Treatment Refusal and Abandonment Remain Major Concerns Despite Good Outcomes with Multi-Modality Management in Pediatric Medulloblastoma: Experience from a Cancer Center in Eastern India
CC BY-NC-ND 4.0 ? Indian J Med Paediatr Oncol 2019; 40(S 01): S13-S15
DOI: DOI: 10.4103/ijmpo.ijmpo_213_17
Abstract
Context:?Survival in medulloblastoma, the most common pediatric brain tumor, has lagged behind in developing countries in comparison to the West.?Aim:?The aim of this study was to analyze the clinical profile and outcome in a cancer center in Eastern India.?Methods:?Twenty-nine children were retrospectively analyzed over 6 years.?Results:?Vomiting (79%), headache (69%), and unsteadiness (55%) were the presenting complaints. The majority (67%) had classical histology. High-risk (HR) disease (61.6%) exceeded average-risk (AR) (38.4%) disease in numbers. Treatment-refusal (27.6%) and abandonment (6.9%) were major concerns. Four-year EFS was 81% and 52%, excluding and including refusal/abandonment, respectively. There was no relapse/progression among AR patients. Four-year EFS in HR was 63%. Posterior fossa syndrome (37.5%), febrile neutropenia (29%), and ototoxicity (16.7%) were the main treatment-related morbidities.?Implications:?Following this audit, patient tracking to reduce abandonment, coordination to limit delay in postsurgical referral, developing strategies for molecular subgrouping, and reducing cumulative cisplatin exposure were measures adopted to improve outcome in the unit.
Publication History
Publication Date:
24 May 2021 (online)
? 2019. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/).
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Context:?Survival in medulloblastoma, the most common pediatric brain tumor, has lagged behind in developing countries in comparison to the West.?Aim:?The aim of this study was to analyze the clinical profile and outcome in a cancer center in Eastern India.?Methods:?Twenty-nine children were retrospectively analyzed over 6 years.?Results:?Vomiting (79%), headache (69%), and unsteadiness (55%) were the presenting complaints. The majority (67%) had classical histology. High-risk (HR) disease (61.6%) exceeded average-risk (AR) (38.4%) disease in numbers. Treatment-refusal (27.6%) and abandonment (6.9%) were major concerns. Four-year EFS was 81% and 52%, excluding and including refusal/abandonment, respectively. There was no relapse/progression among AR patients. Four-year EFS in HR was 63%. Posterior fossa syndrome (37.5%), febrile neutropenia (29%), and ototoxicity (16.7%) were the main treatment-related morbidities.?Implications:?Following this audit, patient tracking to reduce abandonment, coordination to limit delay in postsurgical referral, developing strategies for molecular subgrouping, and reducing cumulative cisplatin exposure were measures adopted to improve outcome in the unit.
Introduction
Central nervous system tumors are second only to hematological malignancies among childhood cancers. Medulloblastoma is the most frequent brain tumor in children.[1] Cure rates with multimodality treatment approaches 85% for average-risk (AR) and 75% for high-risk (HR) patients.[2] Data from India are limited.[3] [4] [5] [6] [7] The aim of the study was to analyze the clinical profile and outcome in a referral oncology center in Eastern India over the last 6 years.
