Resistant metastatic penile carcinoma and response to biochemotherapy with paclitaxel and epidermal growth factor receptor monoclonal antibody, nimotuzumab
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2013; 34(01): 24-27
DOI: DOI: 10.4103/0971-5851.113411
Abstract
Carcinoma penis is one of the common malignancies in developing world especially among rural population. Multimodality treatment with surgery, radiation and chemotherapy for advanced penile carcinoma with groin nodal metastasis is crucial to optimise the outcome. Cisplatin, fluorouracil, methotrexate, vinorelbine, bleomycin and paclitaxel are the common chemotherapeutic agents used along with local therapy. Paucity of data to show superiority of one chemotherapeutic regime over another and only modest response to any combination chemotherapy. Progression of disease after surgery, radiation and chemotherapy is associated with poor outcome and quality of life. Nimotuzumab, Anti EGFR monoclonal antibody, along with paclitaxel in our case of resistant metastatic penile carcinoma has shown good symptomatic palliation and clinical response.
Publication History
Article published online:
20 July 2021
© 2013. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Carcinoma penis is one of the common malignancies in developing world especially among rural population. Multimodality treatment with surgery, radiation and chemotherapy for advanced penile carcinoma with groin nodal metastasis is crucial to optimise the outcome. Cisplatin, fluorouracil, methotrexate, vinorelbine, bleomycin and paclitaxel are the common chemotherapeutic agents used along with local therapy. Paucity of data to show superiority of one chemotherapeutic regime over another and only modest response to any combination chemotherapy. Progression of disease after surgery, radiation and chemotherapy is associated with poor outcome and quality of life. Nimotuzumab, Anti EGFR monoclonal antibody, along with paclitaxel in our case of resistant metastatic penile carcinoma has shown good symptomatic palliation and clinical response.
INTRODUCTION
Carcinoma penis is one of the common malignancies in developing world especially among rural population.[1] Poor genital hygiene, promiscuity, phimosis, human papillomavirus (HPV), and tobacco consumption are the common risk factors.[2] The presence and extent of inguinal lymph node metastases are the most important prognostic factors in patients with penile cancer.[3] Local and regional recurrences are common during the first 2 years of follow-up. Cisplatin, fluorouracil, methotrexate, vinorelbine, bleomycin, and paclitaxel are the common chemotherapeutic agents used along with local therapy to improve the outcome in terms of disease control or symptomatic relief.
CASE REPORT
A 59-year-old male presented with penile ulcer since 1 month with reactive left inguinal lymphadenopathy. Wide excision of lesion with 1 cm margin was done after biopsy revealed squamous cell carcinoma. Subsequently on follow-up, he developed inguinal lymph nodal metastasis 3 months later for which he received bilateral groin radiation to a dose of 54.8 Gy/16 # with direct portal. Recurrence was seen in bilateral inguinal nodes within 3 months for which bilateral groin node dissection was done and adjuvant three cycles of paclitaxel and cisplatin were given in view of multiple groin node involvement and perinodal extension. After 6 months of follow-up, patient developed scrotal edema with multiple perineal nodules and inguinal lymphadenopathy confirmed as metastasis of squamous cell carcinoma on FNAC. In view of good performance status and paucity of alternative treatment option, second-line chemotherapy with two cycles of oxaliplatin and capecitabine were given on compassionate ground which produced no response. There was local progression and involvement of bilateral external iliac lymph nodes. Third-line chemotherapy was administered with four cycles of gemcitabine and vinorelbine. Patient again had no response to therapy. The patient still had an excellent performance status and was very desirous of continuing systemic therapy; hence, it was decided to administer biochemotherapy with nimotuzumab and paclitaxel at a dose of 200 mg and 80 mg/m2 weekly, respectively. After 12 weeks, clinically, there was reduction in scrotal edema and resolution in skin nodules. Response evaluation of PET-CT revealed no change in the status of left inguinal lymphadenopathy with persistent SUV max of 4.0; however, right-sided inguinal metastasis disappeared after biochemotherapy [Figures [Figures11 and and2].2]. Patient developed grade 3 peripheral neuropathy after 12 weeks; hence, paclitaxel was discontinued and patient is now continuing on weekly nimotuzumab and has completed 23 weeks of nimotuzumab till date.
