Virtual Teaching and Training Models in Pediatric Oncology: A Retrospective Study from an LMIC
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2022; 43(03): 241-249
DOI: DOI: 10.1055/s-0042-1750206
Abstract
Introduction A multidisciplinary approach is essential for success in pediatric oncology treatment. Updated protocols, quality nursing care, psychosocial support, safe and standardized preparation of chemotherapy, infection control, and effective data management are key shareholders for the effective management of childhood cancer. The Department of Pediatric Oncology at Indus Hospital and Health Network (IHHN) initiated consistent teaching and trainings with the help of the My Child Matters Grant from Sanofi Espoir Foundation. These courses were conducted in person starting in 2019 and had to be postponed and restructured due to coronavirus (COVID-19) pandemic in early 2020.
Objectives The aim of this study was to determine the impact of virtual teaching models for healthcare workers employed in pediatric hematology/oncology departments in low-resource settings.
Materials and Methods After in-person courses in 2019, courses for all six disciplines (physicians, nursing, infection control, pharmacy, psychosocial care, and cancer registry) were conducted virtually starting December 2020, open to all and free of cost. A total of 878 registrations were obtained and 267 certifications given. Lectures with Q&A sessions were conducted via zoom and recordings shared through email. Each course was conducted by the relevant department at IHHN with pre- and postassessment conducted through Google Forms. Session feedback was taken through zoom polls and a comprehensive course feedback conducted after completion; e-certificates were awarded to successful participants according to a predetermined criterion.
Results A total of 434 physicians' registrations were done from around Pakistan and countries like Saudi Arabia, Malaysia, Jordan, and Canada for the online physicians' course, of which 110 received certifications after completing post-test and attendance criteria of 55%. Pharmacy, infection control, psychosocial care, and cancer registry courses saw participation and certification of 51, 41, 24, and 14 participants, respectively. Online sessions received positive feedback in terms of instructors, course content, convenience, and access from over 90% participants.
Conclusion Due to the ease in coordinating hectic schedules and cost-effectiveness of online lectures, this virtual teaching model will persist despite the trajectory of the COVID-19 pandemic. Similar ventures aimed at pediatric oncology teaching and training are needed in a widespread manner to improve outcomes of childhood cancer.
Publication History
Article published online:
02 July 2022
© 2022. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Introduction A multidisciplinary approach is essential for success in pediatric oncology treatment. Updated protocols, quality nursing care, psychosocial support, safe and standardized preparation of chemotherapy, infection control, and effective data management are key shareholders for the effective management of childhood cancer. The Department of Pediatric Oncology at Indus Hospital and Health Network (IHHN) initiated consistent teaching and trainings with the help of the My Child Matters Grant from Sanofi Espoir Foundation. These courses were conducted in person starting in 2019 and had to be postponed and restructured due to coronavirus (COVID-19) pandemic in early 2020.
Objectives The aim of this study was to determine the impact of virtual teaching models for healthcare workers employed in pediatric hematology/oncology departments in low-resource settings.
Materials and Methods After in-person courses in 2019, courses for all six disciplines (physicians, nursing, infection control, pharmacy, psychosocial care, and cancer registry) were conducted virtually starting December 2020, open to all and free of cost. A total of 878 registrations were obtained and 267 certifications given. Lectures with Q&A sessions were conducted via zoom and recordings shared through email. Each course was conducted by the relevant department at IHHN with pre- and postassessment conducted through Google Forms. Session feedback was taken through zoom polls and a comprehensive course feedback conducted after completion; e-certificates were awarded to successful participants according to a predetermined criterion.
Results A total of 434 physicians' registrations were done from around Pakistan and countries like Saudi Arabia, Malaysia, Jordan, and Canada for the online physicians' course, of which 110 received certifications after completing post-test and attendance criteria of 55%. Pharmacy, infection control, psychosocial care, and cancer registry courses saw participation and certification of 51, 41, 24, and 14 participants, respectively. Online sessions received positive feedback in terms of instructors, course content, convenience, and access from over 90% participants.
Conclusion Due to the ease in coordinating hectic schedules and cost-effectiveness of online lectures, this virtual teaching model will persist despite the trajectory of the COVID-19 pandemic. Similar ventures aimed at pediatric oncology teaching and training are needed in a widespread manner to improve outcomes of childhood cancer.
Keywords
education - pediatrics - capacity building - mentorshipIntroduction
One of the greatest challenges that low-to-middle income countries (LMIC) face in the realm of childhood cancer is the lack of specialist pediatric oncologists, nurses, and other personnel. Over 8,000 patients are diagnosed with cancer each year in Pakistan, an underestimated figure due to lack of access to facilities and diagnosis.[1] A meager number of seven physician fellowship programs in pediatric hematology/oncology are registered with College of Physicians and Surgeons Pakistan, requiring a minimum 2-year commitment after first fellowship in pediatrics.[2] Similarly, specialized oncology training in nursing is mostly done informally instead of mandatory focused educational programs. In 2009, the first Pediatric Oncology Nurse Technician 1-year diploma was initiated by the Sindh Board,[3] but due to limited access, most nurses practicing in childhood cancer wards are unequipped in specialized skills. The difficulty of attaining a position in the limited training programs coupled with the commitment of traveling long distances to cities has led to a dire shortage of specialists in smaller urban and rural centers across the country. Despite there being roughly 13 pediatric oncology units (POUs) currently functioning in Pakistan,[1] most of these units are consequently lacking formally trained pediatric oncology healthcare teams, leading to stunted progress in capacity and quality of available care.