Materials and Methods
All children, <18>3-years at diagnosis, with postoperative residual <1>3-years with HR disease received 36 Gy in 20-fractions. All children >3-years received boost to the posterior fossa/tumor bed with a dose of 55.8 Gy in 31-fractions. None received concurrent chemotherapy with radiation. Children <3>
Results
Twenty-nine children were included in this study. Median age was 7 years (range: 0.9?14). Sixteen (55%) were male. Median symptom-interval was 3.7 months (range: 1?12). Clinical features at diagnosis included vomiting (23, 79%), headache (20; 69%), unsteadiness of gait (16; 55%), and cranial nerve palsy (3; 10%). On the preoperative MRI (n?= 25), the location of the tumor was in the midline cerebellum (10; 40%), roof of the 4th ventricle (10; 40%), and lateral cerebellum (5; 20%). Surgical data were available in 19; 9 (47%) had gross tumor excision, 4 (21%) had near total removal, and 6 (31.5%) had subtotal resection. A ventriculoperitoneal shunt had been inserted in 14/23 (61%). Pathological subtype was documented in the reports of 12 patients: classical (8; 67%), desmoplastic/nodular (2; 16.5%), and LCA (2; 16.5%). Staging (n?= 25) revealed 12 (48%) with localized disease, 3 (12%) with malignant cells in the CSF, 7 (28%) with disease in the spine, and 3 (12%) with distant metastasis in the liver and bones. Sixteen had HR (61.6%) and 10 (38.4%) had AR disease. Out of the 16 children with HR disease, 13, including two children <3>1.5 cm 2, and one was 1.7 years old. Data were incomplete in three children.
Among the 29 children, 8 (27.6%) refused treatment and 2 (6.9%) abandoned care. All had HR disease. One child (3.4%) opted for palliative care in view of metastatic disease. Three (10.3%) had recurrence/progressive disease on follow-up. The remaining 15 (51.7%) children are well on follow-up. Median follow-up duration for the entire cohort was 54 months. The median 4-year event-free survival (EFS) was 81.4% ? 0.1% and 51.2% ? 0.1%, excluding and including refusal/abandonment, respectively. There were no relapses/progressive disease, or refusal/abandonment among AR patients (EFS = 100%). Among HR patients, EFS, excluding refusal/abandonment was 63.4% ? 0.1% [Figure 1] and including refusal/abandonment was 31.1% ? 1.2%.
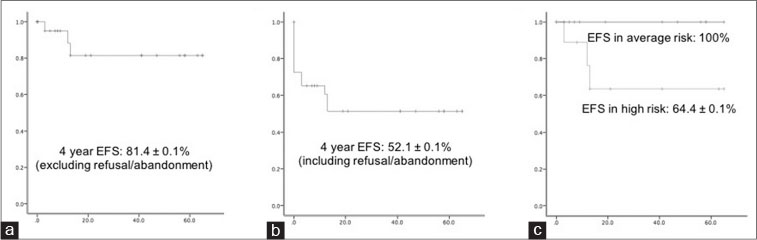
|?Figure. 1? Event free survival in children with medulloblastoma: (a) excluding refusal and abandonment; (b) including refusal and abandonment as events; (c) event-free survival in children with average and high-risk disease at median follow-up of 54 months (cases with refusal/abandonment were censored)|
Data related to treatment-related toxicity was available in 24 children. About 9 (37.5%) had posterior fossa syndrome, 7 (29%) needed admissions for febrile neutropenia, 1 (4%) had a shunt block, and 4 (16.7%) had hearing loss. All needed nutritional support. There was no death related to treatment toxicity.
Discussion
With the rapid introduction of molecular profiling in clinical classification, management of pediatric brain tumors, including medulloblastoma, is likely to undergo a paradigm change.[1] However, the developing countries are struggling with providing optimal care to children with potentially curable brain tumors. Access to care and treatment refusal/abandonment remain important concerns. This has been highlighted in previous studies from Asia, Africa, and Latin America.[8] [9] [10] The index series reports 35% refusing/abandoning care. The retrospective nature of the audit precluded detailed analysis of the possible reasons for default. However, patient tracking over telephone has been prospectively activated in our center to counter this menace, using workforce, and financial support from government and voluntary groups.
