Subcutaneous panniculitis-like T-cell lymphoma in a case of carcinoma cervix
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2013; 34(02): 104-106
DOI: DOI: 10.4103/0971-5851.116192
Abstract
Subcutaneous panniculitis-like T-cell lymphoma (SPTCL) is an uncommon extra nodal non-Hodgkin lymphoma accounting for less than 1% of all NHLs known to have an aggressive course, with no well-defined treatment protocols. A 42-year-old lady, operated five months earlier for a squamous cell carcinoma of the cervix presented with pain and induration of the lower part of the anterior abdominal wall; 3 months after completing chemotherapy and radiotherapy. FNAC done, yielded scanty material and was inconclusive. The biopsy showed features of a subcutaneous panniculitis-like T-cell lymphoma. While on chemotherapy she developed a vault recurrence and extensive intra-abdominal spread of the squamous cell carcinoma and succumbed. SPTCL is a rare entity and has been reported in renal and cardiac allograft recipients and in one case of ovarian carcinoma. Its occurrence in the setting of carcinoma cervix is unusual, hence is being reported.
Publication History
Article published online:
20 July 2021
© 2013. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/.)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Subcutaneous panniculitis-like T-cell lymphoma (SPTCL) is an uncommon extra nodal non-Hodgkin lymphoma accounting for less than 1% of all NHLs known to have an aggressive course, with no well-defined treatment protocols. A 42-year-old lady, operated five months earlier for a squamous cell carcinoma of the cervix presented with pain and induration of the lower part of the anterior abdominal wall; 3 months after completing chemotherapy and radiotherapy. FNAC done, yielded scanty material and was inconclusive. The biopsy showed features of a subcutaneous panniculitis-like T-cell lymphoma. While on chemotherapy she developed a vault recurrence and extensive intra-abdominal spread of the squamous cell carcinoma and succumbed. SPTCL is a rare entity and has been reported in renal and cardiac allograft recipients and in one case of ovarian carcinoma. Its occurrence in the setting of carcinoma cervix is unusual, hence is being reported.
INTRODUCTION
Subcutaneous panniculitis-like T-cell lymphoma (SPTCL) belongs to the category of extranodal mature T and NK-cell neoplasms.[1,2] This preferentially infiltrates the subcutaneous tissue [Figure 1] and is composed of atypical lymphoid cells of varying size with marked tumor necrosis, karyorrhexis and angioinvasion.[1,2]
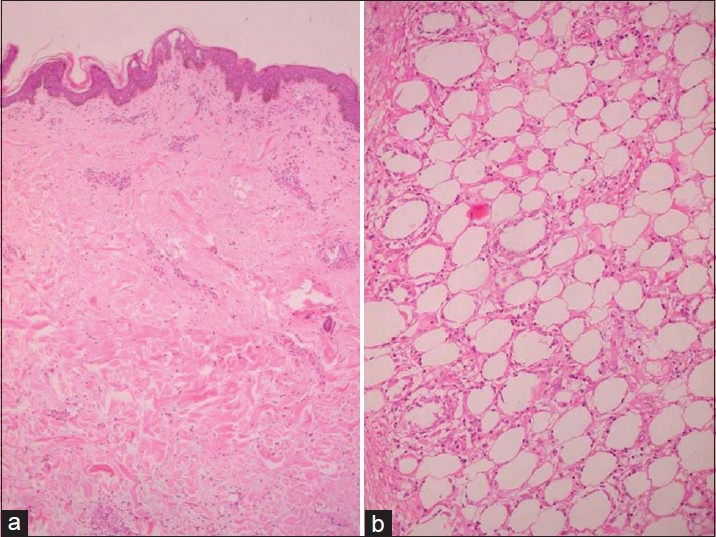
| Fig. 1 (a) Photomicrograph showing unremarkable epidermis and dermis (H and E, ×10) and (b) showing subcutis infiltrated by atypical lymphoid cells with rimming of adipocytes (H and E, ×40)
SPTCL is rare accounting for less than 1% of all NHLs. It has a wide age range usually occurring in the elderly (median age 64 years) with a slight male preponderance. It involves the extremities and trunk, usually presenting as multiple subcutaneous nodules, symptoms being primarily related to these nodules. The association of SPTCL with other malignancies is unusual, though they have been reported in allograft recipients and in a case of ovarian carcinoma.[3,4] Here, immunosuppression appears to be a predisposing factor.
