Retrospective analysis of patients with carcinoma cervix in a rural/semi-urban setting in Western India
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2016; 37(01): 25-27
DOI: DOI: 10.4103/0971-5851.177011
Abstract
Objectives: To compare the presentation of cervical cancer and the treatment modalities received by the patients at a semi-urban/rural area of Western India with that of published literature from urban centers. Materials and Methods: We conducted a retrospective analysis of patients with cervical cancer who presented at a semi-urban/rural cancer center between 2010 and 2013. A total of 141 patients with the median age of 51 years (25-81) were studied. The demographic and clinical variables included age, annual family income, profession, comorbidities, baseline hemoglobin, prior screening, clinical stage, treatment administered, and complications. The pathological variables included tumor type and grade. Results: In our study, all patients presented with vaginal bleeding. Majority of the patients (51 patients, 37.7%) had Stage 3B disease. Since majority presented at later stages (Stage 3B), chemotherapy-radiotherapy was the most common treatment modality used in our population. On histopathology, 127 patients (90%) had squamous cell carcinoma while 14 patients (10%) had adenocarcinoma. In 96 patients (68%), the tumor grade was not known while it was a high, intermediate, and low grade in 6 (4%), 18 (13%), and 21 (15%) patients, respectively. The follow-up data of our study were not adequate; hence, the long-term survival results could not be presented. Conclusion: Patients in rural India setting present at later stages which could be improved by creating awareness, improving their personal hygiene, and adequate screening.
Publication History
Article published online:
12 July 2021
© 2016. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Objectives:
To compare the presentation of cervical cancer and the treatment modalities received by the patients at a semi-urban/rural area of Western India with that of published literature from urban centers.
Materials and Methods:
We conducted a retrospective analysis of patients with cervical cancer who presented at a semi-urban/rural cancer center between 2010 and 2013. A total of 141 patients with the median age of 51 years (25-81) were studied. The demographic and clinical variables included age, annual family income, profession, comorbidities, baseline hemoglobin, prior screening, clinical stage, treatment administered, and complications. The pathological variables included tumor type and grade.
Results:
In our study, all patients presented with vaginal bleeding. Majority of the patients (51 patients, 37.7%) had Stage 3B disease. Since majority presented at later stages (Stage 3B), chemotherapy-radiotherapy was the most common treatment modality used in our population. On histopathology, 127 patients (90%) had squamous cell carcinoma while 14 patients (10%) had adenocarcinoma. In 96 patients (68%), the tumor grade was not known while it was a high, intermediate, and low grade in 6 (4%), 18 (13%), and 21 (15%) patients, respectively. The follow-up data of our study were not adequate; hence, the long-term survival results could not be presented.
Conclusion:
Patients in rural India setting present at later stages which could be improved by creating awareness, improving their personal hygiene, and adequate screening.
INTRODUCTION
One of the leading causes of death in women all over the world is cancer of the uterine cervix. It is the most common cause of cancerous deaths in females in developing countries, whereas, in rest of the world, cervical cancer is the second most common cause of death from cancer in women. Cervical cancer contributes to 15% of all cancers in females worldwide while in South-East Asia, it accounts for 20-30% of all cancers.[1]
Every year approximately 500,000 new cases of cervical cancer occur out of which 79% occur in the developing countries.[2] Cervical cancer causes approximately 288,000 deaths worldwide.[3] Unlike many other cancers, cervical cancer occurs early and strikes at the reproductive period of a woman's life. The median age of cervical cancer is 38 years (age 21-67 years), with the incidence escalating in 30-34 years and peaking at 55-65 years. In India, women above 15 years of age are at increased risk of developing cervical cancer.
In sub-Saharan Africa, the women dying from the disease are 22.5/100,000, and the newly occurring cases are 34.8/100,000 women annually. On the other hand, in North America, these figures are 2.5 and 6.6, respectively.[4] The contributing factors to these radical differences can be explained by the lack of access to effective screening and to services that facilitate early detection and treatment.