Despite limited numbers, the protocol-based standardized management for the AR patients produced satisfactory results. The higher proportion of HR patients was plausibly due to referral bias. The previous studies from India have reported the survival in the AR group varies between 73% and 83% and among HR, between 34% and 63%, similar to the index study [Table 1].[3] [4] [5] [6] Lack of molecular subgrouping is recognized as a lacuna in most of these studies. An additional limitation was that there were only three children below 3 years of age, one of whom had progressive disease, and the other two had defaulted. It is well established that this challenging subgroup of patients need a dedicated approach different from that for older children.
|
Author |
Center |
Year |
n |
Survival |
|---|---|---|---|---|
|
Muzumdar et al. [4] |
Mumbai |
2011 |
365 |
5-year progression free survival: 73% (average risk), 34% (high risk) |
|
Menon et al.[3] |
Trivandrum |
2006 |
79 |
5-year overall survival: 24% |
|
Kumar et al.[6] |
Hyderabad |
2015 |
31 |
3-year overall survival: 40% |
|
Das et al. (current study) |
Kolkata |
2018 |
26 |
4-year event-free survival: 100% (average risk), 63% (high risk) |
|
Gupta et al.[5] |
Mumbai |
2012 |
20 |
3-years relapse-free survival: 83% (average risk, age <5> |
- Gupta T, Sarkar C, Rajshekhar V, Chatterjee S, Shirsat N, Muzumdar D. et al.?Indian Society of Neuro-Oncology consensus guidelines for the contemporary management of medulloblastoma. Neurol India 2017; 65: 315-32
- Gajjar A, Chintagumpala M, Ashley D, Kellie S, Kun LE, Merchant TE. et al.?Risk-adapted craniospinal radiotherapy followed by high-dose chemotherapy and stem-cell rescue in children with newly diagnosed medulloblastoma (St. Jude Medulloblastoma-96): Long-term results from a prospective, multicentre trial. Lancet Oncol 2006; 7: 813-20
- Menon G, Nair S, Muthurethinam T, Krishnakumar K, Bhattacharya RN.?Medulloblastoma in children: Prognostic factors and predictors of outcome. J Pediatr Neurosci 2006; 1: 16-20
- Muzumdar D, Deshpande A, Kumar R, Sharma A, Goel N, Dange N. et al.?Medulloblastoma in childhood-King Edward memorial hospital surgical experience and review: Comparative analysis of the case series of 365 patients. J Pediatr Neurosci 2011; 6: S78-85
- Gupta T, Jalali R, Goswami S, Nair V, Moiyadi A, Epari S. et al.?Early clinical outcomes demonstrate preserved cognitive function in children with average-risk medulloblastoma when treated with hyperfractionated radiation therapy. Int J Radiat Oncol Biol Phys 2012; 83: 1534-40
- Kumar LP, Deepa SF, Moinca I, Suresh P, Naidu KV.?Medulloblastoma: A common pediatric tumor: Prognostic factors and predictors of outcome. Asian J Neurosurg 2015; 10: 50
- Gaur S, Kumar SS, Balasubramaniam P.?An analysis of medulloblastoma: 10 year experience of a referral institution in South India. Indian J Cancer 2015; 52: 575-8
- Rajagopal R, Abd-Ghafar S, Ganesan D, Bustam Mainudin AZ, Wong KT, Ramli N. et al.?Challenges of treating childhood medulloblastoma in a country with limited resources: 20 years of experience at a single tertiary center in Malaysia. J Glob Oncol 2017; 3: 143-56
- Wang C, Yuan XJ, Jiang MW, Wang LF.?Clinical characteristics and abandonment and outcome of treatment in 67 Chinese children with medulloblastoma. J Neurosurg Pediatr 2016; 17: 49-56
- Friedrich P, Lam CG, Kaur G, Itriago E, Ribeiro RC, Arora RS. et al.?Determinants of treatment abandonment in childhood cancer: Results from a global survey. PLoS One 2016; 11: e0163090
- Nageswara Rao AA, Wallace DJ, Billups C, Boyett JM, Gajjar A, Packer RJ. et al.?Cumulative cisplatin dose is not associated with event-free or overall survival in children with newly diagnosed average-risk medulloblastoma treated with cisplatin based adjuvant chemotherapy: Report from the Children?s Oncology Group. Pediatr Blood Cancer 2014; 61: 102-6
Address for correspondence
Publication History
Publication Date:
24 May 2021 (online)
? 2019. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial-License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/).
