A Longitudinal Study to Reexamine the Mental Health Impact on Radiation Oncology Health Care Workers with the Launch of COVID-19 Vaccination Strategies in India
CC BY-NC-ND 4.0 · Indian J Med Paediatr Oncol 2022; 43(05): 415-423
DOI: DOI: 10.1055/s-0042-1755547
Abstract
Introduction The novel coronavirus disease 2019 (COVID-19) catastrophe caused significant mental threats to health care workers (HCW), especially during the first wave of the pandemic. India successfully implemented vaccination strategies in January 2021 that is likely to ameliorate the mental health impact of HCWs. The current survey aims to identify the change in impact following vaccination and address the issues affecting mental health.
Objective The primary objective is to reevaluate the stress levels of radiation oncology HCWs with vaccine implementation and compare it with the mental health status at the onset of the pandemic. The secondary objective is to identify the current causative factors influencing mental health.
Materials and Methods Health care workers who participated in the initial mental health impact survey at the outset of the COVID-19 pandemic from May to July 2020 were included in this study. Two hundred eligible HCWs were reassessed of the total 363 initial assessments. The 7-item Generalised Anxiety Disorder (GAD-7), 9-item Patient Health Questionnaire (PHQ-9), and 22-item Impact of Events Scale-revised (IES-R) was again served for assessing anxiety, depression, and posttraumatic stress disorder. The Mc Nemar test was used to evaluate the change and significance of the mental health impact. Univariate and multivariate analyses were done to identify the causative factors affecting mental health.
Results The cohort's median age was 30 years (interquartile range [IQR]: 27–33). The incidence of moderate-to-severe level anxiety, depression, and stress significantly declined to 6.5% (p = 0.031), 9% (p = 0.01), and 19% (p < 0.001) compared with 39.5, 40.5, and 30.5% during the pandemic onset. On further analysis, HCWs with affected family members had higher levels of stress (p = 0.002). The rest of the parameters did not have significant impact on mental health outcomes.
Conclusion With public education, awareness, and vaccination strategies, the second follow-up survey conducted after vaccine implementation demonstrated a significant number of HCWs in the radiation oncology community, exhibiting a decline in the incidence of anxiety, depression, and stress levels compared with the initial wave of the pandemic.
Keywords
mental health - radiation oncology - COVID-19 vaccination - anxiety - depression - stressPublication History
Article published online:
20 October 2022
© 2022. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
Abstract
Introduction The novel coronavirus disease 2019 (COVID-19) catastrophe caused significant mental threats to health care workers (HCW), especially during the first wave of the pandemic. India successfully implemented vaccination strategies in January 2021 that is likely to ameliorate the mental health impact of HCWs. The current survey aims to identify the change in impact following vaccination and address the issues affecting mental health.
Objective The primary objective is to reevaluate the stress levels of radiation oncology HCWs with vaccine implementation and compare it with the mental health status at the onset of the pandemic. The secondary objective is to identify the current causative factors influencing mental health.
Materials and Methods Health care workers who participated in the initial mental health impact survey at the outset of the COVID-19 pandemic from May to July 2020 were included in this study. Two hundred eligible HCWs were reassessed of the total 363 initial assessments. The 7-item Generalised Anxiety Disorder (GAD-7), 9-item Patient Health Questionnaire (PHQ-9), and 22-item Impact of Events Scale-revised (IES-R) was again served for assessing anxiety, depression, and posttraumatic stress disorder. The Mc Nemar test was used to evaluate the change and significance of the mental health impact. Univariate and multivariate analyses were done to identify the causative factors affecting mental health.
Results The cohort's median age was 30 years (interquartile range [IQR]: 27–33). The incidence of moderate-to-severe level anxiety, depression, and stress significantly declined to 6.5% (p = 0.031), 9% (p = 0.01), and 19% (p < 0.001) compared with 39.5, 40.5, and 30.5% during the pandemic onset. On further analysis, HCWs with affected family members had higher levels of stress (p = 0.002). The rest of the parameters did not have significant impact on mental health outcomes.
Conclusion With public education, awareness, and vaccination strategies, the second follow-up survey conducted after vaccine implementation demonstrated a significant number of HCWs in the radiation oncology community, exhibiting a decline in the incidence of anxiety, depression, and stress levels compared with the initial wave of the pandemic.