The estimated cumulative lifetime risk and death from cervical cancer in Indian women are about 2.5% and 1.4%, respectively.[5] Cervical cancer is a disease most frequently found in poverty-stricken communities and reflecting a problem of equity at both levels: Gender and regional, and this, is not only due to social and economic development inequalities but also due to the infrastructure and human resources necessary for primary care.[6]
We undertook a retrospective analysis of cervical cancer patients presenting to a cancer center in a rural/semi-urban region of Western India to evaluate the percentage of patients presenting with carcinoma cervix with their stages and the treatment modalities received and to compare this to published literature from urban centers.
MATERIALS AND METHODS
This is a retrospective analytical study that included consecutive patients with cervical cancer presenting to a semi-urban cancer center during the years 2010-2013. The Medical Records Department was requested to provide the case charts of all patients diagnosed with cervical cancer during this period. Information on demographic characteristics, presenting complaints, pathological variables, and treatments received were abstracted from the case charts into a previously designed case record form. The demographic variables included age, annual family income, profession, and co-morbidities. The clinical variables included baseline hemoglobin, prior screening, clinical stage, and treatment administered. Stage-wise treatment was administered as per standard guidelines. The pathological variables included tumor type and grade. Any ambiguity in the report was resolved through discussion with the pathologists. The data were entered and analyzed in SPSS version 19.0 (IBM SPSS Statistics for Windows, version 19.0. Armonk, NY: IBM Corp).
RESULTS
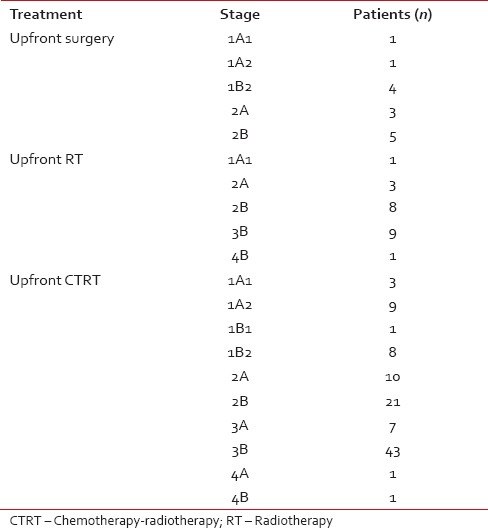
Total of 141 patients were studied [Table 1]. The median age was 50 years (range 25-81). Of these only 5% patients were working, remaining were housewives. Ninety-three percent of patients had an annual income of < Rs. 50,000/- (approximately 800 USA$). With regards to co-morbidities, 58 patients (41%) had hypertension, 51 (36%) had diabetes, 3 (2%) had a congestive cardiac failure, and 2 (1.5%) had past history of tuberculosis. Only 9 patients (6%) had a history of undergoing Pap smear examination prior to the diagnosis of cervical cancer. All patients (100%) had bleeding per vaginum as the presenting complaint. The baseline hemoglobin (Hb) distribution was Hb > 10 g/dl in 40 patients (28%), Hb 8-10 g/dl in 60 patients (43%), and Hb < 8 in 41 patients (29%). Majority of the patients (51 patients, 37.7%) had Stage 3B disease while in the remaining stage distribution was as following: 1A1: 5 patients (3.5%), 1A2: 10 patients (7%), 1B1: 1 patient (0.7%), 1B2: 13 patients (9%), 2A: 16 patients (11%), 2B: 34 patients (24%), 3A: 7 patients (5%), 4A: 1 patient (0.7%), and 4B: 2 patients (1.4%). On histopathology, 127 patients (90%) had squamous cell carcinoma while 14 patients (10%) had adenocarcinoma. In 96 patients (68%), the tumor grade was not known while it was high, intermediate, and low grade in 6 (4%), 18 (13%), and 21(15%) patients, respectively. The treatment distribution for these patients was as follows [Table 2]: 14 (10%) underwent upfront surgery (radical hysterectomy), 103 (73%) had upfront concomitant chemotherapy/radiotherapy (CT/RT), and 22 (16%) had upfront radiotherapy (RT) alone. Of the patients who underwent upfront surgery, 1 patient was of Stage 1A1 and 1A2, 4 patients of 1B2, 3 patients of 2A, and 5 patients of Stage 2B. Only one patient who underwent surgery had adenocarcinoma. Two patients were given neoadjuvant chemotherapy (NACT), of which one patient was given CTRT after NACT failure while the other was given only RT. Of the 14 patients who underwent surgery, 11 patients (79%) were given postoperative CTRT. Of the 103 upfront CTRT patients, 93 (90%) received both external RT and brachytherapy.