In line with the World Cancer Declaration drafted in 2013, nations need to focus on increasing number of training opportunities available for health professionals in different aspects of cancer control.[4] The Indus Hospital and Health Network (IHHN) was awarded the My Child Matters (MCM) grant by the Sanofi Espoir Foundation for teaching and capacity building in POUs across Pakistan in 2009. Along with oncologists, pediatricians, and nurses, theoretical and hands-on courses for clinical pharmacists, psychosocial staff, infection control specialists, and cancer registry operators have also been developed and implemented.
The coronavirus (COVID-19) pandemic provided the world of medicine with a unique opportunity to revolutionize healthcare via the incorporation of technology for education of healthcare workers and delivery of patient care. Telehealth has given medical professionals the ability to learn from experts around the world and several medical societies have made webinars and online lessons easily accessible and free of cost.[5] There are several benefits of telehealth and education in pediatric oncology care, improving patient care through advancements in clinical aptitude an virtual case discussions as shown in Brazil.[6] The objective of our initiative was to use similar virtual techniques for education and trainings and ultimately improve survival rates of children with cancer, especially in third-world countries and underprivileged areas within developed countries.
Materials and Methods
This is a commentary article on the period from January to December 2020, during which courses were conducted through purely virtual modes of teaching due to the COVID-19 pandemic. The focus of these training programs was primarily on the 10 IHHN-partnered POUs; however, registrations were open to the general public, completely free of cost. This was a major shift from the previously followed format of in-person courses requiring physical presence of individuals from each unit at IHHN Korangi Campus. After onset of COVID-19, MCM funds were redirected to improving infrastructure of POUs. Teleconferencing equipment sets (LED screens, webcam, keyboard, CPU) along with reliable and prepaid internet connections were sent to nine partnered centers, ensuring consistent participation by a larger number of staff than was possible previously.
The physicians' course was divided into leukemia, lymphoma, solid tumors, and supportive care and therapy modules with weekly sessions for 13 weeks. Nursing course sessions were biweekly for 1 month. Psychosocial, infection control, pharmacy, and cancer registry courses were held daily for 1 week each. Course objectives and content were designed by specialists from each discipline, adapted from standardized lecture series, as shown in [Table 1]. The target audiences for each course are also included in [Table 1], with flyers and course registration forms circulated on public forums 2 weeks before starting date, as well as through unit heads and personal contacts. External, in-house, and international faculty from different institutions were engaged as specialist instructors. The MCM-partnered centers did not have specialized nurses, physicians, and other healthcare workers; therefore, all necessary basics of pediatric oncology knowledge were included as assessed by field experts at IHHN. These gaps in training were evaluated during the course of partnership under the grant.
|
N. |
Courses conducted |
Duration (h) |
|---|---|---|
|
1. |
Physicians' course: |
|
|
Target: Pediatricians, junior fellows, and medical officers working in POUs |
||
|
i |
Childhood cancer status in Pakistan and when to suspect Malignancy |
1 hour |
|
Leukemia module |