Keywords
Introduction
The novel coronavirus disease 2019 (COVID-19) pandemic, a catastrophic health crisis witnessed in the 21st century, had adversely affected mental health across the globe.[1] The relentless increase in the number of cases and the unpredictable nature of this pandemic had further exacerbated the public's psychological distress.[2] In India, more than 4.3 crore cases have been identified so far, with above 5.2 lakh COVID-19-related deaths.[3] [4] The psychological impact of COVID-19 on humanity makes it imperative to address issues concerning mental health with a degree of urgency.[5]
Although there is an acute shortage of health workforce, we have nearly 5.76 million health care workers (HCWs).[6] Mental stress had taken a toll on our HCWs during this critical period, affecting their professional and personal life. A few of the apparent reasons attributed were lengthy working hours, multiple shifts, risk of contracting the infection, transmitting it to family members back home, nonavailability of personal protective equipment (PPE), isolation, quarantine, and segregation from families.[7] In terms of availability of beds, our country has approximately 713,986 hospital beds across 25,778 hospitals in the government sector which is as low as 13.76 beds per 10,000 people.
During the first pandemic wave, more significant anxiety and panic was reported consequent to the rising number of fatalities and unavailability of a vaccine. Various studies were conducted on the deteriorating mental health condition of HCWs. HCWs from oncology and, especially, branches like radiation oncology, have more frequent contact and exposure to the patients due to the fractionated and prolonged course of treatment. A multinational study conducted in India from May 2020 to July 2020 with 758 participants of the radiation oncology fraternity, comprising various Asian countries revealed significant anxiety, depression, and stress levels s in HCWs.[8]
With the rising number of cases and deaths, the public, including HCWs, was apprehensive about contracting the infection and the possibility of a next wave. The beginning of 2021 witnessed the approval of vaccines to fight the pandemic that had caused untold misery and deaths across the globe.[9] However, around 20 to 30% of the population were also apprehensive about the vaccine's side effects.[10] India inaugurated its vaccination drive program on January 16, 2021.[11] Two vaccines were approved, the Covaxin which is an inactivated viral vaccine and Covishield which uses the viral vector platform. The country expedited its vaccination drive on a war footing, and 1 billion cumulative vaccine doses were administered by October 21, 2021.[12] This remarkable achievement was possible due to continued efforts from government agencies, vaccine manufacturers, and HCWs.
The ongoing vaccination drive, the resultant decrease in the severity of infections, and a marked fall in death rates are likely to have boosted the morale of most of our HCWs. On the other hand, the public was also apprehensive about the shortage of vaccines, their effectiveness, side effects, and the possibility of a second pandemic wave. We could see that a proportion of them was still unable to cope with the stress despite continued awareness and vaccine implementation. Hence, our study aimed to evaluate the change in the mental health status of radiation oncology HCWs following the mass vaccination drive in India and compare it with that at the beginning of the pandemic and identify the various causative factors negatively impacting their mental health.
Materials and Methods
This longitudinal study was conducted as a continuation of the survey done during the onset of the pandemic to reexplore the mental health status of HCWs with the advent of vaccine implementation strategies. The initial assessment from various Asian countries was published earlier this year.[8] The data collection variables included demographic profile, history of COVID-19 contact, testing, and infection with vaccination status. Responses of the mental health assessment tools were analyzed. The case record form with all data variables is given in the [Supplementary Material S1] (available in the online version).
Participants
The mental health status of radiation oncology HCWs from four tertiary cancer care centers in India was assessed from January 2021 to May 2021. This period was chosen because the first wave of the pandemic was tailing down, and vaccination strategies for HCWs were just implemented and slowly picking up across the country. Participants were requested to fill out the survey via a google form. Three reminders were sent for completing the survey, and each question was marked mandatory to avoid missing data. The closure date for the response to the survey was fixed as May 10, 2021.
Inclusion and Exclusion Criteria
Our study included radiation oncology HCWs from India who filled the survey at the pandemic onset, aged 18 years and above. There was no cut-off for the upper age limit. The participants included radiation oncology clinicians, physicists, technologists, nurses, and allied workers. Participants who did not participate in the initial survey were excluded.