CASE REPORT
A 42-year-old lady, presented with two indurated and painful patches in the lower part of her anterior abdominal wall, the right hypochondriac and lumbar regions. This was three months after completing chemotherapy and radiotherapy for a squamous cell carcinoma of the cervix for which she had been operated five months prior to the present complaint. She had received treatment at another hospital.
On local examination, there was an ill-defined, diffuse thickening and hardening of the abdominal wall. FNAC was attempted but yielded scanty material, hence was inconclusive. An incisional biopsy was performed and submitted for histopathology.
PATHOLOGIC FINDINGS
Grossly, the specimen was skin covered tissue measuring 6 × 5.5 × 4.5 cm. The external and cut surfaces were unremarkable except for a few thickened whitish streaks in the subcutis.
Microscopically, there was an unremarkable epidermis and dermis [Figure 1a]. The subcutis had a diffuse infiltrate of small-to-medium-sized atypical lymphoid cells with a few larger cells with prominent nucleoli [Figure 1b]. The tumor cells were seen rimming adipocytes [Figure 2a]. Mitotic activity was brisk with abundant karyorrhectic debris. Foci of angioinvasion were seen [Figure 2b]. Histiocytic aggregates forming ill-defined granulomas were present. Numerous lipid laden foamy histiocytes were also seen. There was no evidence of a metastatic carcinoma.
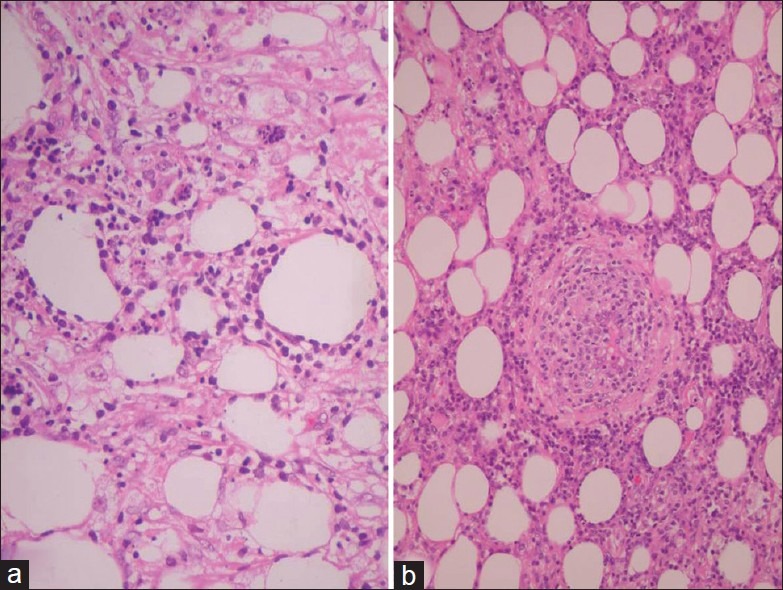
| Fig. 2 (a) Photomicrograph showing karyorrhectic debris (H and E,×40) and (b) showing angiocentricity (H and E, ×40)
Immunohistochemistry was performed on these sections. The lymphoid cells were found to be positive for CD8 [Figure 3], but negative for CD4. They were also positive for T-cell markers like CD3 and CD43 [Figure 3]. They were negative for CD30, CD56, CD79a and CD20 [Figure 3]. Thus, a diagnosis of a subcutaneous panniculitis-like T-cell lymphoma was concluded.