||
|
ii |
Approach to a child with suspected leukemia |
1.5 hours |
|
iii |
Pediatric oncological emergencies; hyper leucocytosis and TLS |
1 hour |
|
iv |
Blood transfusion guidelines and transfusion reactions |
1 hour |
|
v |
AML, CML, and JMML management guidelines |
1 hour |
|
Lymphoma module |
||
|
vi |
Hodgkin lymphoma in children; classification, workup, and management |
1 hour |
|
vii |
Non-Hodgkin lymphoma in children; workup and management |
1 hour |
|
Solid tumor module |
||
|
viii |
Approach to abdominal masses in children |
1 hour |
|
ix |
Approach to brain tumor |
1.5 hours |
|
x |
Approach to retinoblastoma |
1.5 hours |
|
Supportive care and therapy module |
||
|
xi |
Pain management and psychosocial support |
1 hour |
|
xii |
Management of infections in immunocompromised patients |
1 hour |
|
xiii |
Breaking bad news |
1 hour |
|
2. |
Nursing course |
|
|
Target: Nurses and students with an interest or posting in POUs |
||
|
i |
Pediatric cancers, treatment, and oncological emergencies |
1 hour |
|
ii |
Chemotherapy and toxicity |
1 hour |
|
iii |
Safe handling and immediate complications |
1 hour |
|
iv |
Procedure and CVAD |
1 hour |
|
v |
Blood transfusion and reactions, nutrition |
1 hour |
|
vi |
Supportive care and caring for caregivers |
1 hour |
|
vii |
Survivorship and grieving and counselling |
1 hour |
|
viii |
Pediatric cancers |
1 hour |
|
3. |
Pharmacy course |
|
|
Target: Clinical pharmacists, nurses, technicians, and other HCWs involved in chemotherapy preparation |
||
|
i |
Introduction to oncology pharmacy and standards of practice |
1 hour |
|
ii |
Classification of anticancer agents and potential interactions |
1 hour |
|
iii |
Chemotherapy toxicity and symptoms management |
1 hour |
|
iv |
Supportive care medications |
1 hour |
|
v |
Use of antimicrobials in cancer patients |
1 hour |
|
4. |
Psychosocial course |
|
|
Target: Psychologists, social workers, and physicians involved in counselling of childhood cancer patients |
||
|
i |
Basics of psychosocial care for pediatric patients |
1 hour |
|
ii |
Communicating with pediatric patients and their families |
1 hour |
|
iii |
Breaking bad news |
1 hour |
|
iv |
Grief and trauma |
1 hour |
|
v |
Self-care for professionals |
1 hour |
|
5. |
Infection control course |
|
|
Target: Infection control practitioners and nurses |
||
|
i |
Introduction to IPC program and facility assessment |
1 hour |
|
ii |
Transmission-based precautions aseptic technique: concepts and principles |
1 hour |
|
iii |
COVID-19 prevention and control |
1 hour |
|
iv |
Environmental cleaning and disinfection: best practices in resource-limiting settings |
1 hour |
|
v |
Construction and renovation in oncology unit |
1 hour |
|
vi |
Safe handle of linen in immunocompromised population waste management |
1 hour |
|
6. |
Cancer registry course: |
|
|
Target: Childhood cancer registry data entry operators and supervising physicians |
||
|
i |
Introduction to cancer registry |
1 hour |
|
ii |
Introduction to ICD-O3 |
1.5 hours |
|
iii |
Chemotherapy toxicity and symptoms management |
1 hour |
|
iv |
Supportive care medications |
1 hour |
|
7. |
Disease-specific protocol discussion sessions for physicians—Level 2 |
|
|
Target: Oncopediatricians and fellows at partnered POUs |
||
|
i |
ALL |
1.5 hours |
|
ii |
APML |
1.5 hours |
|
iii |
Hepatoblastoma |
1.5 hours |
|
iv |
Germ cell tumors |
1.5 hours |
|
v |
Wilms tumor |
1.5 hours |
|
vi |
Neuroblastoma |
1 hour |
|
vii |
Retinoblastoma |
1.5 hours |
|
viii |
Medulloblastoma and other CNS tumors |
1.5 hours |
|
ix |
Bone tumors |
1.5 hours |
|
x |
LCH and sarcomas |
1.5 hours |
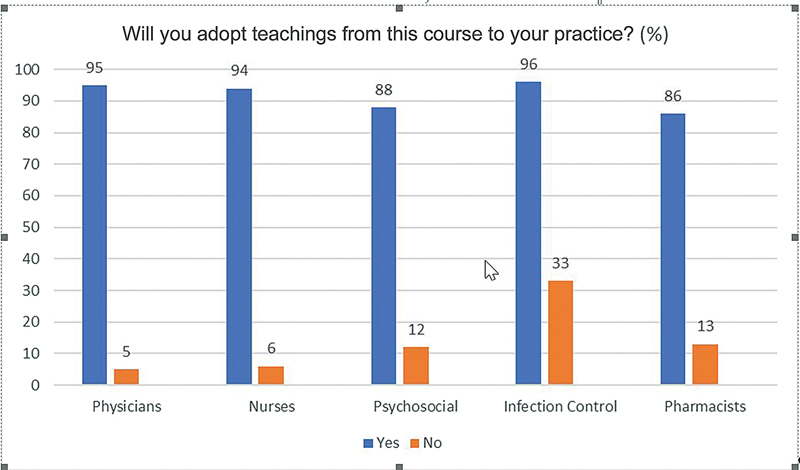
| Figure 1:Feedback responses (course teachings).