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
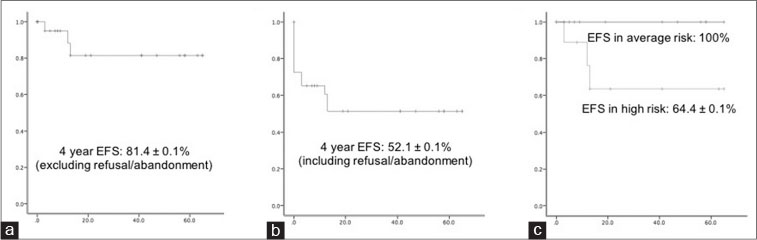
|?Figure. 1? Event free survival in children with medulloblastoma: (a) excluding refusal and abandonment; (b) including refusal and abandonment as events; (c) event-free survival in children with average and high-risk disease at median follow-up of 54 months (cases with refusal/abandonment were censored)|
References
- Gupta T, Sarkar C, Rajshekhar V, Chatterjee S, Shirsat N, Muzumdar D. et al.?Indian Society of Neuro-Oncology consensus guidelines for the contemporary management of medulloblastoma. Neurol India 2017; 65: 315-32
- Gajjar A, Chintagumpala M, Ashley D, Kellie S, Kun LE, Merchant TE. et al.?Risk-adapted craniospinal radiotherapy followed by high-dose chemotherapy and stem-cell rescue in children with newly diagnosed medulloblastoma (St. Jude Medulloblastoma-96): Long-term results from a prospective, multicentre trial. Lancet Oncol 2006; 7: 813-20
- Menon G, Nair S, Muthurethinam T, Krishnakumar K, Bhattacharya RN.?Medulloblastoma in children: Prognostic factors and predictors of outcome. J Pediatr Neurosci 2006; 1: 16-20
- Muzumdar D, Deshpande A, Kumar R, Sharma A, Goel N, Dange N. et al.?Medulloblastoma in childhood-King Edward memorial hospital surgical experience and review: Comparative analysis of the case series of 365 patients. J Pediatr Neurosci 2011; 6: S78-85
- Gupta T, Jalali R, Goswami S, Nair V, Moiyadi A, Epari S. et al.?Early clinical outcomes demonstrate preserved cognitive function in children with average-risk medulloblastoma when treated with hyperfractionated radiation therapy. Int J Radiat Oncol Biol Phys 2012; 83: 1534-40
- Kumar LP, Deepa SF, Moinca I, Suresh P, Naidu KV.?Medulloblastoma: A common pediatric tumor: Prognostic factors and predictors of outcome. Asian J Neurosurg 2015; 10: 50
- Gaur S, Kumar SS, Balasubramaniam P.?An analysis of medulloblastoma: 10 year experience of a referral institution in South India. Indian J Cancer 2015; 52: 575-8
- Rajagopal R, Abd-Ghafar S, Ganesan D, Bustam Mainudin AZ, Wong KT, Ramli N. et al.?Challenges of treating childhood medulloblastoma in a country with limited resources: 20 years of experience at a single tertiary center in Malaysia. J Glob Oncol 2017; 3: 143-56
- Wang C, Yuan XJ, Jiang MW, Wang LF.?Clinical characteristics and abandonment and outcome of treatment in 67 Chinese children with medulloblastoma. J Neurosurg Pediatr 2016; 17: 49-56
- Friedrich P, Lam CG, Kaur G, Itriago E, Ribeiro RC, Arora RS. et al.?Determinants of treatment abandonment in childhood cancer: Results from a global survey. PLoS One 2016; 11: e0163090
- Nageswara Rao AA, Wallace DJ, Billups C, Boyett JM, Gajjar A, Packer RJ. et al.?Cumulative cisplatin dose is not associated with event-free or overall survival in children with newly diagnosed average-risk medulloblastoma treated with cisplatin based adjuvant chemotherapy: Report from the Children?s Oncology Group. Pediatr Blood Cancer 2014; 61: 102-6


 PDF
PDF  Views
Views  Share
Share