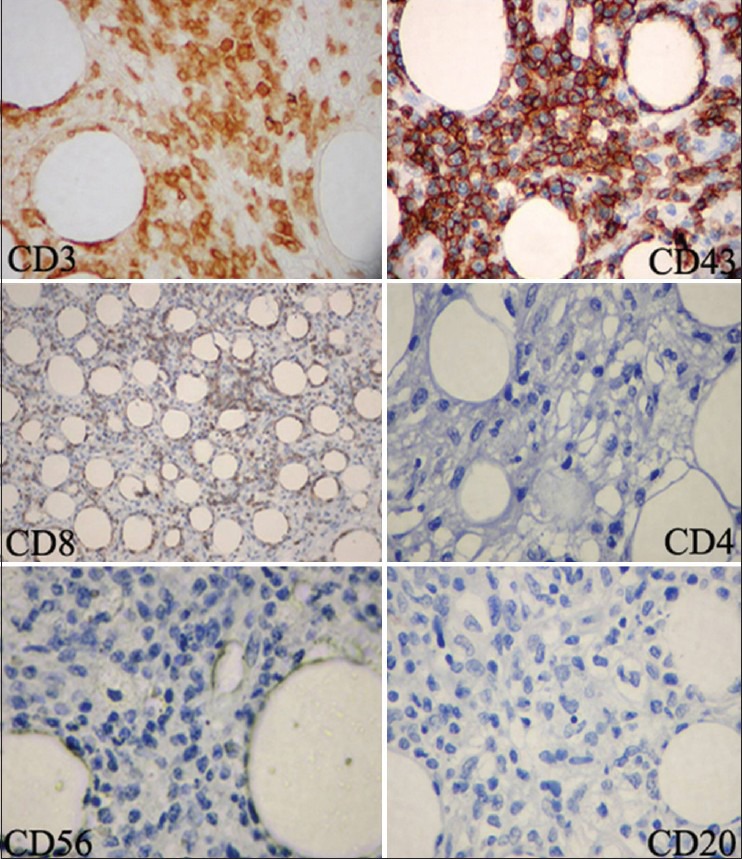
| Fig. 3 Photomicrograph showing positivity for CD3, CD43, CD8. CD20, CD4 and CD56 are negative (IHC, ×40)
The paraffin block of the initial cervical biopsy was requisitioned and sections reviewed and showed features of a poorly differentiated squamous cell carcinoma [Figure 4]. Following this, the patient received two cycles of CHOP regimen with substantial reduction in pain and induration. While on treatment, however, she developed spotting per vaginam. A pap smear from the vaginal vault revealed a recurrent carcinoma. Subsequently the patient was lost to follow-up. A telephonic enquiry revealed that she had died ten months after the diagnosis.
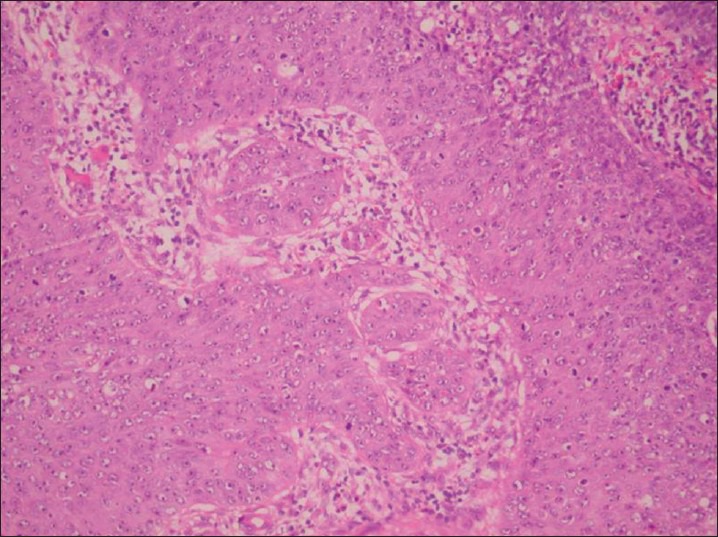
| Fig. 4 Photomicrograph showing squamous cell carcinoma of the cervix (H and E, ×40)
DISCUSSION
SPTCL is a rare entity,[1] accounting for less than 1% of all NHLs. Its association in immunosuppressed states has been reported;[3,4] however, its synchronous or metachronous occurrence in treated cases of cervical carcinomas has not been reported hitherto in the English literature. Most SPTCLs occur sporadically.