|
Physicians |
Nurses |
Pharmacists |
Psychosocial |
Infection control |
Cancer registry |
|
|---|---|---|---|---|---|---|
|
Total registrations |
434 |
68 |
135 |
67 |
147 |
27 |
|
Total certifications |
109 (25%) |
28 (41%) |
51 (38%) |
24 (36%) |
41 (28%) |
14 (52%) |
|
Partnered units |
64/109 (58.7%) |
22/28 (78.6%) |
35/51 (68.6%) |
11/24 (45.8%) |
15/41 (36.6%) |
13/14 (92.9%) |
|
Physicians |
Nurses |
Pharmacists |
Psychosocial |
Infection control |
Cancer registry |
|
|
Avg. pretest |
23/40 (56.2%) |
13/19 (68.4%) |
12/15 (80%) |
11/19 (57.9%) |
17/30 (56.7%) |
22/29 (75.9%) |
|
Avg. post-test |
29/40 (71.9%) |
15/19 (78.9%) |
13/15 (86.7%) |
11/19 (57.9%) |
20/30 (66.7%) |
23/29 (79.3%) |
|
p-Value (two-tailed) |
0.001789 |
0.043325 |
0.004534 |
0.012372 |
0.000265 |
0.0976 |
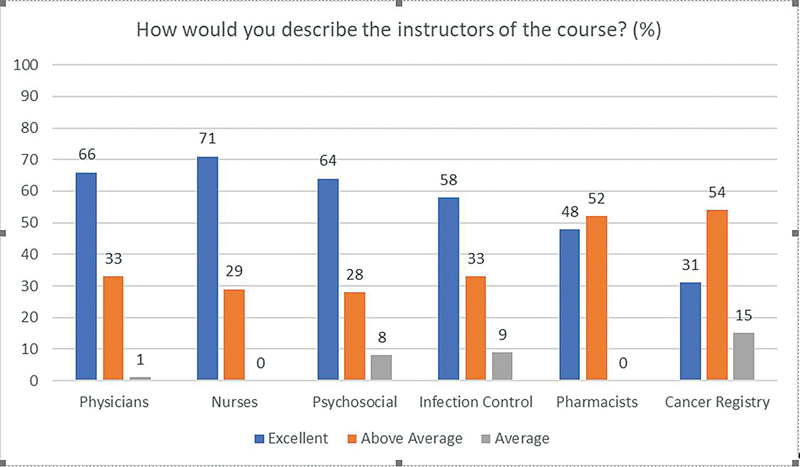
| Figure.2:Feedback responses (instructors).
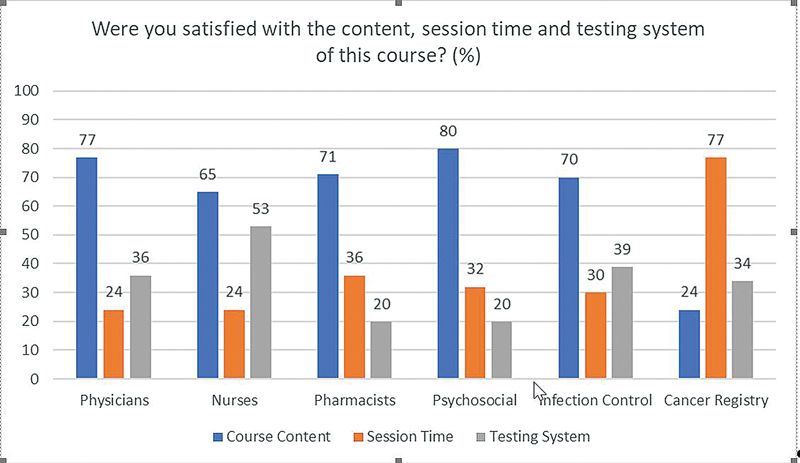
| Figure.3:Feedback responses (course satisfaction).
Secondary Outcomes
A total of 10 healthcare workers (6 data operators, 1 infection control practitioner and 3 psychologists) visited IHHN after attending the online course for hands-on training. A total of 1 week of practical observations and practice was conducted for each of these participants in a multidisciplinary environment. Each of these 10 participants has stayed connected to IHHN after training for mentorship and continued guidance in their practice.
Discussion
For years, tele-education has played a vital role in providing learning opportunities for rural and remote healthcare workers.[7] However, with the COVID-19 pandemic came a global prospect to innovate and implement quality online teaching methods with willing widespread acceptance.[7] Virtual education can be described as synchronous, that is, happening in real-time through chat rooms, or asynchronous that occurs without real-time interaction through prerecorded online channels.[8] Advantages of virtual education include flexibility of schedules, efficient use of time, accessibility from any location, exposure to national, and international faculties and worldwide distribution of knowledge and resources.[8] [9] [10] [11] For our pediatric oncology courses, a synchronous real-time teaching model was used to allow live interaction with participants. A large variety of individuals involved in pediatric oncologic care were able to connect and attend sessions from different cities and countries, saving expenditure on travel and accommodation.
The online form-based testing system was not as preferred by participants as reflected in the feedback form with only 36% (physicians), 53% (nurses), 20% (pharmacists), 20% (psychosocial), 39% (infection control), and 34% (cancer registry) satisfied with this testing method. When asked for open ended comments, most of these participants cited delays in connectivity and lack of technological expertise as reasons for this feedback. This resistance to adopt virtual teaching among participants reflects the environment prevailing in public institutes lacking resources. Most participants belonged to government hospitals and had to resort to using personal smartphones and mobile data to login to sessions.
Due to difficulty in synchronizing schedules, the convenience of the instructors was prioritized and a time slot was fixed in the afternoon. Most sessions were scheduled for 1 hour to avoid fatigue and redundancy and WhatsApp chat groups were created after each course for continued communication, mentorship, and learning. However, other than cancer registry participants, each course saw decreased satisfaction regarding session time in physicians (24%), nurses (24%), pharmacists (32%), psychosocial, and infection control (30%) courses. It was noted that the entire 1 hour was not used for teaching as coordination, mic, and slide sharing issues recurred in every session, reducing the content discussion time. Since physicians of every level were free to participate in the course, the level of questions and understanding varied, potentially contributing to the dissatisfaction with session time.