Data Collection
Of the 363 Indian participants who participated in the initial survey, 200 responses were received, forming the study sample for the current analysis. [Supplementary Fig. S1] (available in the online version) represents the number of participants evaluated during the first and second surveys. The demographic profile, including a history of vaccination status, was documented. The 7-item Generalised Anxiety Disorder (GAD-7), 9-item Patient Health Questionnaire (PHQ-9), and 22-item Impact of Events Scale-revised (IES-R) was again utilized for assessing anxiety, depression, and posttraumatic stress disorder. Univariate and multivariate analysis was done to identify the causative factors affecting mental health. No subgroup analysis was performed. For GAD-7, scores 0 to 4 represent minimal, 5 to 9 mild, 10 to 14 moderate, and 15 to 21 severe anxiety. For PHQ-9, scores 0 to 4 represent none, 5 to 9 mild, 10 to 14 moderate, 15 to 19 moderately severe, and 20 to 27 severe depression. For IES-R scores from 0 to 88, a total score of 24 or more for posttraumatic stress disorder is a clinical concern.[13] [14]
Statistical Analysis
Statistical Package for Social Sciences software, Version 25, was utilized for data analysis. The McNemar test was used to evaluate the change and significance of the mental health impact. Important causative factors for anxiety, depression, and stress were analyzed. Significant factors were entered into a multivariate Cox's proportional hazards model and expressed as hazard ratio (HR) with a 95% confidence interval (CI). A p-value of ≤0.05 was considered statistically significant.
Ethics
Tata Memorial Centre Institutional Ethics Committee approval was taken (project no: 3482, dated: May 13, 2020), and Clinical Trial Registry of India registration (CTRI no.: 2020/05/025212) was done before the initiation of the study. Informed consent was obtained from all participants. The procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1964, as revised in 2013.
Results
A total of 200 participants were assessed again for anxiety, depression, and stress. It was observed that 108 (54%) were married, 103 (51.5%) aged above 50 years, and 105 (52.5%) had less than three rooms in the household. Comorbidities were present in 26 (13%) participants. Among all the participants, 93 (46.5%) were physicians and 197 (98.5%) of HCWs had above secondary education. [Table 1] shows the demographic profile of the participants.
|
Participants |
n = 200 |
||
|---|---|---|---|
|
Median age [IQR] in years |
30 |
[27–33] |
|
|
n |
% |
||
|
Gender |
Female |
87 |
43.5 |
|
Male |
113 |
56.5 |
|
|
Marital status |
Divorced or separated |
1 |
0.5 |
|
Married |
108 |
54.0 |
|
|
Single |
91 |
45.5 |
|
|
Number of rooms in the household |
<3> |
105 |
52.5 |
|
≥3 |
95 |
47.5 |
|
|
Children less than 15 years |
0 |
135 |
67.5 |
|
1 |
44 |
22.0 |
|
|
≥2 |
21 |
10.5 |
|
|
Age more than 50 years |