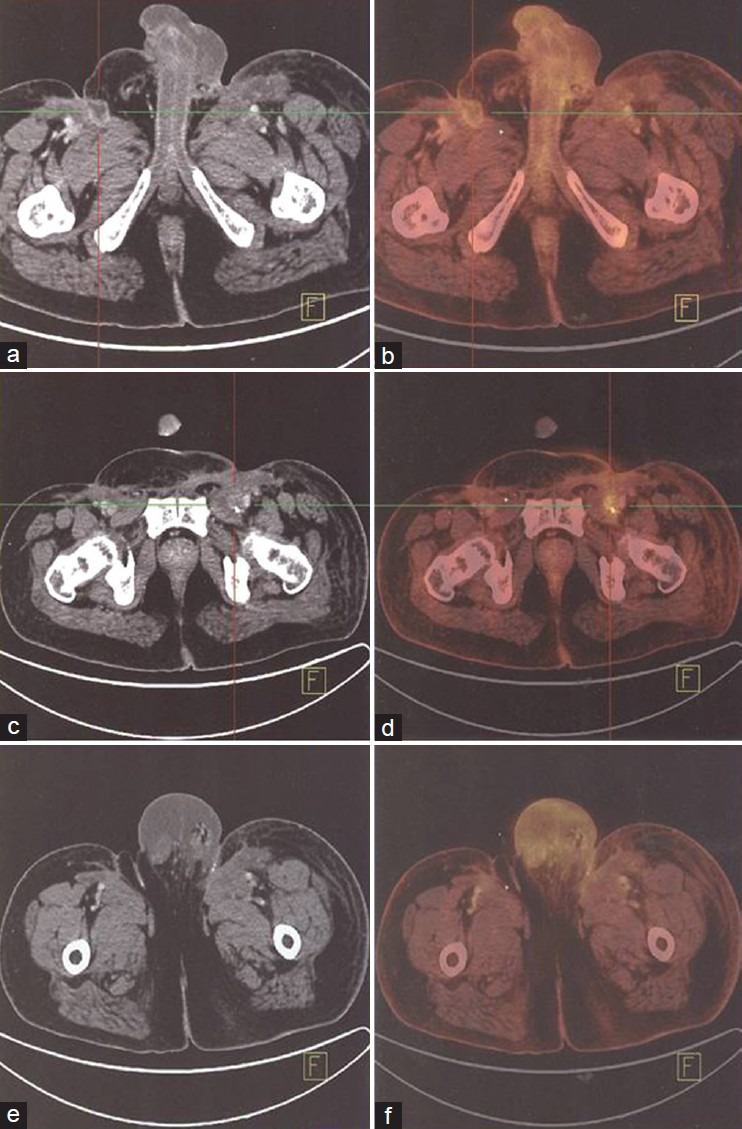
| Fig. 1 (a and b) Baseline PET-CT showing bilateral groin lymphadenopathy with scrotal edema. (c and d) Post 12 weeks resolution of right groin lymphadenopathy with persistent disease on left side. (e and f) Showing resolution of lower inguinal lymphadenopathy with persistent scrotal edema-post 12 weeks of therapy
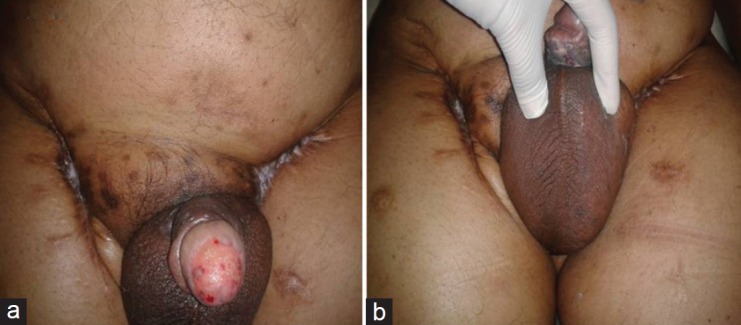
| Fig. 2 (a and b) Clinical response post 12 weeks of bio-chemotherapy with significant resolution of cutaneous nodules and scrotal edema
DISCUSSION
Carcinoma penis comprises less than 1% of all malignancies among western population with median age at diagnosis around 60 years and 30% presenting with advanced disease.[4] The incidence is as high as 10-17% in African countries while the age standardized rate in India varies from 0.8 to 1.8 per lakh population with Chennai registry having the highest incidence.[5,6] Neonatal circumcision commonly practiced in Jews has a preventive role as demonstrated by decrease in incidence of penile carcinoma among men who were circumscribed in early childhood.[5,7] Higher incidence of penile and cervical carcinoma with concordance among married couple in Hindu population but not in Muslims reiterates the significance of circumcision, HPV infection, and poor post-coital genital hygiene as risk factors for carcinogenesis.[8,9]
Early localized penile carcinoma has an excellent outcome with more than 70% long-term survival with local penile conservative approach using surgery or radiotherapy. About 30-40% of patients present with lymph node metastases in which long-term survival is just 20-30%.[3] Multimodality treatments with surgery, radiation, and chemotherapy for advanced penile carcinoma with groin nodal metastasis is crucial to optimize the outcome with minimal toxicity and morbidity. Penile squamous cell carcinoma is chemosensitive. Chemotherapeutic agents including cisplatin, 5-fluorouracil, Bleomycin, methotrexate, and vincristine have been used in various combinations to downstage the tumor and improve resectability in patients with groin node metastases. Earlier, small studies using single drugs such as cisplatin, methotrexate, and bleomycin have shown only modest response rates varying from 15% to 30% with majority of partial response and durability from 1 to 3 months.