Recordings of lectures were shared with all participants immediately after the session along with the slides presented by the instructor. As techniques such as avoidance of cognitive overload and monitoring task completion times are effective in improving engagement in an online setting,[12] assessments and question and answer sessions were conducted after each module to increase participation and motivate individuals to engage in fruitful discussions. Unfortunately, increased engagement was not seen among participants as test completion rate was limited to 25% (physicians), 41% (nurses), 38% (pharmacists), 36% (psychosocial workers), 28% (infection control), and 52% (cancer registry). A possible reason for this was the lack of course fee; without monetary commitment participants did not hesitate to drop out and did not seem to prioritize the course as the organizers hoped.
Drawbacks of virtual education can be largely categorized into three groups: (1) technology and infrastructure barriers, (2) educators' barriers, and (3) learners' barriers.[11] With a drastic shift to online education, there has been an urgent need for instructors and learners to be well-versed in the use of technology. Investment in appropriate technological services is essential for teaching faculties to be well-equipped for efficient virtual learning and training and for continued education when face-to-face interactions are not feasible.[13] [14] Moreover, many professionals rely on free and reliable Wi-Fi services, access to which greatly varies according to economic class, especially in LMICs like Pakistan.[7] [15] A statistically significant difference has been observed between students of developed and developing countries, the former being better equipped and trained in virtual mediums of education.[16] To cater to the dearth of technological resources and infrastructure at the under-resourced public institutes partnered with IHHN, the MCM grant was used to provide teleconferencing equipment sets to remove barriers to national and international sessions for the local staff. However, despite consistent effort and assistance, many centers fall in areas where networks and connectivity remain a persistent issue causing disturbances while they attend sessions and attempt tests.
Connection with large audiences was a significant challenge for IHHN instructors. The attention and participation of individuals were difficult to gauge due to mics and cameras staying switched off, with exception of the cancer registry course that had the smallest number of participants. Many individuals claimed to have watched session recordings due to unavailability during working hours; however, there was no way to verify this. Therefore, it was decided to limit the number of participants per session for future virtual training courses.
For uniformity and improvement in targeted care, MCM centers and other institutions that look toward IHHN for mentorship in pediatric oncology services were engaged in online training sessions for specific tumor protocols. Case-based scenarios along with diagnosis, risk stratification, options in low-resource setting, treatments, and their complications were discussed in great detail while addressing queries from attendees. Assessment of the long-term impact of these focused sessions according to patient outcomes is currently under progress. In the face of digitalization, those who teach and have been taught using conventional, in-person methods are less familiar with virtual teaching methods and thus, more likely to face difficulties adapting.[17] In particular, laboratory-based courses, student placements, and field work have been adversely impacted and methods of assessments have required restructuring, requiring constantly learning and adjustments on the part of teachers and students alike.[18]
Online learning is particularly challenging for acquiring technical skills; for example, clinical training in medical professionals is better conducted hands-on.[16] Keeping this in mind, the focal person of each MCM-partnered unit was requested to identify key personnel in each discipline from their institutes. Select employees were offered travel and accommodation funds and invited for brief 1-week hands-on training opportunities in the infection control, data registry, and psychosocial departments at IHHN. These visits allowed better communication, practical observations, and improved execution of theoretical knowledge, while strict COVID-19 measures were observed. The aim of this process was to retain trained personnel long-term so that they can serve as trainers to other individuals once they return to their home institutes.
Since distance and in-person education both have distinct advantages and disadvantages, a middle-ground approach in the form of blended learning must be adopted.[19] Among medical and nursing students in Uganda, a 75% preference for blended learning was observed.[20] Similarly, a combination of online modules and subsequent practical assignments was proven to be successful in training medical personnel in an intensive care unit and emergency room in Germany.[21] A unique problem being faced in pediatric oncology in Pakistan is the lack of specialized training among physicians and nurses. Ranging from freshly graduated house officers and medical officers, pediatricians, medicine residents, and nurses with various certifications, most institutes have staff of diverse backgrounds responsible for childhood cancer patients. This is an additional challenge while designing teaching and training activities, further compounded by the fact that trained individuals often rotate indefinitely out of the service soon after attending the course. Since the courses for cancer registry, psycho-oncology, infection control, and pharmacy were spread over less than 12 hours, they would be considered workshops or web series rather than courses. The described courses were not certified from an educational institute, a limitation that IHHN is actively pursuing for the improvement in future courses. Despite the significant change in pre- and post-test averages seen in five courses, translation of this knowledge to patient care is a major challenge. Further studies are recommended for blended models along with innovative ways to engage and motivate healthcare workers of childhood cancer in low-resource settings.