No |
97 |
48.5 |
|
Yes |
103 |
51.5 |
|
|
Occupation |
Administrator |
3 |
1.5 |
|
Allied health care worker |
20 |
10.0 |
|
|
Nurse |
4 |
2.0 |
|
|
Physician |
93 |
46.5 |
|
|
Physicist/therapist |
80 |
40.0 |
|
|
Cadre |
Junior staff (<10> |
124 |
62.0 |
|
Senior staff (>10 years' experience) |
26 |
13.0 |
|
|
Student |
50 |
25.0 |
|
|
Comorbidities |
No |
174 |
87.0 |
|
Yes |
26 |
13.0 |
|
|
History of smoking or tobacco use |
No |
191 |
95.5 |
|
Yes |
7 |
3.5 |
|
|
Do not want to disclose |
2 |
1.0 |
|
|
Educational qualification |
Above secondary |
197 |
98.5 |
|
Below secondary |
3 |
1.5 |
|
|
n (200) |
% |
||
|---|---|---|---|
|
Close contact |
No |
40 |
20.0 |
|
Yes |
160 |
80.0 |
|
|
Place of Contact |
Society |
13 |
8.1 |
|
Workplace |
138 |
86.3 |
|
|
Other |
9 |
5.6 |
|
|
Testing for COVID-19 |
No |
87 |
43.5 |
|
Yes |
113 |
56.5 |
|
|
COVID-19 positive |
No |
171 |
85.5 |
|
Yes |
29 |
14.5 |
|
|
Weeks for recovery |
2 to 4 |
27 |
93.1 |
|
4 to 6 |
2 |
6.9 |
|
|
Family members contracted COVID-19 |
No |
154 |
77.0 |
|
Yes |
46 |
23.0 |
|
|
HCW and family +ve |
Yes |
6/46 |
13 |
|
Vaccination facility |
No |
48 |
24.0 |
|
Yes |
152 |
76.0 |
|
|
Volunteering to get vaccinated |
No |
55 |
27.5 |
|
Yes |
145 |
72.5 |
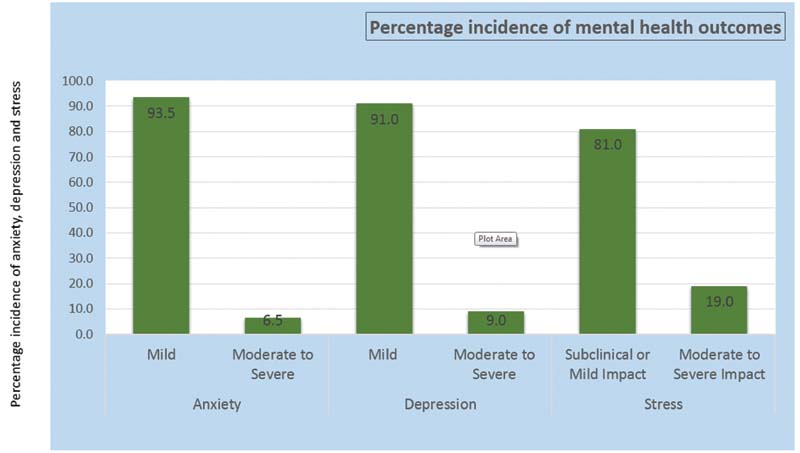
| Figure 1:Percentage incidence of mental health outcomes during second survey.
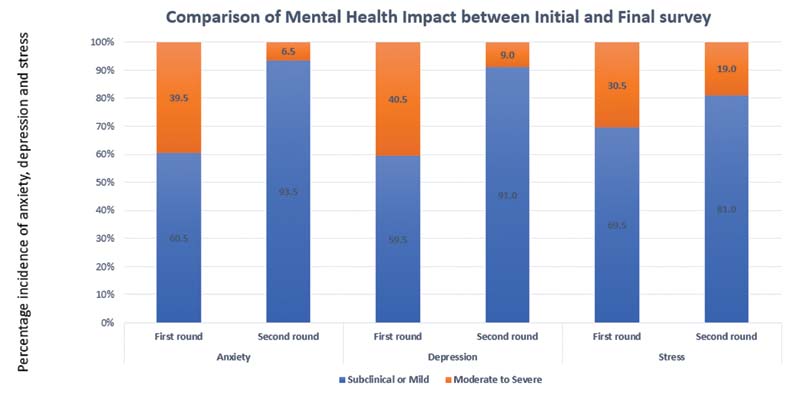
| Figure 2:Comparison of mental health impact between initial and final survey.
Univariate analysis was done to assess the factors which determine anxiety, depression, and stress levels. It was seen that none of the factors was significant for anxiety and depression among all. However, for stress levels, COVID-19 infection among family members significantly contributed to increased stress levels (p = 0.002). [Table 3] shows the univariate analysis for stress. The tables of univariate analysis for anxiety and depression are shown in the [Supplementary Tables 1] and [2] (available in the online version).
|
Variables to assess the change in impact |
Mild Impact (n = 162) n (%) |
Mild-to-severe Impact (n = 38) n (%) |
p-Value |
|
|---|---|---|---|---|
|
Median age [IQR] in years |
29.5 [27–33] |
30 [28–34.25] |
0.118 |
|
|
Gender |
Female |
72 (82.8) |
15 (17.2) |
0.578 |
|
Male |
90 (79.6) |
23 (20.4) |
||
|
Marital status |
Divorced or separated |
1 (100.0) |
0 (0.0) |
0.881 |
|
Married |
87 (80.6) |
21 (19.4) |
||
|
Single |
74 (81.3) |
17 (18.7) |
||
|
No. of rooms in household |
<3> |
87 (82.9) |
18 (17.1) |
0.482 |
|
≥3 |
75 (78.9) |
20 (21.1) |
||
|
Children in the house <15> |
0 |
110 (81.5) |
25 (18.5) |
0.837 |
|
1 |
36 (81.8) |
8 (18.2) |
||
|
2 |
16 (76.2) |
5 (23.8) |
||
|
Adults >50 years |
0 |
84 (86.6) |
13 (13.4) |
0.05 |
|
≥1 |
78 (75.7) |
25 (24.3) |
||
|
Occupation |
Administrator |
3 (100.0) |
0 (0.0) |
0.437 |
|
Allied health care worker |
19 (95.0) |
1 (5.0) |
||
|
Nurse |
3 (75.0) |
1 (25.0) |