[10,11] Haas et al. in a prospective, multi-institutional Phase II study using cisplatin, bleomycin, and methotrexate demonstrated improvement in response rate upto 32% with 12% complete response with median duration of response upto 16 weeks. However, it came with significant toxicity with 11% treatment-related death and 17% life-threatening complications precluding the establishment of this combination as standard therapy.[12]
Long-term survival post-radical groin node dissection using weekly vincristine, bleomycin, and methotrexate was demonstrated by Pizzocaro et al. They also proposed the potential of curative resection in case of inoperable inguinal nodal metastasis following neoadjuvant chemotherapy.[13] Roth et al., in a small cohort of patients, demonstrated potential benefit of intra-arterial chemotherapy using methotrexate, mitomycin, and bleomycin with 75% response rates and 37% complete responses with two out of three complete responders achieving long-term control rates. Use of bleomycin as a radiosensitizer in low-grade tumors has shown equivalent results to surgery with the potential for penile conservation.[14] Combination of cisplatin and 5-FU in neoadjuvant therapy improved the response rates upto 80% with 40% complete responses.[15] Impressive results of adding taxanes to cisplatin and 5-FU (TPF) in locally advanced head and neck carcinomas with higher complete response rates and trend toward better survival inspired investigators to attempt the same in metastatic penile carcinoma.[16] Complete pathological response was demonstrated in patients completing four cycles of TPF albeit with higher toxicity and 50% of patients had complete clinical response among patients receiving at least two cycles.[17]
No large-scale prospective trials have been designed to ascertain the optimal timing and regimens of chemotherapy in carcinoma penis partly due to the rarity of the disease. No conclusive data exists to show superiority of one chemotherapeutic regimen over any other in recurrent and metastatic carcinoma with all described combinations resulting in only modest responses. Extensive literature search did not reveal any studies on second-line or beyond chemotherapy, thus limiting options for such subgroup of patients. Increased expression of epidermal growth factor receptor (EGFR) is associated with poorer outcome in advanced head and neck cancer.