Table 1
Baseline characteristics
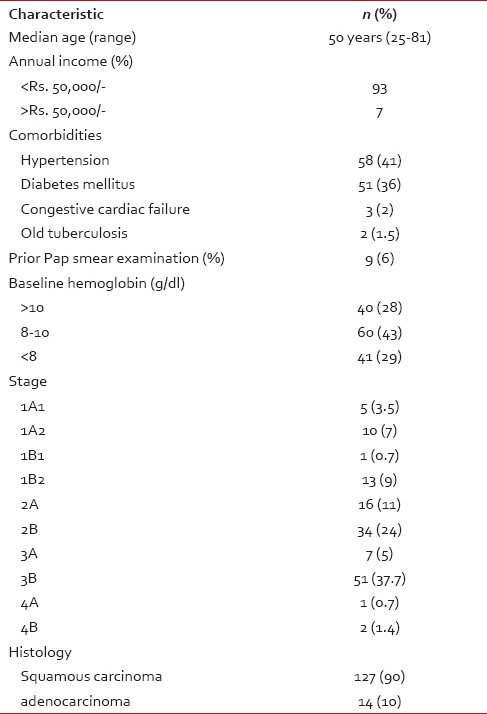
Table 2
Treatment details based on stage
DISCUSSION
This is a retrospective study of carcinoma cervix patients from rural/suburban area of western India. Screening for carcinoma cervix is still in its initial form in India, especially in the rural areas, the awareness is low as seen by the small percentage of patients who had undergone prior screening in our study. Majority of the patients were from lower socioeconomic strata. Majority of them had baseline anemia, which could have been due to bleeding and low nutrition. When compared to the western population, the median age and presenting symptom interpreted from this study was similar. The histopathology in our population was predominantly squamous carcinoma (90%) whereas, in the west, studies show that squamous carcinoma was seen only in 70%.[7] In this study, only 10% patients could undergo curative surgery as majority of them had an advanced stage on presentation, thus making CTRT as the most common treatment modality while studies from the west showed that nearly 40% could undergo surgery.[8]
The scenario of cervical cancer in India is changing, with a gradual decrease in incidence in both urban- and rural-based registries, with breast cancer presently having an upper hand.[9] Simpler screening methods such as visual inspection with acetic acid have shown to be helpful.[10] In a study done in Mumbai, where they had trained primary health care workers for screening by this method, they had showed that cervical cancer mortality reduced by 31%.[11] Such methods could be logistically feasible in the population of our study. The follow-up data of our study was not adequate. Hence, the long-term survival results could not be presented. This data emphasizes that patients in rural Indian setting present at later stages which could be improved by creating awareness in rural women, improving their personal hygiene, and help accessing adequate screening measures.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
Dr. Reshma Suraj Pawar, Kolhapur Cancer Centre, 1182/98, Mali Colony, Takala, Kolhapur, India, Dr. Varun Milind Sardar, RCSM, Government Medical College, CPR Hospital, Near Dasara Chowk, Kolhapur - 416 002, India.


 PDF
PDF  Views
Views  Share
Share