||
|
Physician |
73 (78.5) |
20 (21.5) |
||
|
Physicist/therapist |
64 (80.0) |
16 (20.0) |
||
|
Cadre |
Junior staff |
98 (79.0) |
26 (21.0%) |
0.335 |
|
Senior staff |
20 (76.9) |
6 (23.1) |
||
|
Student |
44 (88.0) |
6 (12.0) |
||
|
Comorbidities |
No |
140 (80.5) |
34 (19.5) |
0.791 |
|
Yes |
22 (84.6) |
4 (15.4) |
||
|
Smoking |
No |
154 (80.6) |
37 (19.4) |
0.746 |
|
Yes |
6 (85.7) |
1 (14.3) |
||
|
Do not want to disclose |
2 (100.0) |
0 (0.0) |
||
|
Educational qualification |
Above secondary |
161 (81.7) |
36 (18.3) |
0.093 |
|
Below secondary |
1 (33.3) |
2 (66.7) |
||
|
Close contact |
No |
33 (82.5) |
7 (17.5) |
0.787 |
|
Yes |
129 (80.6) |
31 (19.4) |
||
|
COVID-19 testing |
No |
71 (81.6) |
16 (18.4) |
0.847 |
|
Yes |
91 (80.5) |
22 (19.5) |
||
|
COVID-19 positivity |
No |
139 (81.3) |
32 (18.7) |
0.802 |
|
Yes |
23 (79.3) |
6 (20.7) |
||
|
COVID-19 in family members |
No |
132 (85.7) |
22 (14.3) |
0.002 |
|
Yes |
30 (65.2) |
16 (34.8) |
||
|
Vaccination facility |
No |
35 (72.9) |
13 (27.1) |
0.102 |
|
Yes |
127 (83.6) |
25 (16.4) |
||
|
Volunteering for Vaccine |
No |
43 (78.2) |
12 (21.8) |
0.532 |
|
Yes |
119 (82.1) |
26 (17.9) |
||
|
Longer period of isolation |
||||
References
- Xiong J, Lipsitz O, Nasri F. et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J Affect Disord 2020; 277: 55-64
- Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet 2020; 395 (10224): e37-e38
- No third wave yet, surge in cases continuation of the second one, say experts. . Accessed October 24, 2021 at: https://economictimes.indiatimes.com/news/india/no-third-wave-yet-surge-in-cases-is-continuation-of-the-second-one/articleshow/85082048.cms
- Das KN. India “prepares for the worst” ahead of possible COVID-19 third wave. . Accessed October 24, 2021 at: https://www.reuters.com/world/the-great-reboot/india-prepares-worst-ahead-possible-covid-19-third-wave-2021-09-07/
- World Health Organization. World Mental Health Report: transforming mental health for all. Accessed October 24, 2021 at: https://www.who.int/teams/mental-health-and-substance-use/
- Karan A, Negandhi H, Hussain S. et al. Size, composition and distribution of health workforce in India: why, and where to invest?. Hum Resour Health 2021; 19 (01) 39
- Kang L, Li Y, Hu S. et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry 2020; 7 (03) e14
- Wadasadawala T, Kumar A, Laskar SG. et al. Multinational study to assess stress levels among the health care workers of radiation oncology community at the outset of the COVID-19 pandemic. JCO Glob Oncol 2021; 7: 464-473
- World Health Organization. COVID-19 vaccines. Accessed October 24, 2021 at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-vaccines
- Dodd RH, Cvejic E, Bonner C, Pickles K, McCaffery KJ. Sydney Health Literacy Lab COVID-19 group. Willingness to vaccinate against COVID-19 in Australia. Lancet Infect Dis 2021; 21 (03) 318-319 DOI: 10.1016/S1473-3099(20)30559-4.