Conclusion
Virtual teaching models will persist despite the trajectory of the COVID-19 pandemic due to their ease and accessibility. Enhancement of knowledge of healthcare workers engaged in paediatric oncology may be possible through virtual models and requires further study in low resource settings. Further studies regarding the impact of blended and virtual learning models and their effectiveness in pediatric oncology teaching and training are needed in a widespread manner to improve outcomes of childhood cancer.
Conflict of Interest
None declared.
Acknowledgments
We would like to acknowledge the contribution of the Departments of Nursing Education, Pharmacy, Infection Control, Electronic Medical Records (EMR), Psycho-Oncology and Drs. Sadia Muhammad and Ghulam Qadir Pathan for their hard work to execute these courses.
References
- Reporter T. 2021. '8,000 children diagnosed with cancer every year'. [online] DAWN.COM. Accessed May 6, 2022 at: https://www.dawn.com/news/1464231
- CPSP Z. 2021. College of Physicians and Surgeons Pakistan. [online] Cpsp.edu.pk. Accessed May 6, 2022 at: https://www.cpsp.edu.pk/accredited-institutes-fcps.php
- Ashraf M. (2021). Pediatric oncology nursing education initiatives at Children Cancer Hospital, Karachi, Pakistan; local problem –local solution. Accessed May 6, 2022 from https://ecommons.aku.edu/aku_symposium/2013_aeme/day1_op_efs/2/
- Uicc.org. 2021. World Cancer Declaration | UICC. [online] Accessed May 6, 2022 at: < https://www.uicc.org/what-we-do/advocacy/world-cancer-declaration
- Wijesooriya NR, Mishra V, Brand PLP, Rubin BK. COVID-19 and telehealth, education, and research adaptations. Paediatr Respir Rev 2020; 35: 38-42
- Pedrosa F, Shaikh F, Rivera G, Ribeiro R, Qaddoumi I. The impact of prospective telemedicine implementation in the management of childhood acute lymphoblastic leukemia in Recife, Brazil. Telemed J E Health 2017; 23 (10) 863-867
- Seymour-Walsh AE, Bell A, Weber A, Smith T. Adapting to a new reality: COVID-19 coronavirus and online education in the health professions. Rural Remote Health 2020; 20 (02) 6000 DOI: 10.22605/rrh6000.
- Kaup S, Jain R, Shivalli S, Pandey S, Kaup S. Sustaining academics during COVID-19 pandemic: the role of online teaching-learning. Indian J Ophthalmol 2020; 68 (06) 1220-1221
- Desai D, Sen S, Desai S, Desai R, Dash S. Assessment of online teaching as an adjunct to medical education in the backdrop of COVID-19 lockdown in a developing country - an online survey. Indian J Ophthalmol 2020; 68 (11) 2399-2403
- Mukhtar K, Javed K, Arooj M, Sethi A. Advantages, limitations and recommendations for online learning during COVID-19 pandemic era. Pak J Med Sci 2020; 36 (COVID19-S4): S27-S31
- Al-Balas M, Al-Balas HI, Jaber HM. et al. Distance learning in clinical medical education amid COVID-19 pandemic in Jordan: current situation, challenges, and perspectives. BMC Med Educ 2020; 20 (01) 341 DOI: 10.1186/s12909-020-02257-4.
- Jowsey T, Foster G, Cooper-Ioelu P, Jacobs S. Blended learning via distance in pre-registration nursing education: a scoping review. Nurse Educ Pract 2020; 44: 102775 DOI: 10.1016/j.nepr.2020.102775.
- Leal Filho W, Price E, Wall T. et al. COVID-19: the impact of a global crisis on sustainable development teaching. Environ Dev Sustain 2021; 23 (08) 11257-11278
- Gottschalk M, Werwick K, Albert C. et al. Digitalization of presence events in the COVID-19 pandemia - the lecturers' perspective. GMS J Med Educ 2021; 38 (01) Doc30 DOI: 10.3205/zma001426.
- Kruse C, Betancourt J, Ortiz S, Valdes Luna SM, Bamrah IK, Segovia N. Barriers to the use of mobile health in improving health outcomes in developing countries: systematic review. J Med Internet Res 2019; 21 (10) e13263 DOI: 10.2196/13263.
- Abbasi MS, Ahmed N, Sajjad B. et al. E-Learning perception and satisfaction among health sciences students amid the COVID-19 pandemic. Work 2020; 67 (03) 549-556
- Altwaijry N, Ibrahim A, Binsuwaidan R, Alnajjar LI, Alsfouk BA, Almutairi R. Distance education during COVID-19 pandemic: a college of pharmacy experience. Risk Manag Healthc Policy 2021; 14: 2099-2110
- Williams J. (2008). The Handbook of Blended Learning: Global Perspectives, Local Designs, by Curtis J. Bonk and Charles R. Graham (Eds.). San Francisco. CA: John Wiley and Sons 2006; 580 pages, hard cover. Academy Of Management Learning & Education, 7 (01) 132-133
- Lozano-Lozano M, Fernández-Lao C, Cantarero-Villanueva I. et al. A blended learning system to improve motivation, mood state, and satisfaction in undergraduate students: randomized controlled trial. J Med Internet Res 2020; 22 (05) e17101 DOI: 10.2196/17101.