SPTCL, as the name indicates, infiltrates diffusely through the subcutaneous tissue while sparing the dermis and epidermis,[2] except in the gamma-delta subtype, where the mid and deep dermis may be involved.[5] The lace-like pattern of infiltration resembles a lobular panniculitis. The atypical cells range from small-to-medium to large cells with brisk mitoses, necrosis, karyorrhexis and angioinvasion. A typical rimming of adipocytes by tumor cells is characteristic. Often admixed reactive histiocytes are seen many of which may have finely vacuolated cytoplasm. Histiocytic aggregates forming granulomas are also present.[1]
Immunophenotypically, these cells have a mature T-cell phenotype, are CD8 positive and CD4 negative.[1,6] They also express cytotoxic molecules like T-cell intracellular antigen (TIA-1), perforin and granzyme B.[7,8,9] Most cases express alpha beta T-cell receptor gene rearrangement, but up to 25% express gamma-delta T-cell receptor gene rearrangement.[1,5] These latter cases may be positive for CD56.[7]
Association with other malignancies is rare though immunosuppression appears to be a predisposing factor, especially in those with a gamma-delta phenotype. Renal allograft recipients and occasional cardiac allograft patients with SPTCL have been reported.[3] The only other report of it arising after chemotherapy for a case of ovarian carcinoma has been recently published.[4]