- Perappadan BS. Coronavirus. First phase of vaccination to start on January 16. Accessed October 24, 2021 at: https://www.thehindu.com/news/national/india-to-start-covid-19-vaccination-drive-on-jan-16/article33536670.ece
- Total vaccination. Accessed October 24, 2021 at: https://www.mohfw.gov.in/
- Creamer M, Bell R, Failla S. Psychometric properties of the Impact of Event Scale - revised. Behav Res Ther 2003; 41 (12) 1489-1496
- Kawamura N, Kim Y, Asukai N. Suppression of cellular immunity in men with a past history of posttraumatic stress disorder. Am J Psychiatry 2001; 158 (03) 484-486
- The implications of COVID-19 for mental health and substance use. Accessed October 24, 2021 at: https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/
- Mehta S, Machado F, Kwizera A. et al. COVID-19: a heavy toll on health-care workers. Lancet Respir Med 2021; 9 (03) 226-228
- Roy A, Singh AK, Mishra S, Chinnadurai A, Mitra A, Bakshi O. Mental health implications of COVID-19 pandemic and its response in India. Int J Soc Psychiatry 2021; 67 (05) 587-600
- Ranganathan P, Sengar M, Chinnaswamy G. et al; National Cancer Grid of India. Impact of COVID-19 on cancer care in India: a cohort study. Lancet Oncol 2021; 22 (07) 970-976
- Pramesh CS, Badwe RA. Cancer management in India during COVID-19. N Engl J Med 2020; 382 (20) e61 DOI: 10.1056/NEJMc2011595.
- Sharma DC. Lockdown poses new challenges for cancer care in India. Lancet Oncol 2020; 21 (07) 884
- Shrikhande SV, Pai PS, Bhandare MS. et al; all collaborators from Department of Surgical Oncology. Outcomes of elective major cancer surgery during COVID 19 at Tata Memorial Centre: implications for cancer care policy. Ann Surg 2020; 272 (03) e249-e252
- Mukherji A, Gupta T, Agarwal JP. Time, distance, shielding and ALARA; drawing similarities between measures for radiation protection and Coronavirus disease pandemic response. Indian J Cancer 2020; 57 (02) 221-223
- ;Comirnaty and Pfizer-BioNTech COVID-19 vaccine. Accessed October 24, 2021 at: https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/pfizer-biontech-covid-19-vaccine
- Asia-Pacific Roundup: India approves AstraZeneca, Bharat Biotech COVID vaccines. Accessed October 24, 2021 at: https://www.raps.org/news-and-articles/news-articles/2021/1/asia-pacific-roundup-india-approves-astrazeneca-bh
- Oxford-AstraZeneca vaccine: what to know about side effects. Accessed October 24, 2021 at: https://www.medicalnewstoday.com/articles/oxford-astrazeneca-vaccine-what-to-know-about-side-effects
- COVID-19 vaccination: 4 new side-effects of the Covishield vaccine that you should not ignore. Accessed October 24, 2021 at: https://www.dnaindia.com/health/report-4-new-side-effects-of-covishield-vaccine-that-you-should-not-ignore-oxford-astrazeneca-covid-19-vaccination-2910701
- Sanderson K. COVID vaccines protect against Delta, but their effectiveness wanes. Nature 2021; (e-pub ahead of print). DOI: 10.1038/d41586-021-02261-8.
- COVID19-India. Accessed October 24, 2021 at: https://www.covid19india.org/
- Perez-Arce F, Angrisani M, Bennett D, Darling J, Kapteyn A, Thomas K. COVID-19 vaccines and mental distress. PLoS One 2021; 16 (09) e0256406
- Singh GP, Jaswal S. COVID vaccination and mental health: An Indian perspective. Asian J Psychiatr 2022; 67: 102950
- Koltai J, Raifman J, Bor J, McKee M, Stuckler D. COVID-19 vaccination and mental health: a difference-in-difference analysis of the understanding America study. Am J Prev Med 2022; 62 (05) 679-687
- Xiang YT, Yang Y, Li W. et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 2020; 7 (03) 228-229
- Wang G, Zhang Y, Zhao J, Zhang J, Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet 2020; 395 (10228): 945-947
- Bhanot D, Singh T, Verma SK, Sharad S. Stigma and discrimination during COVID-19 pandemic. Front Public Health 2021; 8: 577018
Address for correspondence
Jai P. Agarwal, MDDepartment of Radiation Oncology, Tata Memorial Centre, Homi Bhabha National InstituteMumbai, Maharashtra 400012IndiaEmail: agarwal.jp@tmc.gov.inPublication History
Article published online:
20 October 2022© 2022. Indian Society of Medical and Paediatric Oncology. This is an open access article published by Thieme under the terms of the Creative Commons Attribution-NonDerivative-NonCommercial License, permitting copying and reproduction so long as the original work is given appropriate credit. Contents may not be used for commercial purposes, or adapted, remixed, transformed or built upon. (https://creativecommons.org/licenses/by-nc-nd/4.0/)
Thieme Medical and Scientific Publishers Pvt. Ltd.