[18] Overstimulation of EGFR-mediated signaling can contribute to uncontrolled cell division and thus to oncogenic signaling and tumor angiogenesis and metastasis, protecting cancer cells from undergoing apoptosis. Availability of anti-EGFR therapy has shown improvement in response rates with or without chemotherapy in head and neck squamous cell carcinoma in the recurrent or metastatic second-line setting.[19] EGFR overexpression has recently been shown in penile carcinoma with 80% being strongly positive; however, there are no published studies using monoclonal antibodies or tyrosine kinase inhibitors therapeutically in the recurrent or metastatic setting.[20] Taking analogy with head and neck cancer, anti-EGFR therapy may produce similar responses in recurrent or metastatic penile carcinoma. Nimotuzumab is a humanized therapeutic monoclonal antibody against EGFR approved for tumors of epithelial origin expressing EGFR such as head and neck squamous cell carcinoma.[21] No studies using targeted therapy in recurrent or metastatic penile carcinoma has been reported so far. Our result of clinical response to biochemotherapy after progression on multiple lines of chemotherapy possibly opens a new horizon in management of recurrent or metastatic penile carcinoma. Larger prospective studies are necessary to corroborate our experience within the metastatic setting and perhaps also in the neoadjuvant and adjuvant settings.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
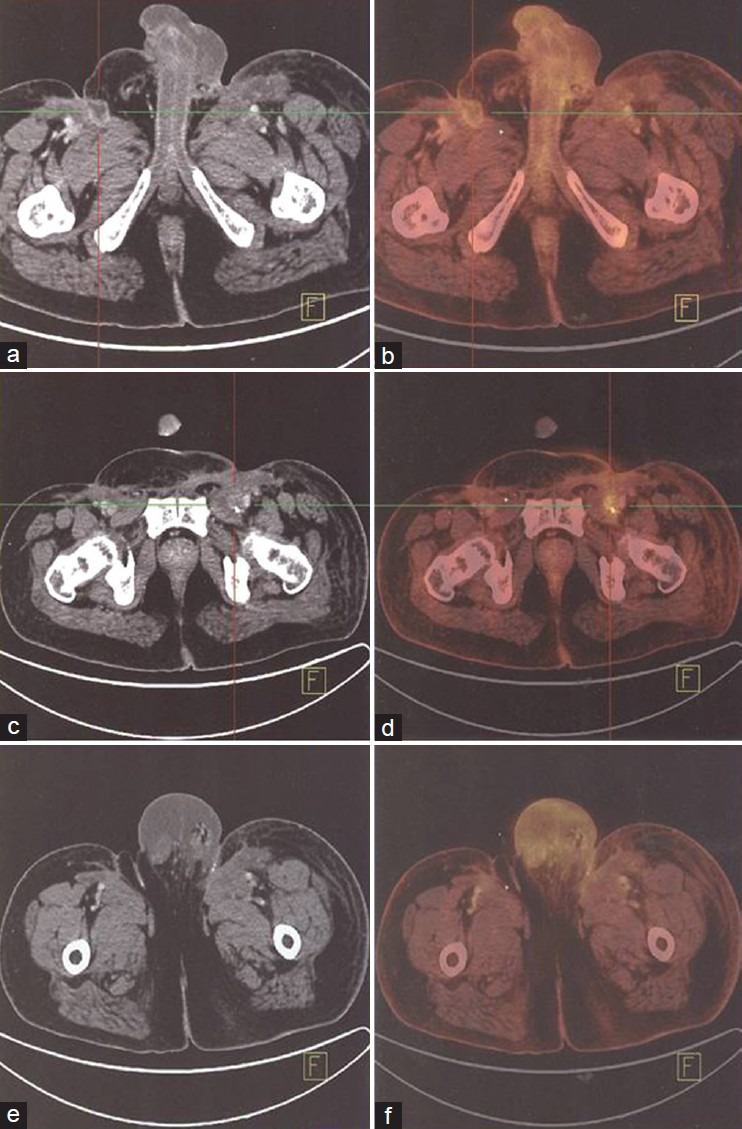
| Fig. 1 (a and b) Baseline PET-CT showing bilateral groin lymphadenopathy with scrotal edema. (c and d) Post 12 weeks resolution of right groin lymphadenopathy with persistent disease on left side. (e and f) Showing resolution of lower inguinal lymphadenopathy with persistent scrotal edema-post 12 weeks of therapy
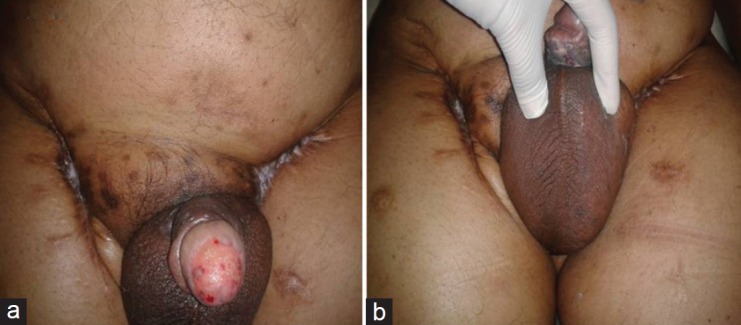
| Fig. 2 (a and b) Clinical response post 12 weeks of bio-chemotherapy with significant resolution of cutaneous nodules and scrotal edema


 PDF
PDF  Views
Views  Share
Share