- Olum R, Atulinda L, Kigozi E. et al. Medical education and e-learning during COVID-19 pandemic: awareness, attitudes, preferences, and barriers among undergraduate medicine and nursing students at Makerere University, Uganda. J Med Educ Curric Dev 2020; 7: 2382120520973212 DOI: 10.1177/2382120520973212.
- Jansen G, Latka E, Behrens F. et al. Hospital paramedic. An interprofessional blended learning concept to qualify paramedics and medical personnel for deployment in intensive care units and emergency departments during the COVID-19 pandemic. Anaesthesist 2021; 70 (01) 13-22
Address for correspondence
Publication History
Article published online:
02 July 2022
© 2022. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301
UP, India
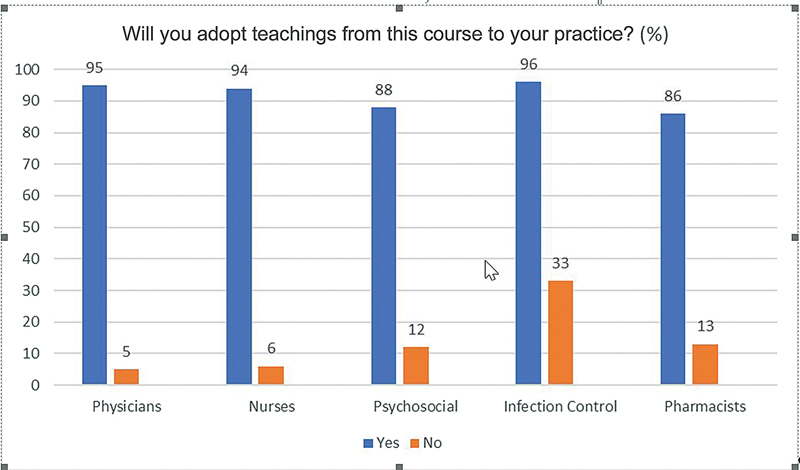
| Figure 1:Feedback responses (course teachings).
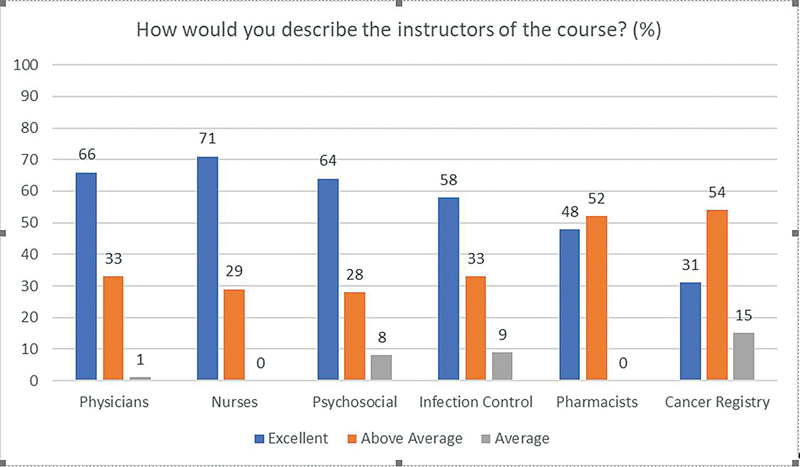
| Figure.2:Feedback responses (instructors).
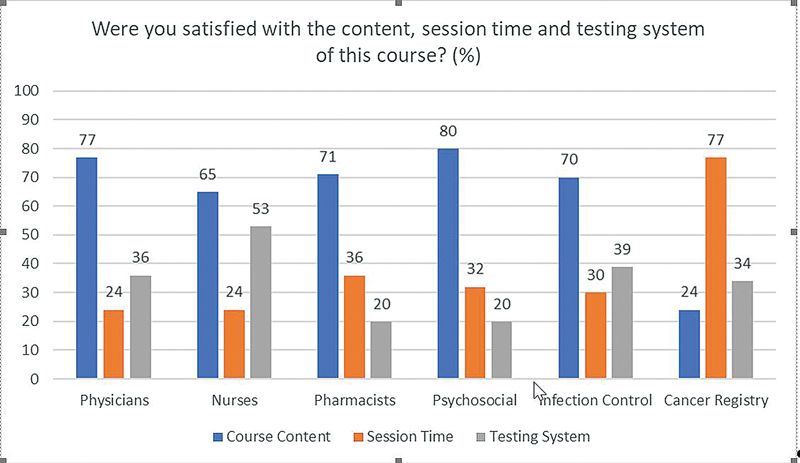
| Figure.3:Feedback responses (course satisfaction).
