goldstraw P, Yamada K. et al. Pulmonary fibrosis and lung cancer: risk and benefit analysis of pulmonary resection. J Thorac Cardiovasc Surg 2003; 125 (06) 1321-1327
- Park J, Kim DS, Shim TS. et al. Lung cancer in patients with idiopathic pulmonary fibrosis. Eur Respir J 2001; 17 (06) 1216-1219
- Chida M, Kobayashi S, Karube Y. et al. Incidence of acute exacerbation of interstitial pneumonia in operated lung cancer: institutional report and review. Ann Thorac Cardiovasc Surg 2012; 18 (04) 314-317
- Chida M, Ono S, Hoshikawa Y, Kondo T. Subclinical idiopathic pulmonary fibrosis is also a risk factor of postoperative acute respiratory distress syndrome following thoracic surgery. Eur J Cardiothorac Surg 2008; 34 (04) 878-881
- Sato T, Teramukai S, Kondo H. et al; Japanese Association for Chest Surgery. Impact and predictors of acute exacerbation of interstitial lung diseases after pulmonary resection for lung cancer. J Thorac Cardiovasc Surg 2014; 147 (05) 1604-1611.e3
- Fujimoto T, Okazaki T, Matsukura T. et al. Operation for lung cancer in patients with idiopathic pulmonary fibrosis: surgical contraindication?. Ann Thorac Surg 2003; 76 (05) 1674-1678 , discussion 1679
- Voltolini L, Bongiolatti S, Luzzi L. et al. Impact of interstitial lung disease on short-term and long-term survival of patients undergoing surgery for non-small-cell lung cancer: analysis of risk factors. Eur J Cardiothorac Surg 2013; 43 (01) e17-e23
- ;Watanabe A, Higami T, Ohori S, Koyanagi T, Nakashima S, Mawatari T. Is lung cancer resection indicated in patients with idiopathic pulmonary fibrosis?. J Thorac Cardiovasc Surg 2008; 136 (05) 1357-1363 , 1363.e1–1363.e2
- Macmillan Cancer Support, Royal College of Anaesthetists. National Institute of Health Research - Prehabilitation for people with Cancer
- Simonsen DF, Farkas DK, Horsburgh CR, Thomsen RW, Sørensen HT. Increased risk of active tuberculosis after cancer diagnosis. J Infect 2017; 74 (06) 590-598
- Engels EA, Shen M, Chapman RS. et al. Tuberculosis and subsequent risk of lung cancer in Xuanwei, China. Int J Cancer 2009; 124 (05) 1183-1187
- Dobler CC, Cheung K, Nguyen J, Martin A. Risk of tuberculosis in patients with solid cancers and haematological malignancies: a systematic review and meta-analysis. Eur Respir J 2017; 50 (02) 1700157
- Wu CY, Hu HY, Pu CY. et al. Aerodigestive tract, lung and haematological cancers are risk factors for tuberculosis: an 8-year population-based study. Int J Tuberc Lung Dis 2011; 15 (01) 125-130


 PDF
PDF  Views
Views  Share
Share