A-12, 2nd Floor, Sector 2, Noida-201301 UP, India
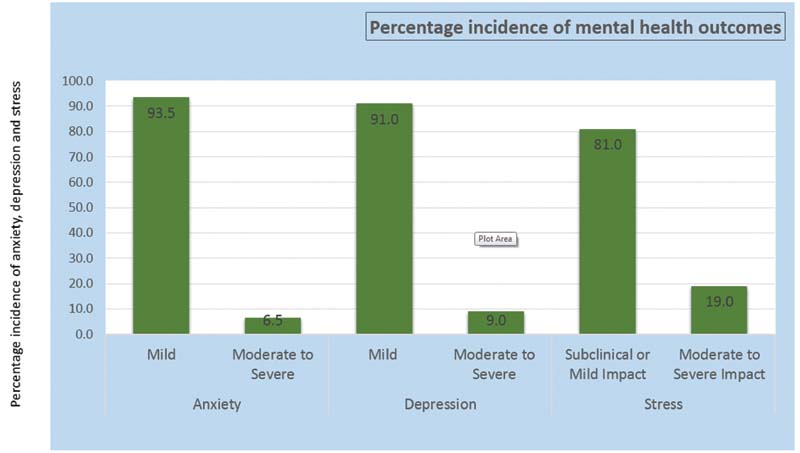
| Figure 1:Percentage incidence of mental health outcomes during second survey.
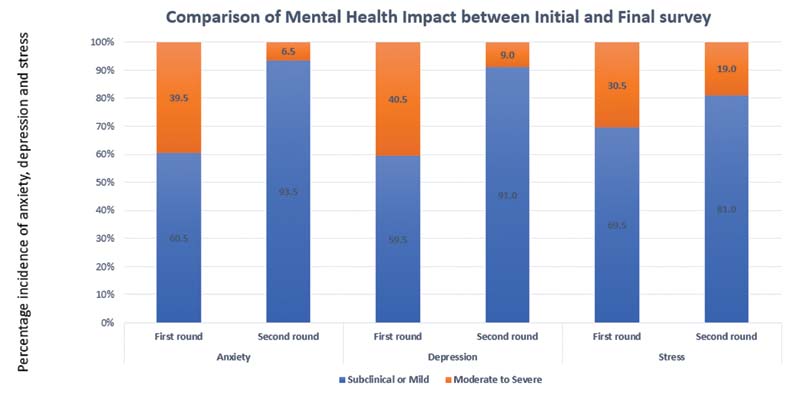
| Figure 2:Comparison of mental health impact between initial and final survey.
References
- Xiong J, Lipsitz O, Nasri F. et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J Affect Disord 2020; 277: 55-64
- Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet 2020; 395 (10224): e37-e38
- No third wave yet, surge in cases continuation of the second one, say experts. . Accessed October 24, 2021 at: https://economictimes.indiatimes.com/news/india/no-third-wave-yet-surge-in-cases-is-continuation-of-the-second-one/articleshow/85082048.cms
- Das KN. India “prepares for the worst” ahead of possible COVID-19 third wave. . Accessed October 24, 2021 at: https://www.reuters.com/world/the-great-reboot/india-prepares-worst-ahead-possible-covid-19-third-wave-2021-09-07/
- World Health Organization. World Mental Health Report: transforming mental health for all. Accessed October 24, 2021 at: https://www.who.int/teams/mental-health-and-substance-use/
- Karan A, Negandhi H, Hussain S. et al. Size, composition and distribution of health workforce in India: why, and where to invest?. Hum Resour Health 2021; 19 (01) 39
- Kang L, Li Y, Hu S. et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry 2020; 7 (03) e14
- Wadasadawala T, Kumar A, Laskar SG. et al. Multinational study to assess stress levels among the health care workers of radiation oncology community at the outset of the COVID-19 pandemic. JCO Glob Oncol 2021; 7: 464-473
- World Health Organization. COVID-19 vaccines. Accessed October 24, 2021 at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-vaccines
- Dodd RH, Cvejic E, Bonner C, Pickles K, McCaffery KJ. Sydney Health Literacy Lab COVID-19 group. Willingness to vaccinate against COVID-19 in Australia. Lancet Infect Dis 2021; 21 (03) 318-319 DOI: 10.1016/S1473-3099(20)30559-4.