However, its occurrence in the setting of a treated case of carcinoma cervix has not been reported. In these circumstances, the possible role of immunosuppression as an etiopathogenetic factor could be considered.
SPTCLs are lymphomas for which treatment modalities are as yet not well defined. The cell of origin is the cytotoxic T-cell.[8] SPTCL arising as a second malignancy is very unusual. In this case it is possible that it had arisen in a state of immunosuppression, as a result of chemotherapy and radiotherapy for the earlier carcinoma cervix.
The potential for aggressive behavior warrants an early diagnosis with an extended panel of immunohistochemical stains for optimal patient outcome.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
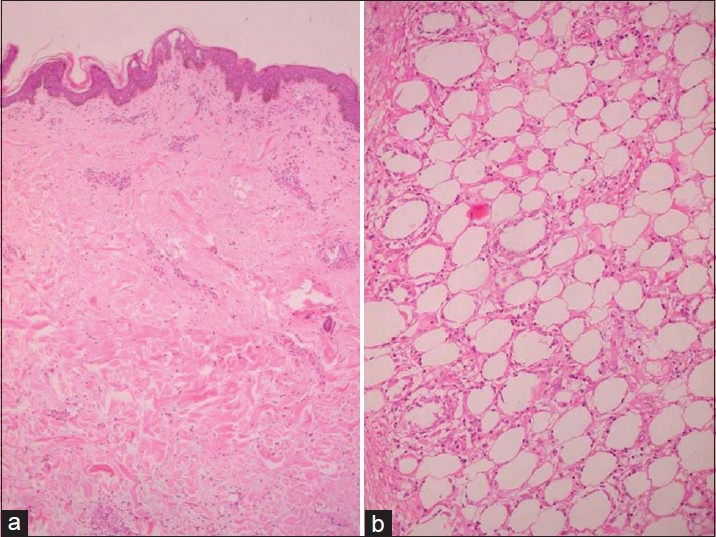
| Fig. 1 (a) Photomicrograph showing unremarkable epidermis and dermis (H and E, ×10) and (b) showing subcutis infiltrated by atypical lymphoid cells with rimming of adipocytes (H and E, ×40)
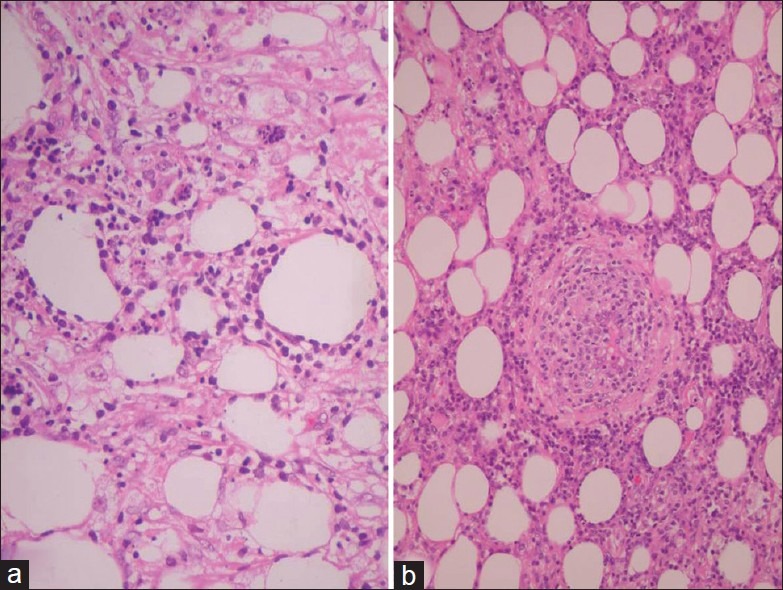
| Fig. 2 (a) Photomicrograph showing karyorrhectic debris (H and E,×40) and (b) showing angiocentricity (H and E, ×40)
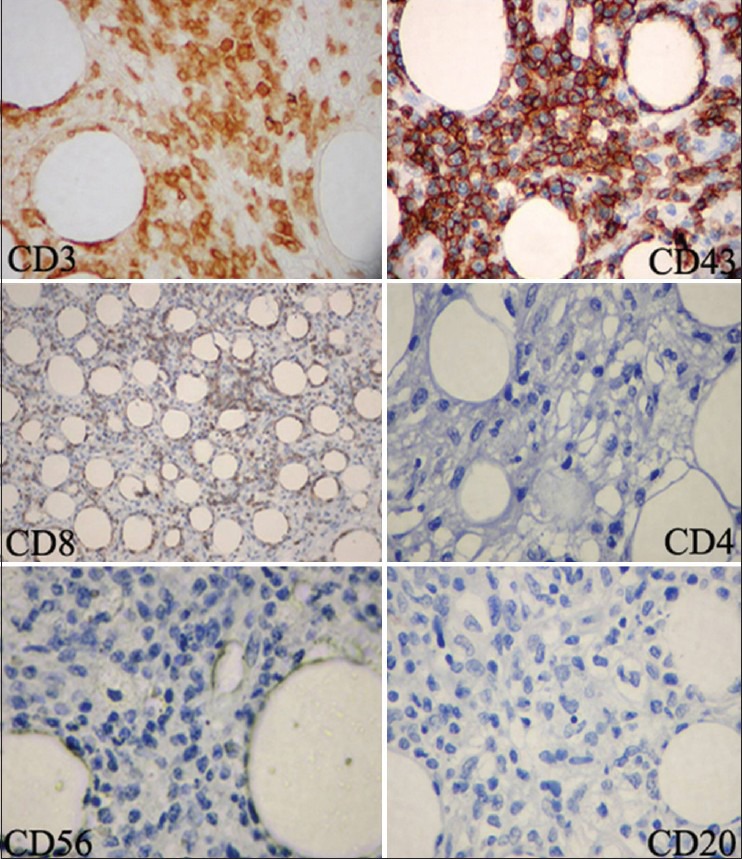
| Fig. 3 Photomicrograph showing positivity for CD3, CD43, CD8. CD20, CD4 and CD56 are negative (IHC, ×40)
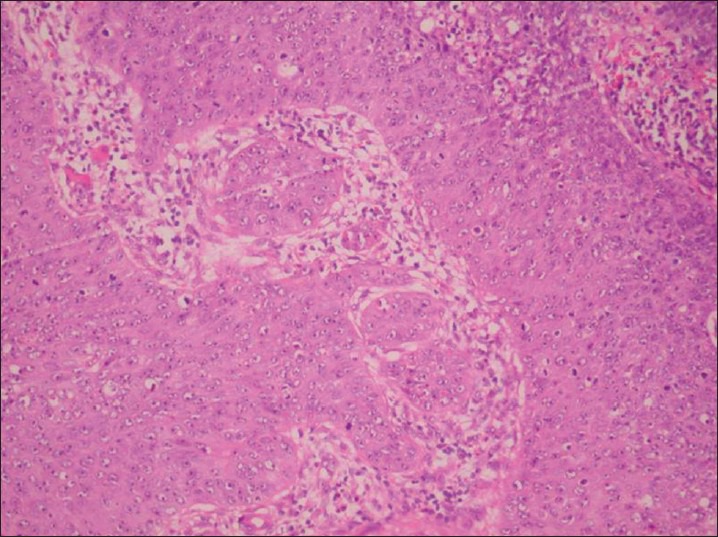
| Fig. 4 Photomicrograph showing squamous cell carcinoma of the cervix (H and E, ×40)


 PDF
PDF  Views
Views  Share
Share