References
- Reporter T. 2021. '8,000 children diagnosed with cancer every year'. [online] DAWN.COM. Accessed May 6, 2022 at: https://www.dawn.com/news/1464231
- CPSP Z. 2021. College of Physicians and Surgeons Pakistan. [online] Cpsp.edu.pk. Accessed May 6, 2022 at: https://www.cpsp.edu.pk/accredited-institutes-fcps.php
- Ashraf M. (2021). Pediatric oncology nursing education initiatives at Children Cancer Hospital, Karachi, Pakistan; local problem –local solution. Accessed May 6, 2022 from https://ecommons.aku.edu/aku_symposium/2013_aeme/day1_op_efs/2/
- Uicc.org. 2021. World Cancer Declaration | UICC. [online] Accessed May 6, 2022 at: < https://www.uicc.org/what-we-do/advocacy/world-cancer-declaration
- Wijesooriya NR, Mishra V, Brand PLP, Rubin BK. COVID-19 and telehealth, education, and research adaptations. Paediatr Respir Rev 2020; 35: 38-42
- Pedrosa F, Shaikh F, Rivera G, Ribeiro R, Qaddoumi I. The impact of prospective telemedicine implementation in the management of childhood acute lymphoblastic leukemia in Recife, Brazil. Telemed J E Health 2017; 23 (10) 863-867
- Seymour-Walsh AE, Bell A, Weber A, Smith T. Adapting to a new reality: COVID-19 coronavirus and online education in the health professions. Rural Remote Health 2020; 20 (02) 6000 DOI: 10.22605/rrh6000.
- Kaup S, Jain R, Shivalli S, Pandey S, Kaup S. Sustaining academics during COVID-19 pandemic: the role of online teaching-learning. Indian J Ophthalmol 2020; 68 (06) 1220-1221
- Desai D, Sen S, Desai S, Desai R, Dash S. Assessment of online teaching as an adjunct to medical education in the backdrop of COVID-19 lockdown in a developing country - an online survey. Indian J Ophthalmol 2020; 68 (11) 2399-2403
- Mukhtar K, Javed K, Arooj M, Sethi A. Advantages, limitations and recommendations for online learning during COVID-19 pandemic era. Pak J Med Sci 2020; 36 (COVID19-S4): S27-S31
- Al-Balas M, Al-Balas HI, Jaber HM. et al. Distance learning in clinical medical education amid COVID-19 pandemic in Jordan: current situation, challenges, and perspectives. BMC Med Educ 2020; 20 (01) 341 DOI: 10.1186/s12909-020-02257-4.
- Jowsey T, Foster G, Cooper-Ioelu P, Jacobs S. Blended learning via distance in pre-registration nursing education: a scoping review. Nurse Educ Pract 2020; 44: 102775 DOI: 10.1016/j.nepr.2020.102775.
- Leal Filho W, Price E, Wall T. et al. COVID-19: the impact of a global crisis on sustainable development teaching. Environ Dev Sustain 2021; 23 (08) 11257-11278
- Gottschalk M, Werwick K, Albert C. et al. Digitalization of presence events in the COVID-19 pandemia - the lecturers' perspective. GMS J Med Educ 2021; 38 (01) Doc30 DOI: 10.3205/zma001426.
- Kruse C, Betancourt J, Ortiz S, Valdes Luna SM, Bamrah IK, Segovia N. Barriers to the use of mobile health in improving health outcomes in developing countries: systematic review. J Med Internet Res 2019; 21 (10) e13263 DOI: 10.2196/13263.
- Abbasi MS, Ahmed N, Sajjad B. et al. E-Learning perception and satisfaction among health sciences students amid the COVID-19 pandemic. Work 2020; 67 (03) 549-556
- Altwaijry N, Ibrahim A, Binsuwaidan R, Alnajjar LI, Alsfouk BA, Almutairi R. Distance education during COVID-19 pandemic: a college of pharmacy experience. Risk Manag Healthc Policy 2021; 14: 2099-2110
- Williams J. (2008). The Handbook of Blended Learning: Global Perspectives, Local Designs, by Curtis J. Bonk and Charles R. Graham (Eds.). San Francisco. CA: John Wiley and Sons 2006; 580 pages, hard cover. Academy Of Management Learning & Education, 7 (01) 132-133
- Lozano-Lozano M, Fernández-Lao C, Cantarero-Villanueva I. et al. A blended learning system to improve motivation, mood state, and satisfaction in undergraduate students: randomized controlled trial. J Med Internet Res 2020; 22 (05) e17101 DOI: 10.2196/17101.
- Olum R, Atulinda L, Kigozi E. et al. Medical education and e-learning during COVID-19 pandemic: awareness, attitudes, preferences, and barriers among undergraduate medicine and nursing students at Makerere University, Uganda. J Med Educ Curric Dev 2020; 7: 2382120520973212 DOI: 10.1177/2382120520973212.
- Jansen G, Latka E, Behrens F. et al. Hospital paramedic. An interprofessional blended learning concept to qualify paramedics and medical personnel for deployment in intensive care units and emergency departments during the COVID-19 pandemic. Anaesthesist 2021; 70 (01) 13-22


 PDF
PDF  Views
Views  Share
Share