- Perappadan BS. Coronavirus. First phase of vaccination to start on January 16. Accessed October 24, 2021 at: https://www.thehindu.com/news/national/india-to-start-covid-19-vaccination-drive-on-jan-16/article33536670.ece
- Total vaccination. Accessed October 24, 2021 at: https://www.mohfw.gov.in/
- Creamer M, Bell R, Failla S. Psychometric properties of the Impact of Event Scale - revised. Behav Res Ther 2003; 41 (12) 1489-1496
- Kawamura N, Kim Y, Asukai N. Suppression of cellular immunity in men with a past history of posttraumatic stress disorder. Am J Psychiatry 2001; 158 (03) 484-486
- The implications of COVID-19 for mental health and substance use. Accessed October 24, 2021 at: https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/
- Mehta S, Machado F, Kwizera A. et al. COVID-19: a heavy toll on health-care workers. Lancet Respir Med 2021; 9 (03) 226-228
- Roy A, Singh AK, Mishra S, Chinnadurai A, Mitra A, Bakshi O. Mental health implications of COVID-19 pandemic and its response in India. Int J Soc Psychiatry 2021; 67 (05) 587-600
- Ranganathan P, Sengar M, Chinnaswamy G. et al; National Cancer Grid of India. Impact of COVID-19 on cancer care in India: a cohort study. Lancet Oncol 2021; 22 (07) 970-976
- Pramesh CS, Badwe RA. Cancer management in India during COVID-19. N Engl J Med 2020; 382 (20) e61 DOI: 10.1056/NEJMc2011595.
- Sharma DC. Lockdown poses new challenges for cancer care in India. Lancet Oncol 2020; 21 (07) 884
- Shrikhande SV, Pai PS, Bhandare MS. et al; all collaborators from Department of Surgical Oncology. Outcomes of elective major cancer surgery during COVID 19 at Tata Memorial Centre: implications for cancer care policy. Ann Surg 2020; 272 (03) e249-e252
- Mukherji A, Gupta T, Agarwal JP. Time, distance, shielding and ALARA; drawing similarities between measures for radiation protection and Coronavirus disease pandemic response. Indian J Cancer 2020; 57 (02) 221-223
- ;Comirnaty and Pfizer-BioNTech COVID-19 vaccine. Accessed October 24, 2021 at: https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/pfizer-biontech-covid-19-vaccine
- Asia-Pacific Roundup: India approves AstraZeneca, Bharat Biotech COVID vaccines. Accessed October 24, 2021 at: https://www.raps.org/news-and-articles/news-articles/2021/1/asia-pacific-roundup-india-approves-astrazeneca-bh
- Oxford-AstraZeneca vaccine: what to know about side effects. Accessed October 24, 2021 at: https://www.medicalnewstoday.com/articles/oxford-astrazeneca-vaccine-what-to-know-about-side-effects
- COVID-19 vaccination: 4 new side-effects of the Covishield vaccine that you should not ignore. Accessed October 24, 2021 at: https://www.dnaindia.com/health/report-4-new-side-effects-of-covishield-vaccine-that-you-should-not-ignore-oxford-astrazeneca-covid-19-vaccination-2910701
- Sanderson K. COVID vaccines protect against Delta, but their effectiveness wanes. Nature 2021; (e-pub ahead of print). DOI: 10.1038/d41586-021-02261-8.
- COVID19-India. Accessed October 24, 2021 at: https://www.covid19india.org/
- Perez-Arce F, Angrisani M, Bennett D, Darling J, Kapteyn A, Thomas K. COVID-19 vaccines and mental distress. PLoS One 2021; 16 (09) e0256406
- Singh GP, Jaswal S. COVID vaccination and mental health: An Indian perspective. Asian J Psychiatr 2022; 67: 102950
- Koltai J, Raifman J, Bor J, McKee M, Stuckler D. COVID-19 vaccination and mental health: a difference-in-difference analysis of the understanding America study. Am J Prev Med 2022; 62 (05) 679-687
- Xiang YT, Yang Y, Li W. et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 2020; 7 (03) 228-229
- Wang G, Zhang Y, Zhao J, Zhang J, Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet 2020; 395 (10228): 945-947
- Bhanot D, Singh T, Verma SK, Sharad S. Stigma and discrimination during COVID-19 pandemic. Front Public Health 2021; 8: 577018


 PDF
PDF  Views
Views  Share
Share

